Treatment Of Stage 4 Ra
After trying all medical options, surgery may be the next option for patients with stage 4 RA. Surgery may be required to repair joint damage, repair tendons, remove the synovium or nodules, separate fused joint, or replace a damaged joint.
Patients usually rely on assistive mobility devices to perform their daily tasks.
Signs Ra Is Progressing
Most people with RA experience a gradual worsening of symptoms. There may be periods of relief, where RA is more manageable. At other times, RA symptoms may flare up and be more intense.
How your condition progresses depends on many factors, including:
- family history of RA
- stage of RA at diagnosis
- any disease triggers that are specific to you
- the presence of certain antibodies in your blood
However, keep in mind that its impossible to predict exactly how RA will progress over time in any individual person. Even if you have family members with RA, your condition may progress differently from theirs.
The Johns Hopkins Arthritis Center notes that the usual course of RA progression for most people includes flare-ups of high disease activity. Over time, those flare-ups become lengthier and more challenging.
Another common pattern occurs when people experience strong attacks in the early stages of RA, followed by periods with minimal disease activity.
Less than 10 percent of people with RA fall into spontaneous remission within the first 6 months of the onset of their symptoms. Remission from RA has a precise medical definition.
In general, it means that RA disease activity stops. Patients who do not demonstrate the disease markers anti-cyclic citrullinated peptide antibody and rheumatoid factor have a greater chance of achieving remission.
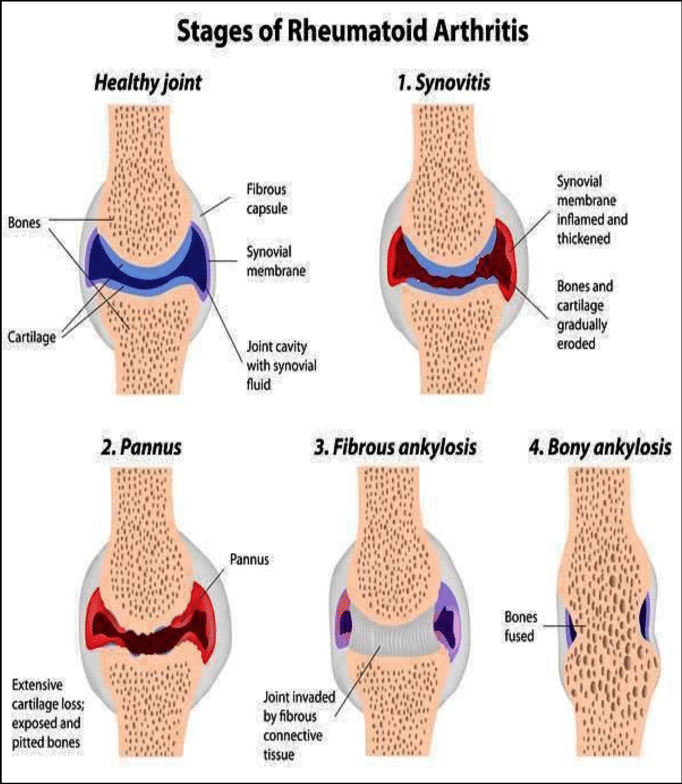
Stages Of Rheumatoid Arthritis
There are four stages. Each has its own treatment options.
Stage 1:
- In the early stages, your joint lining, or synovium, becomes inflamed. The bones arenât damaged yet. But the tissue around them often swells, making your joint stiff and painful.
Stage 2:
- In this moderate stage, inflammation damages your cartilage, the cushiony stuff that protects the ends of your bones.
- The joint will be stiff, and you wonât be able to move it as far as you used to. The doctor will say youâve lost range of motion.
