What Is The Safest Drug For Rheumatoid Arthritis
The safest drug for rheumatoid arthritis is one that gives you the most benefit with the least amount of negative side effects. This varies depending on your health history and the severity of your RA symptoms. Your healthcare provider will work with you to develop a treatment program. The drugs your healthcare provider prescribes will match the seriousness of your condition.
Its important to meet with your healthcare provider regularly. Theyll watch for any side effects and change your treatment, if necessary. Your healthcare provider may order tests to determine how effective your treatment is and if you have any side effects.
Rheumatoid Arthritis And Osteoarthritis
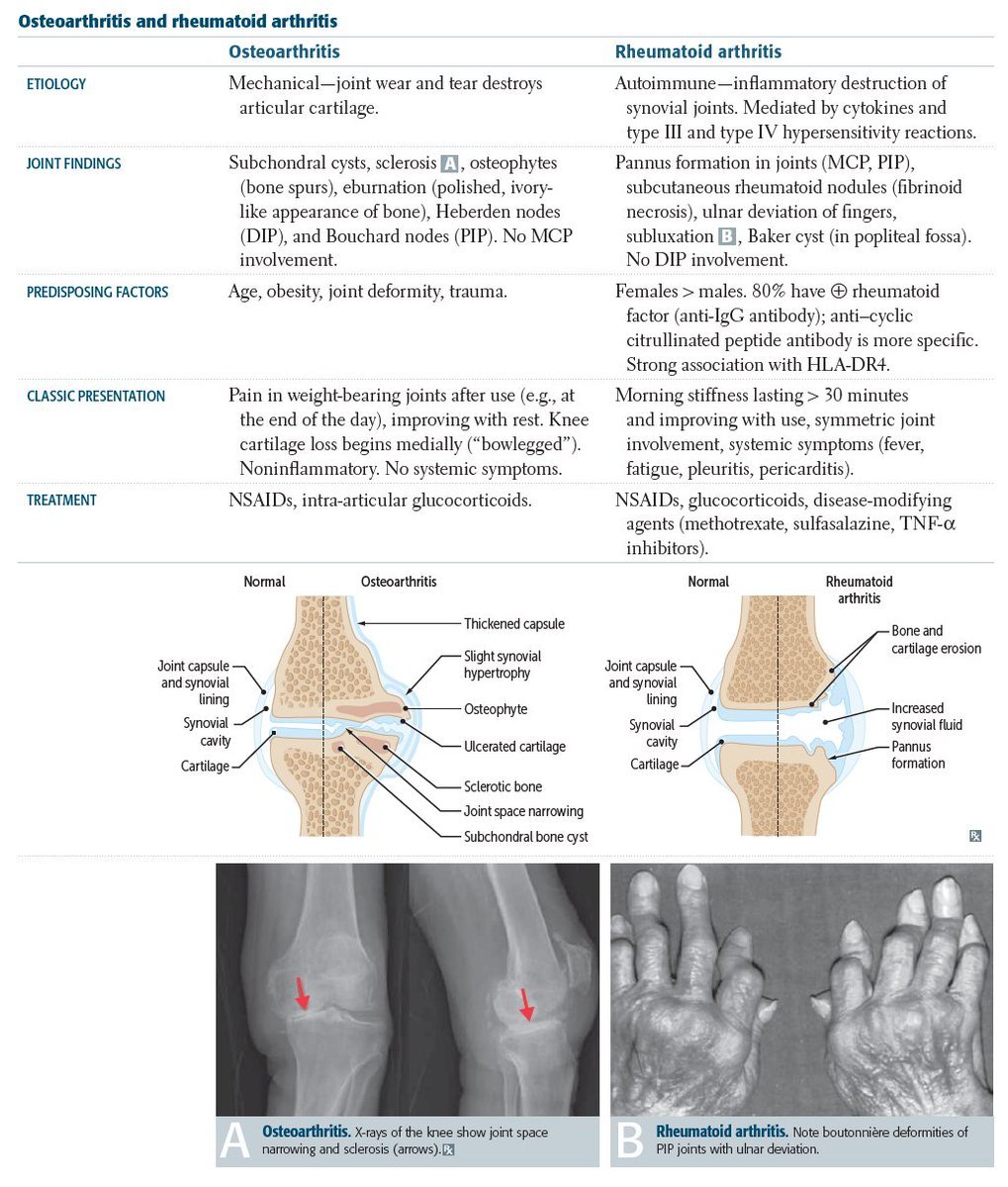
The word arthritis simply means inflammation of the joint. The reasons for that inflammation, however, varies. In the case of osteoarthritis, the cause is wear and tear. RA is an auto-immune condition, meaning that the immune system, normally there to protect us, is attacking healthy the joints.
