What Are The Symptoms
Psoriatic arthritis can affect any joint in the body and symptoms can vary from person to person. It can develop slowly with mild symptoms, or come on quickly and be severe. The most common symptoms are:
- pain, swelling and stiffness in one or more joints
- pain and stiffness in the buttocks, lower back or neck
- pain in tendons, such as at the back of the heel or sole of the foot
- changes in nails, such as thickening, colour change or separation from the skin
- pain and redness in the eyes.
How To Stay Safe
To minimize your risk of COVID-19, the Centers for Disease Control and Prevention advises those who may be at increased risk to:
- Stay home as much as possible.
- Avoid crowds and limit close contact with other people in public .
- Avoid touching your eyes, nose, or mouth in public.
- Disinfect or avoid touching frequently used surfaces in public places, such as doorknobs, elevator buttons, and shopping carts.
- Wash your hands with soap and water for 20 seconds or use an alcohol-based hand sanitizer to clean your hands after going outside or touching public surfaces.
Symptoms of COVID-19 may appear between two and 14 days after exposure, and can include:
- Cough
- Loss of taste or smell
- Sore throat
- Congestion
- Fatigue
If you have any of these symptoms, it is best to get a COVID-19 test to determine if you have been infected. You can visit the website of your local or state health department to find a testing location near you. COVID-19 tests are typically covered by your health insurance or free if you are uninsured.
Cannabidiol Was Not Found To Help With Psa Pain
Whats New Cannabidiol is increasingly sold in stores and websites, and is discussed in many online chat groups as a potentially useful way to deal with pain, including for PsA.
But while patients were asking Jonathan Vela, MD, a rheumatologist at Aalborg University Hospital in Denmark, whether they should take it for their condition, he didnt have an answer. I first heard about CBD in 2017, but at that time no proper study had been done, making it hard to counsel patients, he says.
So Dr. Vela set out to study it. What he and his colleagues eventually found is that people taking CBD had no better response than the placebo.
Research Details The study enrolled 136 people with PsA or osteoarthritis . Half were told to take 20 to 30 mg of synthetic CBD daily for three months the rest swallowed a placebo during that time.
When people were evaluated at the end of the clinical trial, no statistically significant differences were found between the two groups for pain intensity, sleep quality, depression, anxiety, or pain catastrophizing.
Why It Matters Like other therapies, it is important for research to prove the effectiveness of any treatment before people decide to take it.
Although theres a lot of buzz around CBD, at present there is no proper study showing the effect of CBD for pain relief if you have psoriatic arthritis, Vela says.
Also Check: How To Get Rid Of Arthritis In Knees
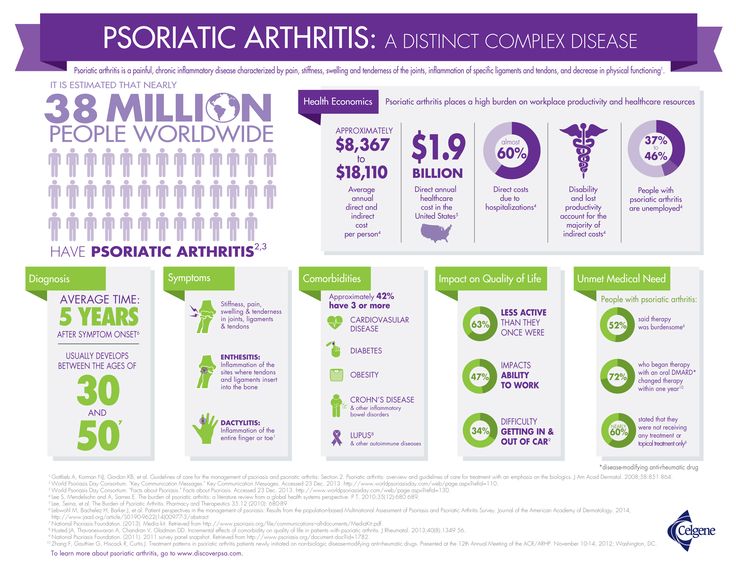
How Common Is Psoriatic Arthritis
- print page
- Bookmark for later
Estimates vary on how many people with psoriasis go on to develop psoriatic arthritis , in part because the disease presents with a wide variety of symptoms among patients and diagnosis may be missed or delayed.1,2 Studies have shown that anywhere between 5 percent to 30 percent of people with psoriasis eventually develop psoriatic arthritis.3 On the other hand, 85 percent of people with PsA also have psoriasis.3 Reports of the incidence of psoriatic arthritis vary between 6 percent and 42 percent, noting that the lower estimates may reflect a missed diagnosis or misdiagnosis .2,4
Identification Of Risk Factors
Risk factors for the development of PsA in psoriasis patients were determined by conditional logistic regression analysis in sex- and age-matched populations using nearest neighbour matching in a ratio of one to four . Using a multivariate regression model, risk factors for development PsA within 4 years of the first psoriasis diagnosis were evaluated. Patients were separated into two groups: patients developing PsA by 31 December 2017 after the first psoriasis diagnosis were assigned to the PsA group , and patients who did not develop PsA by 31 December 2017 after first diagnosis of psoriasis were assigned to the control group . Risk factors for the development of concomitant PsA were identified and their effect size was quantified. All potential risk factors before the first diagnosis of PsA were considered. For the multivariate model, parameters such as the P-value for every individual comorbidity, odds ratio, relative risk, 95% CIs, goodness of fit and percentages of the comorbid diseases in each group were calculated.
