Epidemiology Of Op In Ra
As previously discussed, RA patients have lower BMD levels at lumbar spine and femoral sites than healthy subjects and this difference can be detected also in an early phase of the disease.
The prevalence of osteoporosis and osteopenia is estimated to be doubled in RA patients as compared to healthy controls with a prevalence ranging from 30 to 50% . The risk of developing OP in RA is correlated with the duration and the severity of the disease and even RA pre-menopausal women or men are exposed to a greater risk of osteoporosis in comparison with age- and sex-matched healthy controls . A prospective longitudinal study on 379 patients identified some biomarkers predictive of BMD change in patients with RA . It was found that the annual BMD change at the lumbar spine had a significant association with glucocorticoids use, bisphosphonate or vitamin D use, and homocysteine. On the other hand, BMD changes at the femur were associated with DAS28, C-reactive protein , and ACPA titer . These results further highlight that there is a strict association between cortical bone health and disease activity while trabecular bone is more affected by classical risk factors .
Albeit OP is a major problem in the management of RA patients, the percentage of patients receiving calcium and vitamin D supplementation is about 45% and only 5.4% are treated with bisphosphonates .
Symptoms Of Osteoporosis Of The Spine
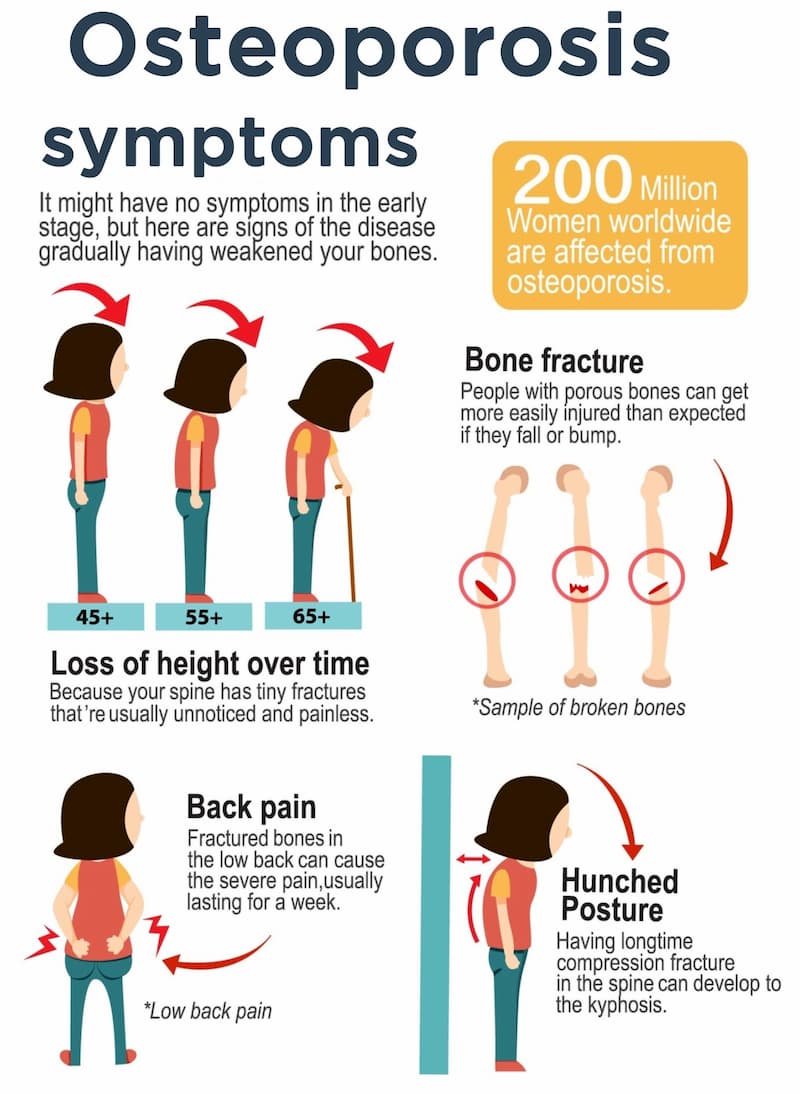
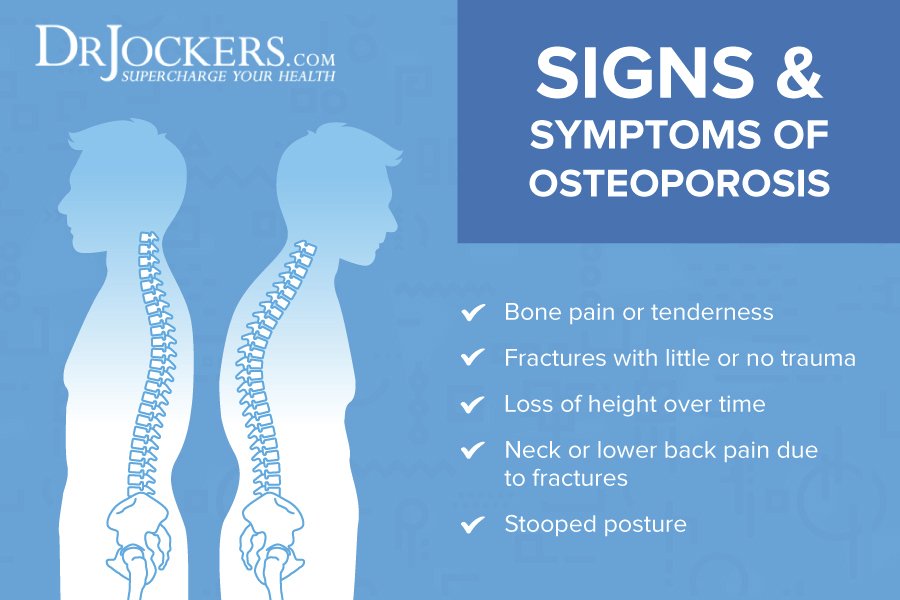
Osteoporosis is often referred to as a silent disease. This means it can develop without any signs. In the case of osteoporosis, bone loss occurs without symptoms. That said, subtle signs of osteoporosis may be joint and bone pain or a loss of height.
Most patients dont know that they have osteoporosis until their bones become so weak that a sudden strain, bump, or fall causes a fracture. Most commonly, osteoporotic fractures occur at the spine, the wrist or the hip, although osteoporotic fractures can occur in other bones as well.
Vertebral Compression Fracture
The vertebrae are the blocks in your back that are stacked on top of each other to make your spine. With osteoporosis the blocks become hollow boxes. Compression fractures occur when the vertebrae collapse. The most common complication of osteoporosis is vertebral compression fracture . These can occur while going about ones daily activities, such as bending or carrying heavy loads, or as the result of a minor fall. Spinal compression fractures may lead to difficulty walking or loss of balance, leading to an increased risk of falling and breaking a hip, or other bones.
