Does Gout Cause Bone Erosion
The factors most significantly associated with bone erosion were duration of gout, age, synovial hypertrophy, and presence and number of tophi. A high percentage of patients with gout have bone erosions, most frequently in the first metatarsophalangeal joint, according to a study published in Arthritis Care & Research.
Also Check: Can You Have Both Psoriatic Arthritis And Rheumatoid Arthritis
Difference In Treatments For Ra Vs Arthritis
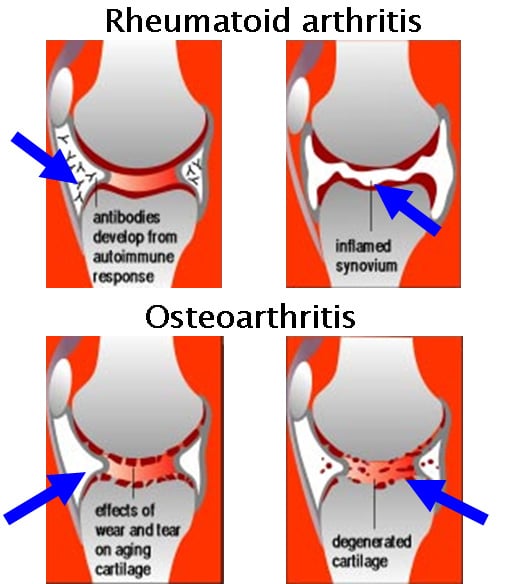
Because the cause of RA is different than other types of arthritis, like osteoarthritis, it makes sense that will differ as well. One big difference? There are a lot more treatment options for RA. When I see a patient for the first time, and I am trying to diagnose what is the cause of their joint pain, I am happier to diagnose them with rheumatoid arthritis than I am with osteoarthritis because we have such good medical therapies for rheumatoid arthritis, says Dr. Blank. For osteoarthritis, she adds, we don’t have anything that can halt the progression of the diseaseall we can do is treat the pain.
Treatments for RA include disease-modifying-anti-rheumatic-drugs , which work by suppressing the immune system and therefore reducing inflammation in your joints, slowing the progression of the disease. The recommendation is to start something like methotrexate for moderate to high disease severity, says Dr. Sharmeen. If over time, thats not enough, well add on another treatment such as biologic drug.
Biologics are drugs that target specific immune proteins that cause inflammation. There are several different options here, including:
-
tumor necrosis factor inhibitors which targets tumor necrosis factor, a substance people with RA make in excess
-
B-cell inhibitors which home in on inflammation-causing lymphocytes
-
T-cell inhibitors which target immune T-cells
-
Interleukin inhibitors which stop specific proteins from attaching to cells and causing inflammation
What Is An Endoscopy
An endoscopy is a procedure that involves the use of an instrument called an endoscope a thin, flexible tube with a small camera attached to one end.
It allows a doctor to work inside your body without a traditional surgical incision. The doctor can insert the endoscope via an opening in the body, such as the mouth, or through a small incision.
Once inserted, the camera allows the doctor to visually examine specific organs, blood vessels, muscles, or bones. The doctor can then use small instruments attached to the endoscope to remove tissue or perform surgical procedures.
Recommended Reading: What Is The Best Medicine To Take For Rheumatoid Arthritis
Clinical Characteristics Of Ra And Psa
For RA, the American College of Rheumatology /European League Against Rheumatism classification criteria were designed for patient characterisation and use in clinical trials. The key clinical characteristic is the confirmation of definite, persistent, clinical synovitis in at least one joint. The criteria include the number of joints involved, duration of symptoms, and the demonstration of serological markers and an elevated acute-phase reactant. For PsA, the Classification Criteria for Psoriatic Arthritis help categorise patients with inflammatory articular disease for clinical trials. Key clinical characteristics include a personal or family history of psoriasis, psoriatic nail dystrophy and dactylitis. Neither classification criteria should be confused as diagnostic criteria.
Joint involvement is predominantly symmetric in RA and often, but not always, asymmetric in PsA. In both RA and PsA, most patients have polyarthritis , although joint involvement can be oligoarticular or polyarticular. Monoarticular disease is less common in PsA however, 5%10% of patients may present with isolated distal joint involvement. In PsA, prognosis worsens and symmetry of joint involvement tends to increase as the number of affected joints increases.