Also Check: How To Prevent Rheumatoid Arthritis In Hands
Who Develops Psoriatic Arthritis
About 1 person in 10 with psoriasis develops psoriatic arthritis. About 2 in 100 people develop psoriasis at some stage in their lives.
In most cases, the arthritis develops after the psoriasis â most commonly within 10 years after the psoriasis first develops. However, in some cases the arthritis develops much later. In a small number of cases the arthritis develops first, sometimes months or even years before the psoriasis develops. Men and women are equally affected.
Psoriasis most commonly first occurs between the ages of 15 and 25 and psoriatic arthritis most commonly develops between the ages of 25 and 50. However, both psoriasis and psoriatic arthritis can occur at any age, including in childhood.
Note: people with psoriasis also have the same chance as everyone else of developing other types of arthritis such as rheumatoid arthritis and osteoarthritis. Psoriatic arthritis is different, and is a particular type of arthritis that occurs only in some people with psoriasis.
Active Psoriatic Arthritis Improves With The Monoclonal Antibody Drug Risankizumab
Whats New Two studies presented at the conference found that risankizumab is effective against PsA. Currently the prescription injectable drug is approved only to treat adults with plaque psoriasis.
In the randomized clinical trials, considered the best way to evaluate a drug, people with PsA reduced the severity of their disease by taking this medication.
Research Details Both studies were part of a research effort known as KEEPsAKE, conducted by an international team of scientists working with the manufacturer.
One study, known as KEEPsAKE 2, involved 443 adults with active cases of PsA who had not been sufficiently helped by prior disease modifying drugs or one or two biologic therapies. Half received a 150 milligram shot of risankizumab at the start of the trial, one month later, and three months after that. The other group received placebo injections.
More patients reported an improvement in their symptoms after taking risankizumab, regardless of what drugs they might have taken in the past.
The second study combined results from KEEPsAKE 1 and 2. It included 1407 people with active disease who had not found relief with prior meds and who were randomized to the same study protocol.
When everyone was evaluated six months after starting the study, people taking risankizumab were again more likely to have significant improvements with their disease.
Don’t Miss: Rheumatoid Arthritis Upper Back Pain
Keep An Exercise Diary
Pay attention to your symptoms after a workout and jot down how youre feeling, says Scholl. You may notice a pattern and realize something doesnt work well for your body.
If you feel that you have an exercise-induced injury, allow the joint to rest and ice it consider calling your doctor if the pain persists. Exercise diaries are also helpful in tracking your progress and keeping you motivated to achieve more.
Most Rheumatologists And Public Health Experts Want People Living With Rheumatic Diseases Like Psoriatic Arthritis To Get The Vaccine As Soon As They Can
Learn more about our FREE COVID-19 Patient Support Programfor chronic illness patients and their loved ones.
If you live with psoriatic arthritis, an inflammatory and autoimmune form of arthritis that affects about 30 percent of people with psoriasis, you may understandably have many questions and concerns about getting the COVID-19 vaccine.
Heres the bottom line: Especially if you have an autoimmune condition like psoriatic arthritis, most rheumatologists and public health experts recommend you get vaccinated against COVID-19. In its COVID-19 Task Force Guidance, the National Psoriasis Foundation says that in most cases, patients with psoriatic disease who dont have contraindications should take the first authorized COVID-19 vaccine that becomes available to them.
Similarly, the American College of Rheumatology states that autoimmune and inflammatory rheumatic disease patients , which includes people with psoriatic arthritis, should receive the vaccine when theyre eligible.
The ACR also states that disease activity and severity should not delay you from getting the vaccine except in extreme cases . That said, vaccination would ideally take place in the setting of well-controlled disease.
Heres everything you need to know about getting the COVID-19 vaccine if you have psoriatic arthritis.
