Clinical Characteristics Of Ra And Psa
For RA, the American College of Rheumatology /European League Against Rheumatism classification criteria were designed for patient characterisation and use in clinical trials. The key clinical characteristic is the confirmation of definite, persistent, clinical synovitis in at least one joint. The criteria include the number of joints involved, duration of symptoms, and the demonstration of serological markers and an elevated acute-phase reactant. For PsA, the Classification Criteria for Psoriatic Arthritis help categorise patients with inflammatory articular disease for clinical trials. Key clinical characteristics include a personal or family history of psoriasis, psoriatic nail dystrophy and dactylitis. Neither classification criteria should be confused as diagnostic criteria.
Joint involvement is predominantly symmetric in RA and often, but not always, asymmetric in PsA. In both RA and PsA, most patients have polyarthritis , although joint involvement can be oligoarticular or polyarticular. Monoarticular disease is less common in PsA however, 5%10% of patients may present with isolated distal joint involvement. In PsA, prognosis worsens and symmetry of joint involvement tends to increase as the number of affected joints increases.
Patient Reported Outcome Measures And Laboratory Assessments
S2 Table shows patient-reported outcome measures and laboratory measures, both unadjusted values and values adjusted for sex and age. In the adjusted analysis patients mean global assessment was significantly lower for RA patients than for PsA and ax-SpA patients, whereas no significant difference was found for evaluators global assessment between the diagnosis groups. RA patients also reported significantly less pain than the PsA and the ax-SpA patients . Similar results were also seen for joint pain . RA patients also experienced significantly less fatigue than the PsA and the ax-SpA patients .
Further, the ax-SpA patients reported significantly more spine pain and spine pain at night than the RA and the PsA patients. In terms of patients global evaluation, pain, joint pain and fatigue, the PsA patients had similar values to the ax-SpA patients, while the RA patients had significantly lower values. These differences in patient reported outcome measures were still significant when adjusted for current use of bDMARDs, steroids and disease duration.
There was no significant difference in morning stiffness, ESR, CRP or MHAQ between the RA, PsA and ax-SpA groups. BASDAI and BASFI were significantly higher in the ax-SpA group than in the PsA group.
Supplementary subgroup analyses of patient-reported outcome measures and laboratory measures were performed for only seropositive RA patients compared to PsA and ax-SpA patients. This did not change the main outcomes .
What Tests To Perform
Laboratory testing
The most important role of lab testing is to exclude other considerations in the differential diagnosis. Anti-cyclic citrullinated peptide antibodies and antinuclear antibodies may be helpful in some patients if there are symptoms that suggest a diagnosis of RA or systemic lupus erythematosus . However, some patients with psoriatic arthritis alone may have positive tests. Acute phase reactants may provide insights into disease activity, although many patients with active PsA have normal acute phase reactants.
It is also important to check a comprehensive metabolic and lipid profile since obesity, metabolic syndrome, type 2 diabetes, fatty liver, and hyperlipidemia are very common features in PsA and the presence of these conditions will influence treatment considerations. In patients who are under consideration for a DMARD, such as methotrexate of leflunomide, it is recommended to check hepatitis B and C serologies and baseline transaminases testing for exposure to tuberculosis should be done if a biologic, such as an anti-TNF agent, is anticipated. An increased rate of progressive liver fibrosis based on serial biopsies was reported in psoriasis patients with obesity or type II diabetes treated with methotrexate. It is also critical to ensure that women of child-bearing age are not pregnant so a pregnancy test may be required.
Imaging
Skin biopsy
Controversies in diagnostic testing
Also Check: Symptoms Of Arthritis In Knees And Legs
What Happens To Patients With Psoriatic Arthritis
Genes implicated in the pathogenesis of PsA include Cw6,IL-23 R alleles and Act1, a molecule in the IL-17R signaling pathway and other MHC Class I alleles , Class I major histocompatibility complex chain-related gene A . Environmental events have also been associated with the onset of psoriatic arthritis, including rubella vaccination, injury sufficient to require a medical consultation, recurrent oral ulcers, moving house and fracture requiring hospitalization.