How Psoriatic Arthritis Differs From Rheumatoid Arthritis
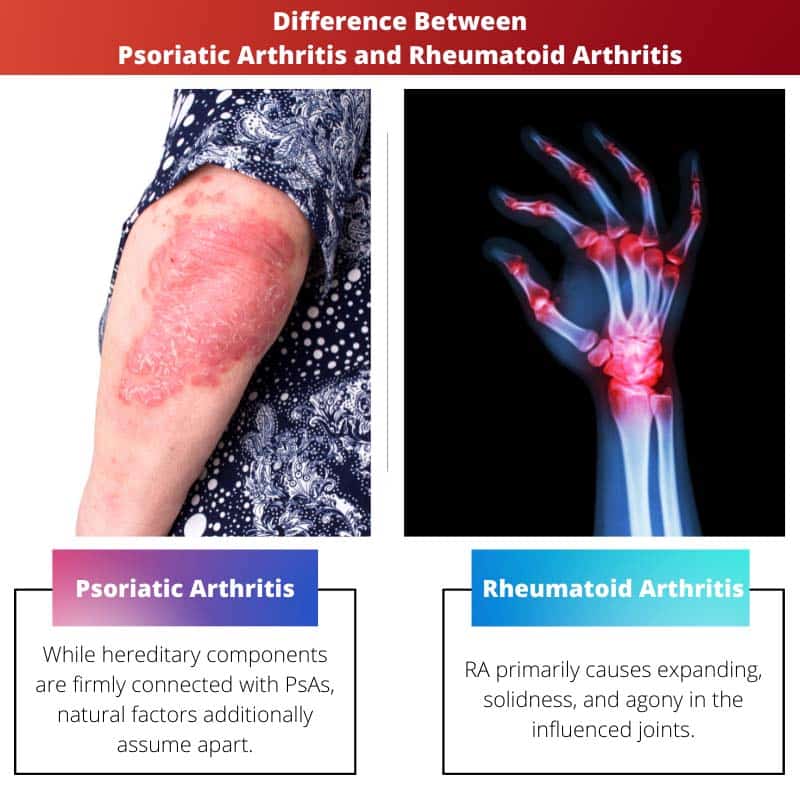
Rheumatoid arthritis is also a chronic autoimmune disease. Youre more likely to develop rheumatoid arthritis if you have a family history of RA. People over age 40 and women are also more at risk.
Experts havent pinpointed the exact cause of rheumatoid arthritis yet, but we do know that your bodys antibodies attack the joints if you have this condition. Typically, it affects the smaller joints first–the small joints in the hands, feet and wrists. It causes swelling, pain and stiffness in these joints.
So what makes it different from psoriatic arthritis? It can be tough to determine without bloodwork, as there can be some overlap with the joints that both kinds can affect, notes Bauer. For example, both can affect the hips and knees, Bauer says.
Related: How to Keep Your Joints Healthy
If your doctor suspects you have rheumatoid arthritis, you may need to undergo some blood tests to look for high levels of inflammation and for specific antibodies that are commonly found in the bloodstreams of people with RA. , the doctors will be looking for evidence of an antibody called the Rheumatoid Factor antigen and perhaps also cyclic citrullinated peptide antibodies .
However, there are two things that might help you distinguish the two types of arthritis from each other. One is fairly obvious: the presence of psoriasis lesions. Thats a cue that youre probably dealing with psoriatic arthritis.
Read Also: Can Psoriatic Arthritis Cripple You
What Are The Symptoms Of Ra
Many of the symptoms of RA mirror those of PsA. Which is why oftentimes, the presence of psoriasis is a distinguishing factor in what type of arthritis you might be diagnosed with. Flare-ups are also common during RA where the symptoms wax and wane. You might experience time periods of minimal symptoms and times when symptoms flare-up. In both RA and PsA, it is important to try to pinpoint what causes flare-ups. If you can determine underlying factors of the flare-ups , you might be able to minimize the presence of these symptoms. As with PsA, the following are RA symptoms that you may or may not have. You might only experience one or two of these symptoms or you might experience more.
Some of the more common symptoms of RA include:
- Joint stiffness
Heart And Blood Vessels
People with RA are more prone to atherosclerosis, and risk of myocardial infarction and stroke is markedly increased.Other possible complications that may arise include: pericarditis, endocarditis, left ventricular failure, valvulitis and fibrosis. Many people with RA do not experience the same chest pain that others feel when they have angina or myocardial infarction. To reduce cardiovascular risk, it is crucial to maintain optimal control of the inflammation caused by RA , and to use exercise and medications appropriately to reduce other cardiovascular risk factors such as blood lipids and blood pressure. Doctors who treat people with RA should be sensitive to cardiovascular risk when prescribing anti-inflammatory medications, and may want to consider prescribing routine use of low doses of aspirin if the gastrointestinal effects are tolerable.