Until I was diagnosed, I thought that arthritis was just something that old people get.
Until you or someone close to you is diagnosed with rheumatoid arthritis , unfortunately, this is most peoples perception of the disease. This is, at least in part, because many people, including some healthcare professionals, still refer to osteoarthritis as arthritis. So whats the difference?
One third of people over the age of 45 in the UK have sought treatment for osteoarthritis, whereas RA affects a much smaller number, at around 1% of the UK population.
There are also differences between the joints affected by these two conditions. Rheumatoid arthritis tends to affect joints symmetrically, most commonly the small joints of the hands and feet. Multiple joints may be affected, sometimes simultaneously, whereas OA will be isolated to individual joints. Osteoarthritis can affect the lower parts of the spine, and the finger joints closest to the nailbeds, both of which are areas of the body rarely affected in RA. RA can affect different joints at different times, whereas osteoarthritis doesnt come and go, although pain and stiffness can come and go.
Also Check: Arthritis Itchy Skin
Rheumatoid Arthritis: An Autoimmune Disease
Rheumatoid Arthritis, an autoimmune condition, is a less common type of arthritis. The immune system is the bodys first line of defence against illness and infections. When an individual is affected by an autoimmune disorder, the immune system wrongly attacks the healthy tissues of the body as it would a virus or bacteria. It primarily targets the joint lining and causing chronic inflammation. Several joints can be affected, and RA can even affect the bodys organs in some of the more serious cases.
Inflammation is a vital tool in a healthy immune response, when the immune system is working as it should. Extra fluids and blood are rushed to the specific area – such as the site of a wound – to assist in fighting an infection. In some cases, the skin surrounding a wound may turn a different colour and become swollen due to inflammation.
With RA, extra fluid and inflammation of the joints can lead to pain and mobility problems, or even lead to permanent joint damage. The disorder often begins in the hands and feet, and can build up gradually or start quite aggressively. RA can also affect adults of any age but the onset of the disease is most common in those between the ages of 40 and 60. Women are 2-3x more likely to suffer from rheumatoid arthritis than men.
Also Check: Can Arthritis Be Cured Permanently
Autoimmune Vs Degenerative Disease
As mentioned, rheumatoid arthritis is an autoimmune disease, in which the bodys white blood cells attack the cartilage in the joints, destroying the collagen structures, bones, and ligaments. As a result, fluid will accumulate in the joints, and lead to stiffness, pain, and swelling around them. Other autoimmune diseases also affect connective tissue, including lupus, scleroderma, mixed connective tissue disease, polymyalgia rheumatica, and ankylosing spondylitis.
Osteoarthritis deteriorates the cartilage that protects the joints, causing bones to rub together and expose nerves, which leads to pain. Other examples of degenerative diseases include osteoporosis, macular degeneration, and multiple sclerosis.
How Is Osteoarthritis Diagnosed
There is no single test to diagnose osteoarthritis. A diagnosis is based on factors like medical history, symptoms, and age. To diagnose osteoarthritis or rule out other conditions, your doctor may run one of the following tests:
- X-ray or other imaging tests
- A joint fluid analysis is known as arthrocentesis. During an arthrocentesis, joint fluid is removed and analyzed to determine the cause of pain and swelling.
Recommended Reading: Should You Eat Tomatoes If You Have Arthritis
How Is Osteoarthritis Treated
Osteoarthritis is usually treated with a combination of treatments and will depend on factors like age, occupation, medical history, and the severity of the disease. The goals of treatment are to reduce pain and other symptoms, improve joint function, and maintain quality of life. Treatment is also meant to stop or slow disease progression.
Treatment options may be non-pharmacologic, pharmacologic, complementary or alternative, or surgical. The safest and least invasive treatment options should be used first before moving on to more invasive and expensive options like surgery.
Non-pharmacologic options include exercise, weight loss, or bracing, and splinting to support painful joints.
