Inflammatory Arthritis Vs Osteoarthritis
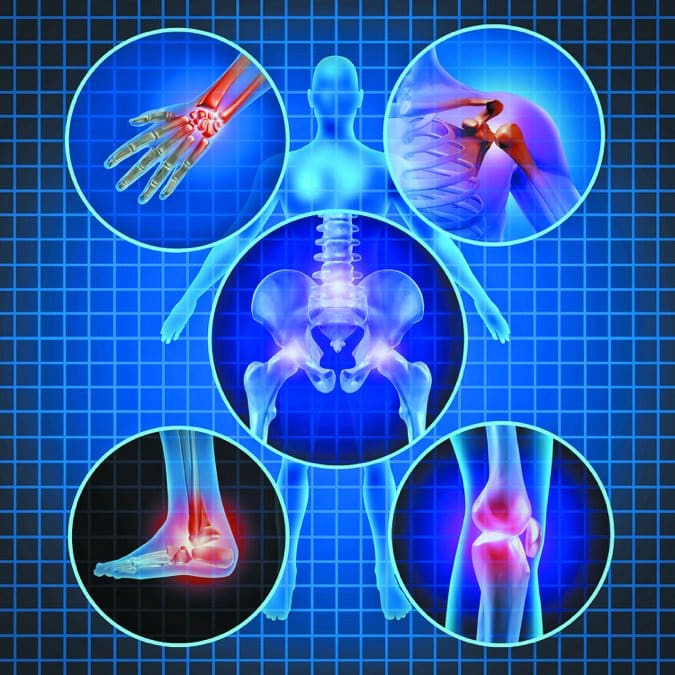
Arthritis actually describes over 100 different conditions that affect joints and the surrounding tissue. They fall into two main categories: inflammatory arthritis and osteoarthritis .
Inflammatory arthritis is a systemic disease in which the mechanisms that normally protect your body attack your own joints and tissues instead. The most well-known example is rheumatoid arthritis , which tends to be symmetrical, meaning youll have problems in the same joints on both sides of your body, like both wrists or both knees.
The second type of arthritis and the most common form is osteoarthritis. A degenerative disorder, its caused by trauma or age-related wear and tear on your joints over time. OA is most likely to affect weight-bearing joints such as the knees, hip, lower spine or big toe, but it can also cause pain and stiffness in your thumb or finger joints.
What Is Osteoarthritis Of The Foot And Ankle
Osteoarthritis is the most common type of arthritis. It mostly affects the hands, knees, hips and spine, but it can happen in any joint in the body, including the feet and ankles.
A joint is a part of the body where two or more bones meet. Your ankle joint is where the tibia and fibula bones in your leg join up with your foot. There are 33 joints in the foot, but the big toe is the one that is most commonly affected by osteoarthritis.
The joints in your body go through a normal cycle of damage and repair during your lifetime. But sometimes the process your body goes through to repair joints can change their shape or structure. When these changes happen in one or more of your joints, its called osteoarthritis.
The ends of our bones are covered in a tough but slippery surface, known as cartilage. This allows the bones to move against each other. The bones are held in place by ligaments. Tendons attached to our muscles and bones help us to move around.
Osteoarthritis causes damage to the cartilage, which results in pain and swelling, and can sometimes mean the bones rub against each other as we move. Osteoarthritis doesnt just affect the cartilage, but can also cause damage to the bones, ligaments, tendons and lining of affected joints.
Osteoarthritis can affect anyone at any age, but its most common in people over 45. It affects more women than men. The risk of developing osteoarthritis is commonly linked to:
How Is Arthritis Diagnosed And Evaluated
When diagnosing arthritis, your doctor will likely do a complete physical examination of your entire body, including your spine, joints, skin and eyes. You may undergo blood tests to detect markers of inflammation. In cases where an infection or gout is suspected, it may be useful to draw some fluid from a joint with a needle in order to analyze the contents of the material. In addition, your physician may order one or more of the following imaging tests:
Also Check: Is Rheumatoid Arthritis Worse Than Osteoarthritis
Ways To Live Better With Arthritis
Living with arthritis can be disruptive and disconcerting. The pain and stiffness can make it difficult to perform the daily tasks most people take for granted. Even things like putting on socks or cooking dinner can be exhausting. Therefore, if you have arthritis, it is important to take especially good care of yourself to relieve pain, improve function, and cope with difficult emotions. In fact, the American College of Rheumatology recommends not only medication but also nondrug treatments for people with osteoarthritis of the hip and knee. These methods include weight loss, physical therapy, and complementary therapies, such as acupuncture and massage.