Stage 3:
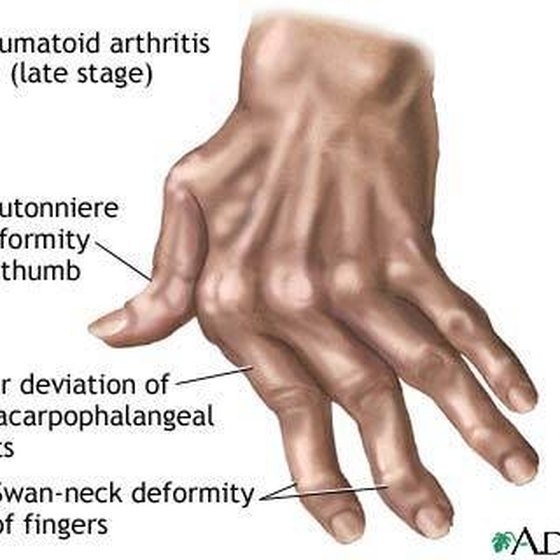
- This is the severe stage. Inflammation is wearing away cartilage and causes erosion of bones near your joints. The joints may become unstable. You might start to notice deformities as the bones move around. Youâll have pain, swelling, and loss of motion.
Stage 4:
- In end stage RA, inflammation stops, but the damage continues. The joint might stop working. Youâll still have pain, swelling, stiffness, and lack of motion. Your muscles may be weak, too. It could be time for joint replacement surgery.
You May Like: Tomatoes Bad For Arthritis
Treatment Of Stage 1 Ra
In the early stage, rheumatoid arthritis, the first line of treatment is the use of Methotrexate.
Methotrexate is a chemotherapy medication that alters the immune system response. It can be taken in the form of pill or injection.
Other medications that change the bodys immune response over time, known as disease-modifying antirheumatic drugs , can also be used to treat early stage of RA.
DMARDs such as leflunomide, hydroxychloroquine, and sulfasalazine are commonly used for the treatment of RA.
Additional treatments may be required to fully manage and slow down the progression of RA. Additional treatment options that may be used include:
- Over-the-counter or prescription nonsteroidal anti-inflammatory drugs . These medications can be in the form of pills, patches, or topical ointments
- Prescription corticosteroids such as methylprednisolone, prednisolone, and prednisone are used to relieve pain and reduce inflammation.
- Physical therapy involves strengthening and stretching exercises to help strengthen the bones of the joint and make the joint more flexible.
- Occupational therapy can also help to improve RA.
Third Stage: Visible Symptoms
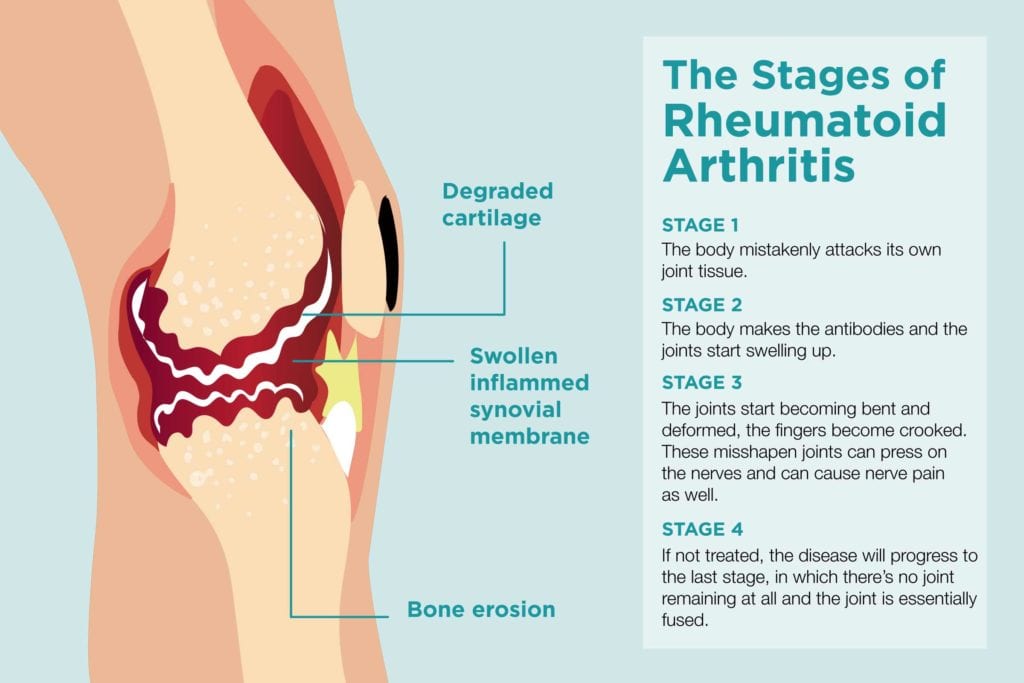
This stage is severe, and blood tests or imaging are not/less relevant to diagnosis because you can see the effect of the disease. It may start bending and deforming, your fingers may crook, and you can see other symptoms. It can press nerves and cause nerve pains also. Before few years, we could see more deformed joints when there were no available treatments.