Pharmacologic options include acetaminophen for mild osteoarthritis or non-steroidal anti-inflammatory drugs like aspirin or ibuprofen. Opioids are also an option for osteoarthritis pain, but because of the potential for abuse, they should only be used if patients dont respond to acetaminophen or NSAIDs.
Complementary or alternative treatments for osteoarthritis can include acupuncture or glucosamine and supplements like chondroitin and turmeric. This combination may help relieve arthritis pain by slowing down the deterioration of cartilage.
Surgery should only be considered when patients dont respond to other treatments. The most common surgery is a total joint replacement, a procedure in which parts of the damaged joint are removed and replaced with a ceramic, metal, or plastic prosthesis.
Natural Treatments For Arthritis
What about rheumatoid arthritis vs. osteoarthritis in terms of a treatment? The goal for both osteoarthritis and rheumatoid arthritis is to decrease pain, minimize damage, and improve function of the joints. Non-steroidal anti-inflammatory and corticosteroid drugs are the conventional method used for both conditions, while immunosuppressive drugs can help stop the immune system from attacking the joints in rheumatoid arthritis patients.
Supplements used for osteoarthritis include glucosamine sulfate, chondroitin sulfate, methylsulfonylmethane, S-Adenosylmethionine, vitamin K, boswellia, and devils claw. Rheumatoid arthritis supplements will include conjugated linoleic acids, manganese and superoxide dismutase, probiotics, bromelain, pancreatic enzymes, and hydrochloric acid. Other supplements for both conditions include curcumin, ginger, omega-3 fatty acids, vitamin C, vitamin D, and collagen.
Also Check: What Can You Take For Arthritis In Your Knees
Will Changing My Diet Help My Rheumatoid Arthritis
When combined with the treatments and medications your provider recommends, changes in diet may help reduce inflammation and other symptoms of RA. But it wont cure you. You can talk with your doctor about adding good fats and minimizing bad fats, salt and processed carbohydrates. No herbal or nutritional supplements, like collagen, can cure rheumatoid arthritis. These dietary changes are safer and most successful when monitored by your rheumatologist.
But there are lifestyle changes you can make that may help relieve your symptoms. Your rheumatologist may recommend weight loss to reduce stress on inflamed joints.
People with rheumatoid arthritis also have a higher risk of coronary artery disease. High blood cholesterol can respond to changes in diet. A nutritionist can recommend specific foods to eat or avoid to reach a desirable cholesterol level.
Is There A Possible Link Between The Contraceptive Pill And Rheumatoid Arthritis
Q) I would be very grateful for any information regarding the possible link between the contraceptive pill and rheumatoid arthritis. I have suffered from rheumatoid arthritis for nearly 40 years but it is relatively well-controlled with quadruple therapy including anti-TNF. I have two daughters in their 20s and I am very worried about the possibility of the contraceptive pill triggering RA. I read about this possible link over 35 years ago and immediately stopped taking the pill myself. Has any progress been made in research since then? I am very worried as both my daughters have recently started taking the pill. I feel terrible that I had not warned them of a possible risk.
A) There is a strong link between hormones and arthritis, and that includes both osteoarthritis and rheumatoid arthritis. Women, of course, have such dramatic surges and ebbs in hormone concentrations and this may explain the common occurrence of arthritis starting after pregnancy and the menopause. And it may be linked to the fact that rheumatoid arthritis is more common in women than men. In fact it is now thought that taking the contraceptive pill may be protective against developing rheumatoid arthritis, although reports are conflicting. The use of oral contraceptives may also reduce the severity of rheumatoid arthritis once it has developed. So I would not spend time worrying about your daughters.
This answer was provided by Dr Philip Helliwell in 2013, and was correct at the time of publication.
Also Check: What Are The Symptoms Of Psoriatic Arthritis In The Feet
How Do Treatment Options And Home Remedies For Osteoarthritis And Rheumatoid Arthritis Differ
For symptomatic OA, doctors commonly recommend over-the-counterpain relievers and sometimes fish oil or glucosamine chondroitin food supplementation. These include acetaminophen and also anti-inflammatory medications such as the NSAIDsibuprofen or naproxen in selected situations. There are no specific treatments for OA.