It makes sense that eating healthful foods, shedding pounds if you are overweight, strengthening your muscles, and learning to move your joints safely are helpful regardless of which form of arthritis you have and which joints are affected. Further, paying attention to diet, weight, and exercise is important for preventing heart disease, which has been linked to rheumatoid arthritis and lupus.
Following are some do-it-yourself strategies and therapies that can help you conserve energy, protect your joints, accomplish daily tasks more easily, and adapt to lifestyle disruptions.
Foot And Ankle Arthritis
How it happens: The foot hitting any surface puts a high degree of contact stress on arthritic jointsevery step hurts. The pain can be quite excruciating if a joint is damaged, says Irvin Oh, MD, chief of Yale Medicine Orthopaedic Foot & Ankle Surgery. Range of motion becomes limited, and bone spurs can develop. Pain is common in the big toe, on the top of the foot, and in the ankle.
Self-care: Keep your weight under control, as being overweight or having obesity puts stress on the foot and ankle. Modify your activity if overuse seems to be exacerbating the pain, and try ice packs. Ankle-strengthening exercises and Achilles-stretching exercises can also help reduce pain. Talk to your doctor about using NSAIDs.
How a specialist can help: We always have to think of evenly distributing mechanical load, says Dr. Oh. He compares the foot and ankle to a tripod and says it must be well-balanced to be optimized for even the most basic functions, like taking a step. Some people with foot arthritis will compensate to avoid feeling pain and that can throw off the balance, he adds. Supportive shoes, an ankle brace, and orthotics may help.
Replacing or fusing arthritic joints may also be recommended. “There are innovative joint replacement options for such surgical treatments as toe implants and total ankle replacements for people whose joints are severely damaged or who have no cartilage left,” he says. We always try to preserve native joints as much as possible.
Recommended Reading: What Do You Do For Arthritis In Your Fingers
Treatment For Gout In The Heel
There is no cure for gout, but treatment to limit attacks and control painful symptoms are available.
If your doctor diagnoses gout, they will most likely suggest medication and certain lifestyle changes based on findings in the testing and your current health.
Certain medications treat gout attacks or flare-ups. Others reduce the risk of potential gout complications.
Also Check: Can You Get Rheumatoid Arthritis In Your Back
Heel Bursitis: Causes And Treatment
The full name for the bursitis you get in the back of your heel, underneath the Achilles tendon, is retrocalcaneal bursitis. Thats a bit of a tongue-twister, so to refer to it as heel bursitis is also fine. It usually manifests as a pain in the back of the heel, accompanied by a puffiness of the painful area.
Ive also discussed this in more detail in this video:
The heel bursa is the little blue sac in the image below. It is filled with fluid and sits between your Achilles tendon and heel bone where the tendon goes over the bone. We have bursas all over the body wherever tendons are close to one another and where a tendon is close to bone. Their function is to protect your tendons they prevent friction and absorb some of the compression forces.
You May Like: Hand Arthritis Remedies
Don’t Miss: How To Treat Arthritis In Your Hands
Cracking Or Popping Sounds
When you bend or straighten your knee, you may feel a grinding sensation or hear cracking or popping sounds. Doctors call this crepitus.
These symptoms can occur when youve lost some of the cartilage that helps with smooth range of motion. Both OA and RA can result in cartilage damage.
When cartilage is damaged, rough surfaces and bone spurs develop. As you move your joints, these irregular areas rub against each other.
Recommended Reading: 10 Rheumatoid Factor
Use Topical Medications For Arthritis In The Feet
Some people find that topical medications provide relief from foot arthritis pain, Frisch says. Look for topicals with capsaicin, an ingredient found in chile peppers thats believed to decrease the amount of substance P, which transmits pain in the body. Capsaicin is sold over the counter as a cream, ointment, stick, gel, lotion, liquid, or pad and under different brand names, such as Icy Hot and Zostrix.