You May Like: Ra Hand Pain Relief
What Is Psoriatic Arthritis Video
Psoriatic arthritis can cause pain, swelling and stiffness in and around your joints.
It usually affects people who already have the skin condition psoriasis . This causes patches of red, raised skin, with white and silvery flakes.
Sometimes people have arthritis symptoms before the psoriasis. In rare cases, people have psoriatic arthritis and never have any noticeable patches of psoriasis.
Psoriatic arthritis and psoriasis are autoimmune conditions. Our immune system protects us against illness and infection. In autoimmune conditions, the immune system becomes confused and attacks healthy parts of the body.
Both conditions can affect people of any age.
Its estimated that around one in five people with psoriasis will develop psoriatic arthritis.
People with psoriasis are as likely as anyone else to get other types of arthritis, such as osteoarthritis or rheumatoid arthritis. These conditions are not linked to psoriasis.
Psoriatic arthritis is a type of spondyloarthritis. These are a group of conditions with some similar symptoms.
Do We Know What Causes Psoriatic Arthritis
- The cause of psoriatic arthritis is the subject of much research.
- You cannot catch psoriatic arthritis or psoriasis from someone else. Therefore they are not contagious.
- The cause of psoriatic arthritis is not proven but experts believe it to be a combination of genetic, immunological and environmental factors. 2 out of 5 people with psoriasis or psoriatic arthritis have a first-degree relative with the condition. This means you have a higher chance of developing psoriasis or psoriatic arthritis if you have relative who has the condition. Some experts believe infections such as streptococcal infections may provoke psoriatic arthritis, though this is not proven.
- The role of bacteria in the gut and developing psoriatic arthritis is the subject of current research.
- Trauma and stress may be contributing factors, although this is not proven.
- The genetic make-up of an individual is likely to determine the risk of developing psoriasis and psoriatic arthritis and probably influences the severity.
- Being overweight is now understood to be linked to developing psoriatic arthritis and is the subject of ongoing research.
- There are certain genetic markers linked to the immune system which are now being used to predict the severity of psoriatic arthritis. Much more is known about the mechanisms that lead to inflammation in other conditions and it is likely advances in science will lead to much more effective treatments with fewer side effects.
Read Also: Rh Arthritis Treatment
Why Exercise Is Important For Psoriatic Arthritis
You can exercise with PsA, and you really should, says Kathryn Dao, MD, Associate Professor, Division of Rheumatology, Department of Internal Medicine at University of Texas Southwestern in Dallas. One of the non-pharmacological treatments for PsA that is written into ACR /NPF guidelines is exercise.
The list of benefits is long: Exercise improves strength, reduces pain, improves range of motion, and provides other health benefits, says Dr. Dao. Here are a few more to consider:
Study Design And Data Source

This was a non-interventional retrospective analysis of insurance claims data using the Institute of Applied Health Research Berlin database . The InGef database is a complete, longitudinal claims data set of 7 million individuals between 2012 and 2017. Approximately 85% of the German population are insured by the statutory health insurance system. For the purpose of this study, InGef provided a representative subset of anonymized claims based on 4 million members of the SHI in Germany, which allows extrapolation of these epidemiological findings to the overall German adult population . All patient-level data in the InGef research database were de-identified. Use of this study database for health services research was therefore fully compliant with German federal law and, accordingly, ethical approval and informed consent were not needed. Besides information on demographic characteristics of insured individuals, the database provides patient data, including diagnostic codes, outpatient care, pharmacotherapy and medical devices, at an anonymized individual level .
Read Also: Rheumatoid Arthritis Over The Counter Medication
Treatment For Psoriatic Arthritis
Treatment for psoriatic arthritis aims to:
- relieve symptoms
- slow the condition’s progression
- improve quality of life
This usually involves trying a number of different medicines, some of which can also treat the psoriasis. If possible, you should take 1 medicine to treat both your psoriasis and psoriatic arthritis.
The main medicines used to treat psoriatic arthritis are:
- non-steroidal anti-inflammatory drugs
- biological therapies
Work And Psoriatic Arthritis
Having psoriatic arthritis may make some aspects of working life more challenging. But, if youre on the right treatment, its certainly possible to continue working.
Help and support is available, and you have rights and options.
The Government scheme Access to Work is a grant that can pay for equipment to help you with activities such as answering the phone, going to meetings, and getting to and from work.
The 2010 Equality Act, and the Disability Discrimination Act in Northern Ireland makes it unlawful for employers to treat anyone with a disability less favourably than anyone else. Psoriatic arthritis can be classed as a disability if its making every-day tasks difficult.
Your employer may need to make adjustments to your working environment, so you can do your job comfortably and safely.