You May Like: Bee Pollen For Arthritis
When To Go To Your Doctor:
The following are guidelines of when to go to your rheumatologist for rheumatoid arthritis treatment:
- When you first experience symptoms like small or large joint pain, stiffness, difficult move joints.
- Once in a three month during first few years of diagnosis
- If you experience progressive rheumatoid arthritis
- If you have worsening symptoms or new symptoms.
The Stages Of Osteoarthritis
- Early-Stage Osteoarthritis: In the early stage of osteoarthritis, the cartilage located in a joint begins to thin. This continues until the person begins to experience occasional pain, as friction develops between the bones at the joint. In this stage of the condition, losing weight and reducing stress on the joints can help reduce the pain. In the early stage of osteoarthritis, it is common to have one or more joints experiencing symptoms.
- Moderate-Stage Osteoarthritis: In this stage, patients often begin to take medications to control the pain. The joints become inflamed and painful much more often during this stage. While its common to experience more pain when pressure is put on joints in this stage, living a moderately active lifestyle actually helps reduce pain.
- Late-Stage Osteoarthritis: In this stage of osteoarthritis, pain, stiffness, and inflammation are common in multiple joint areas. Its common to take stronger pain medications to help reduce pain. Its also common to get joint replacement surgery in this stage, because medications and other treatment methods are not working to reduce pain and to increase mobility.
You May Like: Is Tomato Bad For Arthritis
What Makes Ra Get Worse
Different factors affect the pace and progression of individual patients RA. Some things you cant control, like whether you have a family history of the disease. In addition, although women are more likely to get RA, when men get rheumatoid arthritis, their prognosis is generally worse, Dr. Bhatt says.
But there are factors you can control and change. We know smoking makes RA more aggressive, so smoking cessation is key, Dr. Lally says. Also, people with heavy manual occupations might stress the joints further and might have quicker progression, Dr. Bhatt says. If your workplace can make accommodations for your disease, that will help. Read more about how to make working with arthritis easier.
Exercise and maintaining a healthy weight can also help reduce stress on the joints, Dr. Bhatt says. But talk to your doctor before starting a workout regimen. A physical therapist can advise patients on the right type of exercise, he says. If patients do exercises wrong it could stress the joints even further. In addition, getting enough sleep, starting an anti-inflammatory diet, eating less red meat, and possibly using herbal remedies like turmeric may help control RA, Dr. Bhatt says. Here are more healthy habits to adopt if you have RA.
Know When It Is Progressing:
A persons joints tell him about the progress of RA. It may worsen the pain, increase the swelling, and have other symptoms. The episodes may become more frequent, longer, and painful. Other symptoms are shortness of breath and red and paining eyes. It shows that RA affects other symptoms of the body.
Don’t Miss: Is Banana Good For Arthritis
Possible Complications Of Rheumatoid Arthritis
In general, patients with RA have frequent comorbidities, that is, other chronic disorders that complicate their overall health.
- Patients with RA have reduced healthspan and lifespan.
- RA increases the risks of cardiovascular diseases, such as hypertension, diabetes, and elevated cholesterol, even beyond the usual factors.
- Patients with RA also have about twice the risk of lymphoproliferative diseases, such as leukemia and lymphoma.
- Some of the medications used for RA treatment may result in adverse effects and can increase the risk of infection or kidney problems, thus requiring close monitoring.