Dont Miss: Arthritis Attack Symptoms
Read Also: What’s The Difference Between Psoriatic Arthritis And Osteoarthritis
Am I At Risk Of Osteoarthritis
Anyone who repetitively overuses their joints, including athletes, military personnel, and those with physically demanding jobs, may be at an increased risk of developing early-onset osteoarthritis.
Common symptoms of early-onset osteoarthritis include:
As osteoarthritis progresses, it can lead to increased joint inflammation and disability. With advanced stages of osteoarthritis, you may experience:
- Swelling: Osteoarthritis can cause swelling within joints as a result of joint inflammation that develops due to increased friction between bones from cartilage loss.
- Weakness: Osteoarthritis can cause weakness in the supporting muscles that surround joints. Because moving arthritic joints can be difficult and painful, people with osteoarthritis often avoid certain activities or movements, which leads to muscle atrophy and weakness from lack of muscle use. If one side of the body is affected by osteoarthritis, people will often compensate by using the other side of their body. This can lead to muscle weakness on the affected side from muscle disuse.
- Difficulty with daily functions: Due to acquired muscle weakness and decreased use of arthritic joints, advanced stages of osteoarthritis can lead to significant disability that impacts daily functioning. This can include activities of daily living that require fine motor movements of the hands or gross motor skills like walking and using the stairs.
- Carpometacarpal joint of the thumb
Chaunie Brusie Bsn Rn Rn Bsn
Sudden arthritis is not a real medical condition, but the symptoms of arthritis namely, joint pain and swelling can develop very abruptly in some people, according to the Centers for Disease Control and Prevention .
Video of the Day
Arthritis can also come and go, so you could feel tip-top one day and wake up feeling sore and achy the next.
Heres more on why arthritis might seem to come on all of a sudden, including when you should call a doctor about your symptoms.
You May Like: How To Get Diagnosed With Rheumatoid Arthritis
How Does Osteoarthritis Affect Young People
While 25 percent of people develop symptomatic OA at some point during their lives, some develop it earlier than others. Around 30% of osteoarthritis cases happen in people under 40. Some children even develop osteoarthritis, though this is exceedingly rare.
Having OA as a teen or young adult can be especially challenging. Everyone with OA suffers from similar symptoms. But teens and young adults are at a different period in their lives. Many feel
ostracized from sports and other social activities, and certain jobs may feel out-of-reach. And teens and young adults are more likely to develop mental health issues related to their diagnosis.
If you feel stressed, worried, sad, or anxious about your OA diagnosis, you should contact your doctor or mental health provider. While osteoarthritis is often a lifelong condition, proper management reduces symptoms and improves your quality of life.
What causes osteoarthritis in young people?
Most young adults don’t get osteoarthritis from repetitive wear-and-tear like older adults. The majority of osteoarthritis cases in young adults can be put down to one of the following:
-
Joint injuries from high-impact sports, motor vehicle accidents, or falls
-
Genetic joint malformations
While young adults often suffer from the same symptoms as older adults, they tend to have a higher pain tolerance, and this often leads to delayed diagnosis.
I Thought I Was Too Young For Arthritis I Was Wrong
When I hobbled into the office of a sports doctor in October, I had already considered some of the reasons my foot might be hurting. I had recently started running again after many years away from the sport, and I figured it could be a strained ligament, an inflamed tendon or plantar fasciitis, which ended my marathon-running habit more than a decade ago.
The diagnosis I received was something I had never considered: osteoarthritis. Just a few months shy of 40 at the time, I thought I was too young to have the kind of joint degeneration that, I had always assumed, tended to afflict people much later in life.
Disheartened, I discovered Im not alone.
Although osteoarthritis, often called OA, ordinarily shows up after age 65, its not uncommon for younger people to show signs of wear in their cartilage. This shock-absorbing connective tissue cushions the spaces where bones meet and allows those bones to slide easily as they move.