From a clinical perspective, PsA patients can present with features of RA or spondyloarthritis . The synovial pathology is more akin to findings in spondyloarthritis than RA with infiltrating neutrophils, CD163+ macrophages, and the lack of an antibody response to the shared epitope as observed in RA.The importance of local biomechanical properties in disease pathogenesis, particularly as it relates to the enthesis, has been emphasized. The model of the synovio-entheseal complex delineates an innate immune response triggered by biomechanical and inflammatory events at the enthesis, which subsequently involve adjacent synovium and cartilage.
Mortality rates for PsA were higher than age-matched controls but recent evidence indicates that mortality may not be higher than observed in the general population. PsA patients do have higher rates of mortality from cardiovascular disease than controls.
Pharmacologic considerations
What Causes Oa And Who Is At Risk
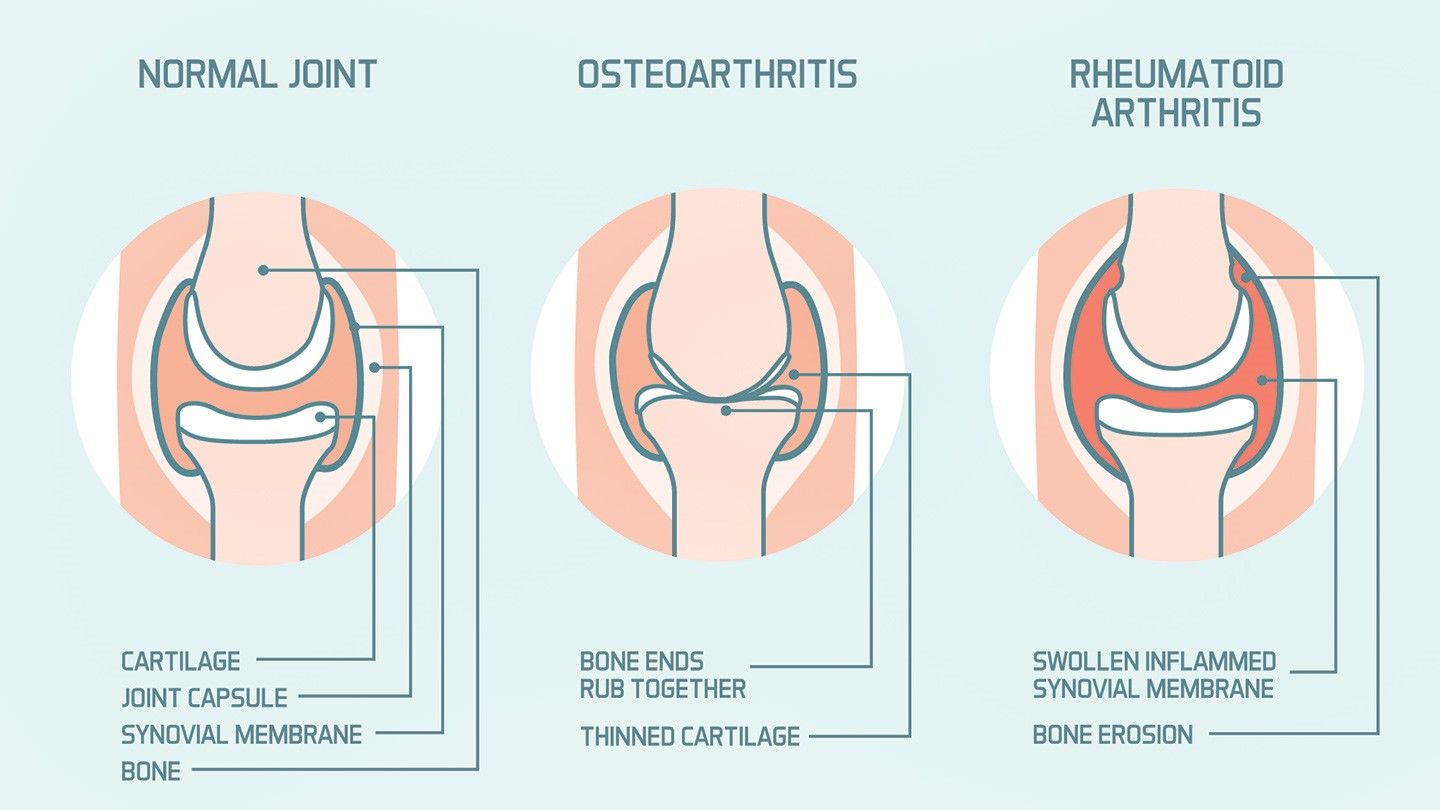
OA causes the cartilage inside the joints to break down and wear away. Cartilage is the flexible connective tissue that surrounds the ends of your bones.