You might be able to change some aspects of your job or working arrangements, or train for a different role.
In order to get the support youre entitled to, youll need to tell your employer about your condition. Your manager or HR department might be a good place to start.
Other available support might include:
- your workplace occupational health department, if there is one
- an occupational therapist. You could be referred to one by your GP or you could see one privately
- disability employment advisors, or other staff, at your local JobCentre Plus
- a Citizens Advice bureau particularly if you feel youre not getting the support youre entitled to.
Read Also: Medical Term Arthritis
How Many People Get Psoriatic Arthritis
ANSWER
Up to a third of people with psoriasis also get psoriatic arthritis. It usually affects people between ages 30 and 50, although you can get it at any age. It causes inflammation, mainly in your joints. It can also affect other parts of your body.
National Institute of Arthritis and Musculoskeletal and Skin Disorders: “Roundtable Discussion on Psoriasis, Psoriatic Arthritis, and Rheumatoid Arthritis.”
National Institute of Arthritis and Musculoskeletal and Skin Disorders: “Roundtable Discussion on Psoriasis, Psoriatic Arthritis, and Rheumatoid Arthritis.”
THIS TOOL DOES NOT PROVIDE MEDICAL ADVICE. It is intended for general informational purposes only and does not address individual circumstances. It is not a substitute for professional medical advice, diagnosis or treatment and should not be relied on to make decisions about your health. Never ignore professional medical advice in seeking treatment because of something you have read on the WebMD Site. If you think you may have a medical emergency, immediately call your doctor or dial 911.
This tool does not provide medical advice. See additional information.
Other Answers On:
Proactive Management Of Psa
If you have been diagnosed with psoriatic arthritis, taking the following actions can help you manage the condition, limit the number of flares you experience, and improve your quality of life:
- Medications
- Manage stress
Medications
Systemic treatments can help you manage disease activity and prevent flares from occurring. Disease-modifying antirheumatic drugs like methotrexate, biologics, and immunomodulators may all be used to manage psoriatic arthritis.
Know Your Triggers
Psoriatic arthritis can have many different triggers. These triggers can vary from person to person. One of our members said, I find that stress is my main trigger, while another shared that coffee triggers a flare-up. The key is to get to know which triggers cause PsA flare-ups for you.
You may want to keep a diary that tracks everything from the foods you eat to the temperature and the weather. Logging your PsA symptoms alongside these factors may help you identify what leads to or worsens your symptoms. Once you know your triggers, you can do your best to avoid them or limit their impact on your life.
Exercise Regularly
After having been recommended specific exercises by a health care provider, one member shared, The exercises are really helping!
Practice Sun Protection
Avoid Injury
Manage Stress
Recommended Reading: Living With Rheumatoid Arthritis In Your 30s
What Are Psoriatic Arthritis Co
Another Psoriatic Arthritis complication is psoriatic psoriasis, which Psoriatic Arthritis definition is similar to psoriasis that affects areas of your body other than your joints.
For Psoriatic Arthritis diagnosis, psoriatic psoriasis Psoriatic Arthritis requires psoriasis in at Psoriatic Arthritis examples least two psoriasis areas for Psoriatic Arthritis treatment psoriasis 6 months or longer.
Psoriasis can affect your skin, fingernails, and toenails.
Genetic Markers Of Psoriatic Arthritis
In the last 3 years, significant progress has been made toward identifying genetic markers associated with psoriatic arthritis. However, most of these markers are also associated with psoriasis, and thus a major remaining challenge is to identify genetic risk factors that are specific to psoriatic arthritis.
HLA locus
The HLA locus contains many genes responsible for immunologic function in humans. Psoriasis and psoriatic arthritis demonstrate human leukocyte antigen associations, most frequently with HLA-Cw6., However, the HLA region may potentially harbor multiple genes that are associated with psoriasis and psoriatic arthritis. For psoriasis, Feng et al. recently identified three independent signals near the HLA locus that contribute to psoriasis risk: HLA-Cw6, c6orf10, and the region between HLA-B and MICA.
Although psoriatic arthritis is most strongly associated with HLA-Cw6, other HLA markers have also been associated with it. The frequency of HLA-B27 is reportedly higher among patients with psoriatic arthritis.,, Gladmann and Farewell performed a univariate analysis of psoriatic arthritis patients and showed that HLA-B27, HLA-B39, and HLA-DQw3 antigens were associated with psoriatic arthritis disease progression, whereas HLA-DR7 was protective. Additionally, the presence of HLA-B39 suggested early progression in psoriatic arthritis.
MICA locus
Other genetic loci
Also Check: Can Osteoarthritis Turn Into Rheumatoid Arthritis