OA may be growing more common, given that medical costs related to the condition have risen. A variety of factors, including obesity, genetics and sports injuries, can explain why some people get the condition early.
And even though the diagnosis initially struck me as a sign that I was doomed to a future of progressive deterioration and decline, it turns out there are plenty of ways to manage arthritis when it strikes relatively early in life. Those strategies rarely require replacing joints or quitting favorite activities.
Also Check: How To Know If You Have Arthritis In Your Back
Here’s How You Can Stay Healthy With Psoriatic Arthritis In Your Twenties And Beyond
A diagnosis of psoriatic arthritis in your twenties doesnt mean you cant enjoy a fun-filled and active life. Here are some strategies that can help you manage your disease, and not feel like you are missing out.
- Stick to your treatment plan. When I think about my patients who seem to be managing their psoriatic arthritis most successfully, it tends to be the people who are keeping their appointments and taking their medications as directed, says Snyder. Its not always easy to remember what you need to take and when you need to take it, but committing to that makes a big difference.
- Communicate with your doctor. In psoriatic arthritis, you can have periods where youre doing great, but there can also be flares, Snyder notes. Be sure to let your physician know when your skin or joints start acting up. Were here and we can help, but we dont know that’s happening if you dont communicate with us, she explains.
- Keep a flexible mindset. Psoriatic arthritis can be unpredictable. Whenever possible, try not to have rigid expectations of how each day has to be. Then if its a good day, you can accomplish more of what you were hoping to do, says Anderson. Try to be sensitive to yourself and mindful of how things are going, and take each day or hour as it comes.
Meleney seconds that advice, adding, When you lie to yourself about how you are feeling and push through it, three days later youre not going to be able to get out of bed.
Whats The Outlook For Someone Living With Arthritis
Since theres no cure for arthritis, most people need to manage arthritis for the rest of their lives. Your healthcare provider can help you find the right combination of treatments to reduce symptoms. One of the biggest health risks associated with arthritis is inactivity. If you become sedentary from joint pain, you may face a greater risk for cancer, heart disease, diabetes and other serious conditions.
Also Check: High Rheumatoid Levels