In healthy joints, cartilage helps grease the movement of the joint and absorbs the shock of impact when you move. When you have OA, the layers of your cartilage begin to break down.
Without cartilage, your bones rub painfully against each other. This can cause permanent damage to both your joints and your bones.
These risk factors can increase your chances of developing OA:
- Genes. Certain inherited genetic changes may increase your odds of developing OA. If a family member has the disease, its possible youll get it as well.
- Age. Your likelihood of getting this type of arthritis increases as you age.
- Gender. Women are
- joint support, such as braces
- alternative remedies
If your joint is badly damaged, you may need surgery. OA surgery replaces the damaged joint with an artificial joint made from plastic or metal.
You May Like: What Does The Rash From Psoriatic Arthritis Look Like
Psoriatic Arthritis Vs Osteoarthritis: Us Prevalence
The number of people in the United States who suffer from osteoarthritis is quite astonishing. Research suggests that 70 percent of adults between 55 and 78 years old have OA. Hip osteoarthritis is the most common complaint in North America. Knee is also rather prevalent. Data on osteoarthritis is largely based on self-reports and radiographic data. How does this compare to psoriatic arthritis? The exact number of people in the U.S suffering from PsA is not known, but some estimate it affects around one percent of the population. While it can develop at any time in a persons life, it seems that most often it occurs between the ages of 30 and 50. While osteoarthritis appears to attack more women than men, psoriatic arthritis attacks men at the same or at a slightly higher rate, compared to women. It is believed that between 18 and 42 percent of people who have psoriasis also have psoriatic arthritis.
What Are The Symptoms Of Psoriasis
There are different types of psoriasis. The most common is chronic plaque psoriasis. This causes patches of red, raised skin, with white and silvery flakes.
It can occur anywhere on the skin, but most commonly at the elbows, knees, back, buttocks and scalp.
Psoriasis can cause small round dents in finger and toe nails, this is known as pitting. Nails can also change colour, become thicker and the nail may lift away from your finger.
Read Also: The Symptoms Of Arthritis
Blood Tests For Psa And Ra
Blood tests can also help tell the difference between PsA and RA.
About 80 percent of people with RA are said to have seropositive RA, which means they test positive for rheumatoid factor or for cyclic citrullinated peptide antibodies.
Most people with PsA do not have RF or CCP antibodies and are considered seronegative. However, it is also possible to have seronegative RA.
So What Is Psoriatic Arthritis And How Does It Differ From Rheumatoid Arthritis
Well, just like rheumatoid arthritis, it is an auto-immune disease. Both cause an erosive inflammatory arthritis in addition to chronic fatigue. And both can have symptoms that vary greatly from person to person. However the distribution of joint involvement differs between the two diseases and psoriatic arthritis involves the skin as well as the joints.
Both diseases can cause destruction of the small joints in your hands and feet as well as larger joints such as knees, hips, shoulders and even the vertebrae in your spine. Classic rheumatoid arthritis primarily involves the PIP joints and wrist, and is generally a symmetrical disease effecting both sides of the body equally. Also with rheumatoid arthritis, nodules specific to this disease are often present.