Doctors treat RA aggressively with medications that limit or stop the autoimmune inflammation. While over-the-counterpain relievers are sometimes used to supplement treatment, the basic treatment requires medications that must be monitored for benefit as well as any signs of toxicity. These medications include
Osteoarthritis Versus Rheumatoid Arthritis
Osteoarthritis is a degenerative condition where the cartilage in joints is damaged, disrupting the smooth gliding motion of the joint surfaces. The result is pain, swelling, and deformity that can worsen over time. The most common joints affected are knees, hips, spine, and hands. The pain of osteoarthritis increases with overuse and improves with rest.
Rheumatoid arthritis , on the other hand, is an inflammatory autoimmune disease that affects connective tissue throughout the body. The most common result is redness, swelling, and tenderness in the joints. RA symptoms and severity can vary significantly between people. Some may have mild symptoms over a short period of time and some may have more severe forms that last many years. RA may occur in cycles of remission with no symptoms and flare ups where symptoms are more severe.
Joints Affected by Osteoarthritis:
Rheumatoid Arthritis:
Recommended Reading: How To Know You Have Arthritis In Hands
What Are The Goals Of Treating Rheumatoid Arthritis
The most important goal of treating rheumatoid arthritis is to reduce joint pain and swelling. Doing so should help maintain or improve joint function. The long-term goal of treatment is to slow or stop joint damage. Controlling joint inflammation reduces your pain and improves your quality of life.
Which Symptoms Are Specific To Osteoarthritis
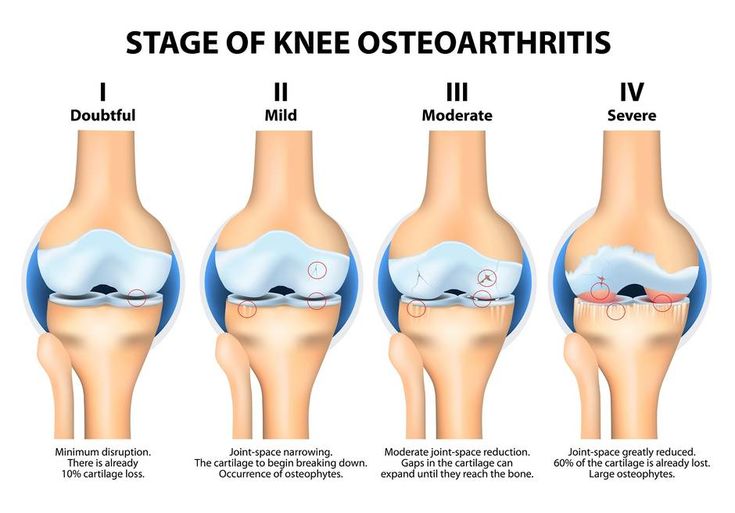
Osteoarthritis symptoms are limited to the affected joints, which may have an aching to burning sensation or experience sharp pain. It may lead to lumps under the skin near joints, but those spots are different than rheumatoid nodules. Osteoarthritis may result in bone spurs, which are excessive bone growth along the edges of arthritic joints.
Osteoarthritis isnt symmetrical, so its symptoms could include pain in one knee or worse pain in one side of the body than the other. It commonly manifests itself in the hand and fingers like rheumatoid arthritis. Osteoarthritis is common in the spine, hips, and knees. Symptoms often include worse stiffness in the morning or after inactivity, but movement typically helps, and pain subsides after a few minutes. Muscles may be weakened around the arthritic joints, especially the knees. Advanced arthritis may cause joint deformation, limited range of motion, and cracking and creaking of the joints.
Diagnosing osteoarthritis is more straightforward. Doctors will inquire about the symptoms being burning, aching, or sharp. They will want to know how long the symptoms in the morning last before they subside and if there is swelling in the affected joints. Doctors will look for joint tenderness, swelling, and any weakening of muscles. Other standard diagnostic tools include X-rays to look for joint damage and blood tests to check for other conditions causing joint pain.
Recommended Reading: Why Do I Have Arthritis In My Knee
The Broader Issue Of Chronic Pain
Dr. Smith emphasizes that in addition to specific conditions such as RA and OA, it is important to be aware of all sources of chronic pain. Chronic, unrelenting pain is the biggest source of disability and financial drain on the western world. We need to rethink how we see pain. The big picture is, Americans hurt. The numbers are massive.
A report from the Institute of Medicine estimates that each year in the United States approximately 100 million adults experience chronic pain, with annual costs between $560 billion and $635 billion. The report notes the need to overcome misperceptions and biases about pain and to use available tools and services to tackle the many factors that influence pain. Research into the causes and the management of chronic pain is increasing, which is good news for patients but people who are affected by chronic pain will still need to take the initiative when it comes to reporting and seeking care for this problem.