When To Seek Treatment
The following are general guidelines of when to seek treatment for your RA progression:
When you first suspect symptoms Regularly during the first few years of diagnosis If you suspect you are experiencing progressive rheumatoid arthritis If you feel your condition is worsening in any way or new symptoms appear
Recommended Reading: Is Banana Good For Rheumatoid Arthritis
The Stages Of Rheumatoid Arthritis
- Stage 1: In the early stage of rheumatoid arthritis, its common to have inflammation, pain, and stiffness in just a few joints in the body. Typically, this reaction comes after doing a strenuous activity.
- Stage 2: In this stage of rheumatoid arthritis, the cartilage in the joints is decreasing and inflammation is increasing. In this stage of the disease, patients begin to experience problems with mobility.
- Stage 3: This stage is considered severe rheumatoid arthritis. In this stage, not only is the cartilage deteriorating, but also the bones at the joints are wearing away. This causes a lot of pain and decreases mobility and muscle strength in multiple parts of the body.
- Stage 4: In this stage of the disease, mobility becomes extremely limited, and joints stop functioning the way they are supposed to. Pain, inflammation, and loss of mobility are severe symptoms in this stage.
How Is Ra Treated
RA can be effectively treated and managed with medication and self-management strategies. Treatment for RA usually includes the use of medications that slow disease and prevent joint deformity, called disease-modifying antirheumatic drugs biological response modifiers are medications that are an effective second-line treatment. In addition to medications, people can manage their RA with self-management strategies proven to reduce pain and disability, allowing them to pursue the activities important to them. People with RA can relieve pain and improve joint function by learning to use five simple and effective arthritis management strategies.
Also Check: Remedy For Arthritis In Lower Back
Five Warning Signs Of Rheumatoid Arthritis
When you subscribe we will use the information you provide to send you these newsletters.Sometimes theyll include recommendations for other related newsletters or services we offer.Our Privacy Notice explains more about how we use your data, and your rights.You can unsubscribe at any time.
There are four stages of rheumatoid arthritis, according to the charity Creaky Joints. The chronic condition might not have a cure, but early medical intervention can slow down its progression. Rheumatologist Dr Rajat Bhatt said: In early rheumatoid arthritis, the patient may not have many symptoms except for some stiffness in the early hours of the morning. Early morning stiffness primarily affects the small joints in the hands, feet and knees.
If the stiffness subsides with movement, its indicative of rheumatoid arthritis rather than osteoarthritis.
Definite testing for RA in this early stage may be difficult, as X-rays can appear normal.
More sensitive imaging like an ultrasound may show inflammation in an affected joint, but sometimes it wont.
This is replicated in blood tests, which may or may not have inflammatory markers.
As a result, many people with RA will progress onto the next stage of the disease without a diagnosis.
In the second stage the body makes the antibodies and the joints start swelling up, Dr Bhatt explained.
It can affect other organ systems and cause inflammation there: the lungs, the eyes, a skin rash, and it can even affect the heart.
There Are 4 Stages To Rheumatoid Arthritis I Have Stage 2 What Do You Have
Rheumatoid Arthritis is a progressive disease. It does not start at the most severe stage. Instead, it slowly progresses. It is sometimes difficult to diagnosis what stage one is in because it is under the skin. However, Drs. are able to roughly guess what stage it is in based on severity of symptoms. Below are the different stages of Rheumatoid Arthritis progression. No one suffers from RA the same way so you might not fit perfectly into one stage but instead you might overlap two stages.
Stage 1: The first stage. There is some small inflammation in the joints and slight swelling. You feel some joint pain, swelling, and stiffness. You think something is wrong and you first go to the Dr. to find out what. This is when the first diagnosis usually starts
Stage 2: The inflammation has progressed where there is cartilage damage. You lose slight mobility and cant move like you used to. You start to understand how exactly this condition will affect your life in the future.
Stage 3: Even though this is just the third stage, it is now considered severe rheumatoid arthritis. The inflammation that is damaging your cartilage is now affecting the bone as well. Your constantly in pain and are probably taking a medication to help with it. Your mobility continues to be negatively affected and you may develop some signs of physical change on the outside of the affected joints.