Both diseases can involve inflammation and scarring of major organs such as your heart and lungs and as in my case can involve your eyes. In addition, both can increase your risk of osteoporosis due the condition itself and also from some of the medications that are used to treat these conditions. After years of taking steroids for my arthritis, it resulted in a couple of compression fractures in my thoracic spine. And, both disorders can also result in joint destruction leading to severe crippling disabilities.
- Was This Helpful?
Recommended Reading: Ra Symptoms In Wrist
Spondylitis With Or Without Sacroiliitis
This occurs in approximately 5% of patients with psoriatic arthritis and has a male predominance.
Clinical evidence of spondylitis and/or sacroiliitis can occur in conjunction with other subgroups of psoriatic arthritis.
Spondylitis may occur without radiologic evidence of sacroiliitis, which frequently tends to be asymmetrical, or sacroiliitis may appear radiologically without the classic symptoms of morning stiffness in the lower back. Thus, the correlation between the symptoms and radiologic signs of sacroiliitis can be poor.
Vertebral involvement differs from that observed in ankylosing spondylitis. Vertebrae are affected asymmetrically, and the atlantoaxial joint may be involved with erosion of the odontoid and subluxation . Therapy may limit subluxation-associated disability.
Unusual radiologic features may be present, such as nonmarginal asymmetrical syndesmophytes , paravertebral ossification, and, less commonly, vertebral fusion with disk calcification.
Symptoms Of Psoriatic Arthritis
The severity of the condition can vary considerably from person to person. Some people may have severe problems affecting many joints, whereas others may only notice mild symptoms in 1 or 2 joints.
There may be times when your symptoms improve and periods when they get worse .
Relapses can be very difficult to predict, but can often be managed with medicine when they do occur.
You May Like: Rheumatoid Arthritis And Lower Back Pain
Past Research And Achievements In This Area
In 2015, research led by our centre for genetics and genomics at the University of Manchester identified genetic variants associated with psoriatic arthritis, but not with psoriasis or rheumatoid arthritis. This helped to establish psoriatic arthritis as a condition in its own right. The findings could lead to the development of drugs specifically for psoriatic arthritis.
Later in the same year, our TICOPA trial looked at the benefits of early aggressive drug treatment for people with psoriatic arthritis followed by an increase in drug dosage if initial treatment isnt working. The trial found that patients treated this way, required fewer hospital- and community-based services than patients receiving the standard care.
Treatment For Psoriatic Arthritis

Treatment for psoriatic arthritis aims to:
- relieve symptoms
- slow the condition’s progression
- improve quality of life
This usually involves trying a number of different medicines, some of which can also treat the psoriasis. If possible, you should take 1 medicine to treat both your psoriasis and psoriatic arthritis.
The main medicines used to treat psoriatic arthritis are:
- non-steroidal anti-inflammatory drugs
- biological therapies
You May Like: Rheumatoid Arthritis Articles
What Are The Symptoms Of Ra
Many of the symptoms of RA mirror those of PsA. Which is why oftentimes, the presence of psoriasis is a distinguishing factor in what type of arthritis you might be diagnosed with. Flare-ups are also common during RA where the symptoms wax and wane. You might experience time periods of minimal symptoms and times when symptoms flare-up. In both RA and PsA, it is important to try to pinpoint what causes flare-ups. If you can determine underlying factors of the flare-ups , you might be able to minimize the presence of these symptoms. As with PsA, the following are RA symptoms that you may or may not have. You might only experience one or two of these symptoms or you might experience more.
Some of the more common symptoms of RA include:
- Joint stiffness
One Side Or Both Sides
Another difference between the two diseases is whether they affect one or both sides of the body. PsA tends to be asymmetric, meaning it affects different joints on either side of the body. RA is more likely to cause symmetrical joint pain and stiffness it affects the same joints on both sides of the body, such as both hands or wrists.
You May Like: Rh Arthritis Treatment
Psoriatic Arthritis Vs Osteoarthritis Differences In Symptoms Causes And Treatment
Written byDr. Victor MarchionePublished onJune 30, 2016
Psoriatic arthritis and osteoarthritis can both affect small joints and can easily be mistaken for each other, but they are two different conditions that require separate treatments.