Were finding very different outcomes with chronic pain versus something like spraining your ankle, says Dr. Smith. leads to depression it leads to inactivity it makes other health conditions worse. Talk to your doctor if you have a long-term pain issue, but make sure your doctor knows that its a long-term issue.
Early Treatment Improves Outcomes
Although there is no cure for RA, early and aggressive treatment has improved outcomes for many people. Treatment of RA often begins with methotrexate or another disease-modifying anti-rheumatic drug . If this initial treatment does not adequately control the RA, people may move on to treatment with a newer, biologic DMARD.
Effective drugs have dramatically improved RA outcomes, but, according to James K. Smith, MD, a rheumatologist at Northwest Rheumatologists in Portland, Oregon, public awareness of newer types of drugs remains low: Im shocked by the number of people who dont know anything about . Although these drugs allow many people to achieve a remission , Dr. Smith notes that prompt diagnosis and early treatment are tremendously important to treatment success. Explaining some of the barriers to early diagnosis, he says, No insurance, a high deductible, a belief that doctors cant help youthere are lots of reasons why people dont go to the doctor. That delays the diagnosis.
In addition to effective drug therapies, engaging in regular, moderate exercise can help maintain joint flexibility and muscle strength and also improve overall health. People with RA who are considering an exercise program should work closely with their healthcare team to identify a regimen that meets their individual needs.
Recommended Reading: What Foods Are Not Good For Arthritis
Treatment Of Ra Vs Oa
The goal of treatment for both RA and OA is to reduce pain, manage symptoms and halt further joint damage. Non-steroidal anti-inflammatory drugs are prescribed to help with pain and to reduce swelling.
OA treatment
The common joint that is affected by osteoarthritis is the knee and osteoarthritis hip joint. If the destruction of the joint surface becomes irreversible the TKR is the only option left. Physical therapy helps to stabilize and strengthen joints. Heat, rest, weight reduction, and massage also help with pain management.
RA treatment
People with RA need stronger oral steroid medications, such as prednisone, to manage inflammation. They also use medications that prevent joint destruction and halt disease progression, including biologics and disease-modifying anti-rheumatic drugs, or DMARDs .
Regular physiotherapy to prevent joint stiffness and fusion together with Biologics and DMARDs are known for their effectiveness, as well as their increased risk for side effects and infections.
What Other Treatments Can Help Pain Caused By Osteoarthritis And Rheumatoid Arthritis
Q) Im getting desperate. I suffer from both osteoarthritis and rheumatoid arthritis. My greatest problem is osteoarthritis in my cervical spine. For about five years Ive been in constant pain, night and day. My rheumatologist can only suggest exercises, heat, a collar and painkillers , all to little effect. I heard of someone who has Botox injections three times a month, which brings great relief. Could you advise me on this or any other treatment you think would be successful? Im reaching the end of my tether.
Patricia, Altrincham, Cheshire 2011
A) Im sorry to hear about this. Constant pain in the neck is one of the worst types of pain and I know from personal experience how disabling it can be. Ive given Botox injections for neck conditions, but only if significant muscle spasm is present this is sometimes referred to as spasmodic torticollis. Botox works by paralysing the muscles. Its a drug derived from the bacteria that cause botulism, where widespread muscle paralysis can occur. It sounds worse than it is and these injections have now been introduced widely in medicine. Youve probably heard of their use in plastic surgery. The paralysis isnt permanent, but can last for a good while. Often the injections have to be repeated to maintain their benefit. In your case, it would be advisable to seek an opinion from someone who administers these treatments. Other injections, such as selective nerve blocks, are also a possibility.
Don’t Miss: What Can Arthritis Lead To
Understand The Underlying Cause Of Joint Pain
Getting relief may feel like the only thing that matters, but in the long run, the root cause of the pain is very important to determine. The treatments for the two diseases are different, says Paula Rackoff, MD, rheumatologist and clinical associate professor in the department of medicine at NYU Langone Medical Center in New York City. You dont want to miss the opportunity for reversing the inflammatory component of RA. And you dont want to treat OA with potentially toxic medication if you dont need it. But every RA patient eventually gets OA as well, so the pain needs to be diagnosed correctly and reassessed every time.