Which stage do you have? Comment Below
Read Also: Is Banana Good For Rheumatoid Arthritis
Stage : The Early Stage
Early stage rheumatoid arthritis often causes joint stiffness, swelling and pain, as well as fatigue. The key to alleviating these symptoms and preventing damage to the joints is to address inflammation as quickly as possible.
Your healthcare provider may prescribe steroids along with a disease-modifying antirheumatic drug for this purpose. DMARDs can help prevent irreversible damage from happening to your joints, as well as slow down the advancement of rheumatoid arthritis. Methotrexate, a drug originally created to treat cancer, is the DMARD most often used to treat rheumatoid arthritis.
If you are a smoker with this disease, it is important that you kick the habit, as it can interfere with treatment.
Weight loss can also help with, as excess weight places stress on the joints. Choosing certain foods that may help reduce inflammation such as some Mediterranean diet staples like fish, whole grains and fresh fruits and vegetables can also help.
Early Detection And Diagnosis
As with most diseases, early detection and diagnosis are crucial for being able to treat symptoms, manage pain, and slow progression. An early diagnosis of RA can help you and your team of physicians and specialists put together an individualized treatment plan so that you can continue living a high quality of life.
Early on, you will want to discuss your case with a rheumatologist or RA specialist who can provide you with the treatment you need to delay the diseases progression. Generally, early diagnosis treatment is aggressive and targeted to properly manage the disease and prevent it from progressing.
If your RA was diagnosed in the early stage when symptoms first appeared, your chances of achieving longer periods of remission typically increase drastically. Thats not to say you wont experience flare-ups. Early diagnosis simply helps manage the disease and cannot guarantee the complete elimination of symptoms.
Read Also: Is Banana Good For Rheumatoid Arthritis
How To Know If Your Ra Is Progressing
You will know your joints will tell you, Dr. Bhatt says. The pain will get worse and you could have more swelling. Dr. Lally says that although periods of pain may resolve on their own in early RA, these episodes tend to become more frequent and longer in duration until the classic features of RA persist. In addition, Dr. Bhatt says to pay attention to non-joint symptoms like increased shortness of breath or red, painful eyes, which could be signs the RA is affecting other systems in the body. Let your doctor know if your RA symptoms are changing at all.
Causes And Risk Factors
RA is caused when the immune system attacks healthy joint tissues. Researchers dont know what causes the immune system to attack the synovium, the lining of the joints. But this process causes inflammation that can destroy bone and cartilage, stretching and weakening tendons and ligaments.
This leads to pain and loss of joint shape and alignment.
Recommended Reading: What Helps Lower Back Arthritis
What Are The Risk Factors For Ra
Researchers have studied a number of genetic and environmental factors to determine if they change persons risk of developing RA.
Characteristics that increase risk
- Age. RA can begin at any age, but the likelihood increases with age. The onset of RA is highest among adults in their sixties.
- Sex. New cases of RA are typically two-to-three times higher in women than men.
- Genetics/inherited traits. People born with specific genes are more likely to develop RA. These genes, called HLA class II genotypes, can also make your arthritis worse. The risk of RA may be highest when people with these genes are exposed to environmental factors like smoking or when a person is obese.
- Smoking. Multiple studies show that cigarette smoking increases a persons risk of developing RA and can make the disease worse.
- History of live births. Women who have never given birth may be at greater risk of developing RA.
- Early Life Exposures. Some early life exposures may increase risk of developing RA in adulthood. For example, one study found that children whose mothers smoked had double the risk of developing RA as adults. Children of lower income parents are at increased risk of developing RA as adults.
- Obesity. Being obese can increase the risk of developing RA. Studies examining the role of obesity also found that the more overweight a person was, the higher his or her risk of developing RA became.
Characteristics that can decrease risk
Who Should Diagnose And Treat Ra
A doctor or a team of doctors who specialize in care of RA patients should diagnose and treat RA. This is especially important because the signs and symptoms of RA are not specific and can look like signs and symptoms of other inflammatory joint diseases. Doctors who specialize in arthritis are called rheumatologists, and they can make the correct diagnosis. To find a provider near you, visit the database of rheumatologistsexternal icon on the American College of Rheumatology website.
You May Like: Are Eggs Bad For Psoriatic Arthritis