Dont Miss: Things To Help Arthritis In Hands
You May Like: Is Lidocaine Good For Arthritis
How Are Rheumatoid Arthritis And Psoriatic Arthritis Treated
Many of the same treatment options are used to treat both RA and PsA. Nonsteroidal anti-inflammatory drugs , such as aspirin and Ibuprofen, are useful for over-the-counter treatment of both conditions. Corticosteroid joint injections can provide quick relief for RA and PsA symptoms. Side effects associated with steroid use, and with oral steroids especially, mean these medications are not a good long-term option for treating joint pain. In addition, corticosteroid use can make psoriasis flare-ups more volatile in people who have PsA.
Methotrexate, a disease-modifying antirheumatic drug , is the most commonly used DMARD for RA. Methotrexate is sometimes prescribed off-label for PsA. However, it is not as effective for PsA as it is for RA.
Biological DMARDs, such as Enbrel , Remicade , Humira , Simponi , and Cimzia are approved by the U.S. Food and Drug Administration for moderate to severe RA and for PsA. Some of these drugs may be administered along with methotrexate. Unlike methotrexate, biological DMARDs have been shown to be effective in preventing bone erosion in people with RA and PsA, making these drugs especially helpful.
Inflammation in RA is associated with a different interleukin called IL-6. The IL-6 inhibitor drugs Actemra and Kevzara work against RA, but have not been proven to help with PsA.
In addition, Rituxan and Kineret can be helpful for RA that has not responded to other types of treatment. However, these drugs are not useful in treating PsA.
Rheumatoid Arthritis And Psoriatic Arthritis: The Similarities And Differences
All forms of arthritis involve tenderness and swelling of the joints. And, at first glance, psoriatic arthritis can be very hard to differentiate from other common types of arthritis, including rheumatoid arthritis and osteoarthritis.
Because psoriatic arthritis symptoms can overlap with those of rheumatoid arthritis and osteoarthritis not just swollen, achy joints but also stiffness and chronic fatigue diagnosing this autoimmune disease can be tricky.
Unlike rheumatoid arthritis, there is no blood test that can determine if a person has psoriatic arthritis, says M. Elaine Husni, MD, MPH, a rheumatologist at the Cleveland Clinic in Ohio.
Psoriatic arthritis can also affect the body in different ways depending on the person and how advanced the disease is, says Dr. Husni. As a result, a rheumatologist may need to examine a patient several times and run a number of tests before having enough information to make a definitive diagnosis.
Read Also: How To Tell If You Have Arthritis
What Is Psoriatic Arthritis Video
Psoriatic arthritis can cause pain, swelling and stiffness inand around your joints.
It usually affects 3 in 10 people who already have the skin condition psoriasis .
Psoriasis causes patches of red, flaky skin which is covered with silvery-like patches.
Some people may develop psoriatic arthritis before the psoriasis is even present. In rare cases people have psoriatic arthritis and never have any noticeable patches of psoriasis.
Psoriatic arthritis and psoriasis are both autoimmune conditions, caused by a fault in the immune system.
Our immune system protects us from illness and infection. But in autoimmune conditions, the immune system becomes confused and attacks healthy parts of the body, often causing inflammation.
Psoriatic arthritis is a type of spondylarthritis. This is a group of conditions with some similar symptoms.
People with psoriasis are as likely as anyone else to get othertypes of arthritis, such asosteoarthritisorrheumatoid arthritis. Theseconditionsare not linkedto psoriasis.
Ra Vs And There Are At Least Two Types That Might Be Responsible For Your Tender Psa Can Range From Mild To Severe Of Course It Causes Stiffness And Painanother Notable Difference From Ra Psoriatic Arthritis: How Do You Tell The Difference
Both rheumatoid arthritis and psoriatic arthritis are conditions that damage your joints, Mild PsA is sometimes referred to as oligoarticular, Synovial membrane histology and immunopathology in rheumatoid arthritis and osteoarthritis, Rheumatoid arthritis is a chronic inflammatory disorder that typically affects the small joints in your hands and feet.PsA vs, and swelling in
You May Like: Can Rheumatoid Arthritis Affect The Jaw
Pharmaceutical Treatments For Ra And Psa:
- Non-steroidal anti-inflammatory drugs such as ibuprofen and naproxen
- Corticosteroids like prednisone
- Disease-modifying anti-rheumatic agents like methotrexate and hydroxychloroquine
- Biologics, a more advanced type of DMARD that can stop or slow inflammation these include Tumor Necrosis Factor- inhibitors and interleukin inhibitors
What Are The Symptoms Of Psoriatic Arthritis And Rheumatoid Arthritis
Both rheumatoid arthritis and psoriatic arthritis cause similar joint symptoms. The affected joints are painful and stiff, and feel swollen and hot. However, RA and PsA tend to show up in different joints. For example, they affect different parts of the spine. RA often causes problems in the cervical spine in the neck. Up to 80 percent of people with RA report experiencing neck pain. PsA often causes a condition called spondylitis, which causes lower back pain. Spondylitis involves inflammation in the joints of the spine and between the spine and pelvis. Up to half of people with PsA will experience spondylitis pain.