Osteoarthritis is a wearing away of cartilage, usually associated with aging. Psoriatic arthritis is an inflammatory condition in which the joints become inflamed and damaged. There can be inflammation in osteoarthritis, but it is not a major characteristic of the condition, so if a person simply treats their osteoarthritis pain with anti-inflammatories, they may not experience much relief. Both osteoarthritis and psoriatic arthritis can lead to bone spurs, so the two conditions sometimes look the same. Researchers report that osteoarthritis is the most common misdiagnosis for psoriatic arthritis.
People who suffer from osteoarthritis experience the bones of the joint rubbing against each other, which causes friction and pain. In the majority of cases, this rubbing affects the hands, knees, hip, and spine. More people have osteoarthritis than any other form of arthritis.
Similiarities Between Psa & Ra
Taking a large step back, these two could be completely indistinguishable, leading to much confusion. It isnt until we really scrutinize what someone is going through on a daily basis, that we can really tell them apart. From a further away standpoint however, both PsA and RA possess many of the same defining features:
- Both PsA and RA are auto-immune conditions: This means that the body mistakenly attacks its own healthy cells in both conditions. This is why individuals with RA and PsA both experience erosive joint symptoms, such as swelling, pain, and stiffness, as well as chronic fatigue from an immune system working in overdrive.
- Both affect internal organs: Long-term progression of both PsA and RA can lead to scarring, inflammation, and damage to major internal organs, such as the heart and lungs. This process is incredibly similar in both!
- Accompanying osteoporosis: Both PsA and RA can lead to a weakening of bones, otherwise known as osteoporosis. This can make additional fracturing of bones or joints incredibly easy for individuals with PsA and RA.
- Similar treatment algorithms: Treatment of RA and PsA can be virtually identical at times, and include anti-inflammatory medications , corticosteroids, DMARDS , and even surgery to stabilize affected joints in serious cases.
Recommended Reading: How To Prevent Rheumatoid Arthritis In Hands
How Psoriatic Arthritis And Rheumatoid Arthritis Differ
Psoriatic arthritis and rheumatoid arthritis are both autoimmune diseases that affect the joints. Both are inflammatory and progressivecausing joint stiffness, pain, and swelling, as well as persistent fatigue. In addition, both occur in flares and can be treated with medications that suppress the immune system.
However, PsA and RA are different diseasesand the differences are important when it comes to their prognosis and the best approach for managing each condition.
With PsA, the joint symptoms are tightly linked to inflammation of the skin from psoriasis . With RA, the immune system primarily targets joint tissue.
The different underlying disease processes mean that the conditions are diagnosed with different methods and they also require different therapeutic approaches.
Can Psoriatic Arthritis Affect Other Parts Of The Body
Having psoriatic arthritis can put you at risk of developing other conditions and complications around the body.
The chances of getting one of these are rare. But its worth knowing about them and talking to your doctor if you have any concerns.
Eyes
Seek urgent medical attention if one or both of your eyes are red and painful, particularly if you have a change in your vision. You could go to your GP, an eye hospital, or your local A& E department.
These symptoms could be caused by a condition called uveitis, which is also known as iritis. It involves inflammation at the front of the eye.
This can permanently damage your eyesight if left untreated.
Other symptoms are:
- blurred or cloudy vision
- sensitivity to light
- not being able to see things at the side of your field of vision known as a loss of peripheral vision
- small shapes moving across your field of vision.
These symptoms can come on suddenly, or gradually over a few days. It can affect one or both eyes. It can be treated effectively with steroids.
Heart
Psoriatic arthritis can put you at a slightly higher risk of having a heart condition. You can reduce your risk by:
- not smoking
- staying at a healthy weight
- exercising regularly
- eating a healthy diet, thats low in fat, sugar and salt
- not drinking too much alcohol.
These positive lifestyle choices can help to improve your arthritis and skin symptoms.
Talk to your doctor if you have any concerns about your heart health.
Crohns disease
Non-alcoholic fatty liver disease
Don’t Miss: Rheumatoid Arthritis Better With Movement