Don’t Miss: How Is Rheumatoid Arthritis Causes
What Are The Types Of Arthritis Of The Knee
There are around 100 types of arthritis. The most common types that might affect your knees include:
- Osteoarthritis is the most common of the types on this list. Osteoarthritis wears away your cartilage the cushioning between the three bones of your knee joint. Without that protection, your bones rub against each other. This can cause pain, stiffness and limited movement. It can also lead to the development of bone spurs. Osteoarthritis gets worse as time passes.
- Post-traumatic arthritis is a type of osteoarthritis. The cartilage starts thinning after trauma to your knee . Your bones rub together, and that causes the same symptoms as osteoarthritis: pain, stiffness and limited movement. Your knee arthritis symptoms might not start until years after the trauma.
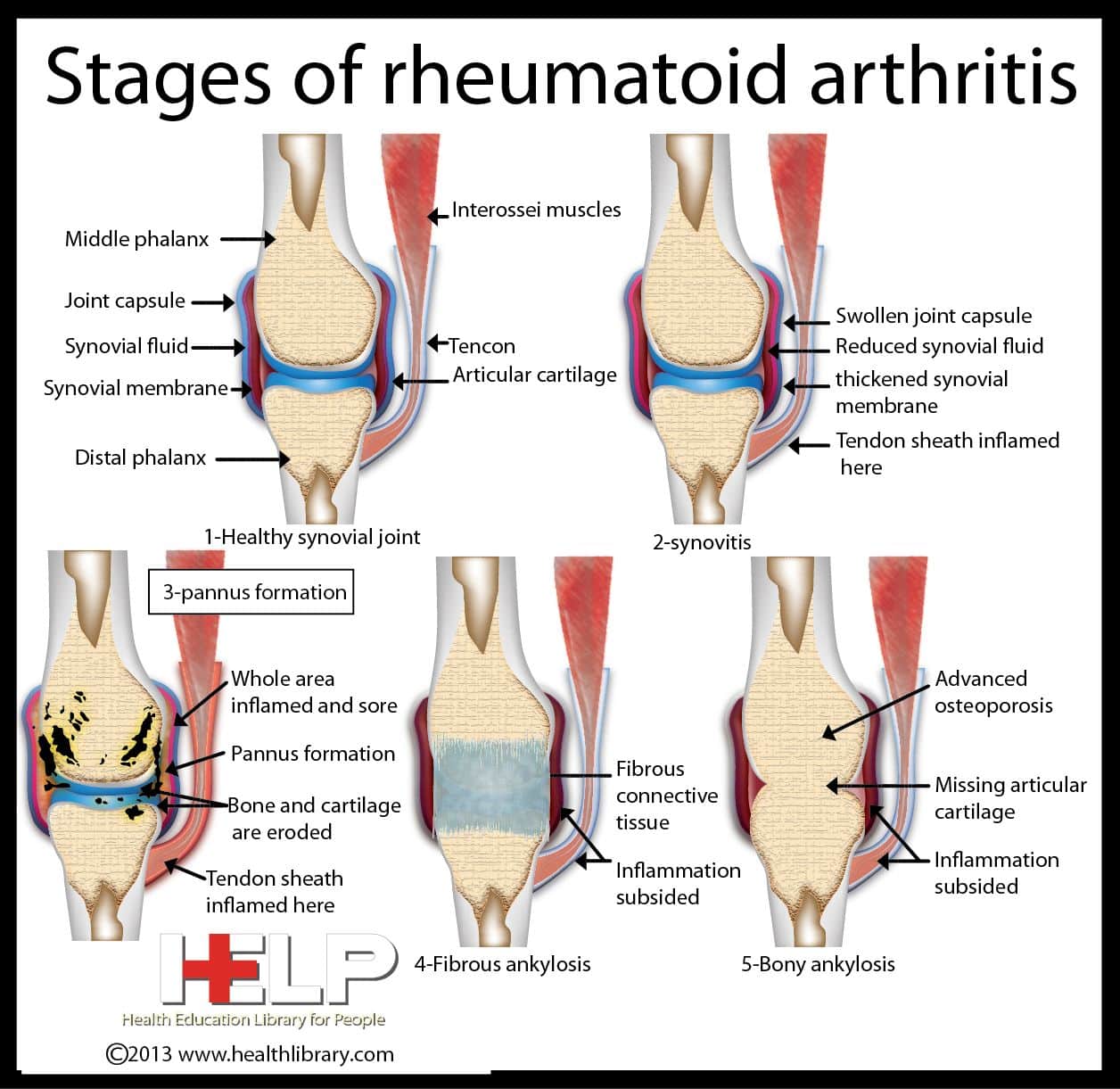
- Rheumatoid arthritis is an autoimmune disease. A healthy immune system causes inflammation when its trying to protect you from an infection, injury, toxin or another foreign invader. The inflammatory response is one way your body protects itself. If you have rheumatoid arthritis, you have an unhealthy immune system that triggers inflammation in your joints even though theres no foreign invader. The inflammation causes pain, stiffness and swelling of the synovial membrane, which can also wear away your cartilage.
When Conservative Treatments Arent Enough
If the treatments above dont help, or your arthritis continues to get worse, Dr. Berg may recommend surgery for your feet or ankles.
One procedure Dr. Berg may recommend is fusion surgery. With this surgery, Dr. Berg fuses specific bones together with pins, rods, plates, or screws. Another procedure Dr. Berg may recommend is joint replacement therapy. With this surgery, your damaged joints are removed and replaced with artificial joints made out of metal or plastic.
If you have arthritis in your feet or ankles, or if you want to see if you do and want to learn about treatment options, book an appointment online or over the phone with Intermountain Foot & Ankle Associates today.
You Might Also Enjoy
You May Like: Whats Good For Arthritis In Your Hands
You May Like: Is Orange Good For Arthritis
What Can I Do To Make Living With Arthritis Easier
Changing your routine can make living with arthritis easier. Adjust your activities to lessen joint pain. It may help to work with an occupational therapist . An OT is a healthcare provider who specializes in managing physical challenges like arthritis.
An OT may recommend:
Recommended Reading: Are Lemons Good For Arthritis