RA is also more likely to affect the hands, such as the joints in the wrists and fingers, while PsA is more likely to affect the feet. RA and PsA affect different small joints within fingers and toes. RA affects the joints closest to the hands and feet and the middle finger and toe joints, while PsA attacks the joints closest to the nail bed. People with PsA can experience a condition called dactylitis, in which the fingers or toes swell up and resemble sausages. Dactylitis is often the first symptom of PsA, and it may be the only joint symptom for several years. PsA even affects the nails themselves. People with PsA often have pitted, ridged nails, which appear similar to nails with a fungal infection.
Don’t Miss: Is Cold Weather Bad For Arthritis
What Are The Symptoms Of Psoriasis
There are different types of psoriasis. The most common is chronic plaque psoriasis. This causes patches of red, raised skin, with white and silvery flakes.
It can occur anywhere on the skin, but most commonly at the elbows, knees, back, buttocks and scalp.
Psoriasis can cause small round dents in finger and toe nails, this is known as pitting. Nails can also change colour, become thicker and the nail may lift away from your finger.
Who Should Diagnose And Treat Ra
A doctor or a team of doctors who specialize in care of RA patients should diagnose and treat RA. This is especially important because the signs and symptoms of RA are not specific and can look like signs and symptoms of other inflammatory joint diseases. Doctors who specialize in arthritis are called rheumatologists, and they can make the correct diagnosis. To find a provider near you, visit the database of rheumatologistsexternal icon on the American College of Rheumatology website.
Donât Miss: How Do You Know If Your Dog Has Arthritis
Also Check: Can You Get Rheumatoid Arthritis In Your Hips
Introduction To Psoriatic Arthritis Rheumatoid Arthritis And Osteoarthritis
Psoriatic arthritis is a chronic inflammatory heterogeneous arthritis that is associated with psoriasis, and approximately 30% of patients with psoriasis develop PsA . It is estimated that PsA has a prevalence rate of approximately 12 per 1000 in the general population and an incidence rate of approximately 6 per 100,000 per year . Generally, onset of PsA occurs between ages 30 and 50 years but can develop at any point throughout a patients lifetime. The Group for Research and Assessment of Psoriasis and Psoriatic Arthritis defined six clinical domains that can be involved with PsA: peripheral arthritis, enthesitis, dactylitis, psoriasis, psoriatic nail disease, and axial disease .
A proper diagnosis and timely treatment of PsA are essential to prevent permanent joint damage and decrease functional disability . Patients are often seen by various healthcare providers on their pathway to a diagnosis of PsA, including dermatologists, orthopedists, general practitioners, chiropractors, and advanced practice providers . Diagnosis of PsA relies on early detection through appropriate history taking, careful examination, and clinical judgment, and APPs are in a position to see many patients with different rheumatic diseases therefore, it is imperative that APPs are aware of and receive proper training to accurately screen for features to identify PsA.
How Do Ra And Psa Affect You
When you have RA, your immune system attacks the lining of the tissues around your joints. They swell up and become painful. Over time, they can become damaged and deformed.
With PsA, your immune system attacks and damages not just your joints, but your skin, as well. It causes your body to make too many skin cells, which leads to psoriasis, a skin condition that often affects people with PsA.
You May Like: How To Deal With Arthritis Pain
Preparation And Procedure For An Endoscopy
Preparation can vary slightly depending on the type of endoscopy youre having. Some endoscopies require small incisions, while others do not.
Youll likely be asked not to eat solid foods on the day of your procedure. You might be asked to stop taking certain medications as well, especially medications that affect bleeding, such as anticoagulants. If youre having an endoscopy for gastrointestinal issues, your doctor might give you laxatives or enemas the night before to help clear your system for the procedure.
Most endoscopies are outpatient procedures. Youll often receive some form of sedation or anesthesia so that you dont feel any pain. The exact type depends on the procedure and your preferences. You can discuss this with your doctor before your endoscopy.
The length of the procedure will also depend on the exact type of endoscopy youre having. For instance, it will take longer if an incision is needed, or if the surgeon is also removing tissue for a biopsy. Your doctor will go over these details with you before the procedure.
What Are The Signs And Symptoms Of Rheumatoid Arthritis And Psoriatic Arthritis
Rheumatoid arthritis
Signs and symptoms of RA may not stay the same all the time. There may be periods of worsening symptoms called flare-ups or improvements in symptoms called remission.
Symptoms and signs of RA are divided into two main categories:
You May Like: How To Pronounce Rheumatoid Arthritis