The compression fracture may range from mild to severe. A mild compression fracture causes minimal pain and deformity and is often treated with activity modification. At Huffman Clinic, we often treat painful compression fractures with kyphoplasty.
Symptoms
Articles On Knee Osteoarthritis
While age is a major risk factor for osteoarthritis of the knee, young people can get it, too. For some individuals, it may be hereditary. For others, osteoarthritis of the knee can result from injury or infection or even from being overweight. Here are answers to your questions about knee osteoarthritis, including how it’s treated and what you can do at home to ease the pain.
You May Like: Can You Get Arthritis In Your Back
If You Have Both Diseases
Individuals who suffer from osteoarthritis and osteoporosis should seek help planning a program to manage both conditions and pay special attention to advice about exercise.
Regular weight-bearing exercise is usually recommended for individuals with osteoporosis, but may be difficult to follow in the presence of significant hip or knee arthritis. Keeping joints mobile requires a special approach to exercise and movement. A specially trained physiotherapist can help ensure exercises are safe and beneficial for both conditions.
Talk With Others Who Understand
Dealing with osteoporosis associated with PsA may feel overwhelming at times. However, you are not alone. MyPsoriasisTeam is the social network for people with psoriasis and psoriatic arthritis. Here, more than 99,000 members come together to ask questions, offer support and advice, and meet others who understand life with psoriatic disease.
Do you have osteoporosis with your PsA? Share your experience and tips in the comments below or by posting on MyPsoriasisTeam.
Recommended Reading: How Painful Is Ra
Osteoporosis And Psoriatic Arthritis: Is There A Connection
Psoriatic arthritis is a type of inflammatory arthritis that occurs in about 10 percent to 20 percent of people with psoriasis. PsA may affect more than your skin and joints, and several comorbidities are linked with PsA. Among these comorbidities is osteoporosis, a bone disease that causes the bones to become fragile and break easily.
There are typically no symptoms in the early stages of osteoporosis, which may also be referred to as osteopenia. The first sign or symptom of osteoporosis is typically a bone fracture, a curving spine, or the loss of height.
Compared to the general population, people with PsA have a greater risk of developing osteoporosis. The prevalence of osteoporosis may be as high as 46 percent in people with PsA, and rates in the general population are approximately 10 percent to 20 percent.
This article covers the relationship between PsA and osteoporosis, as well as ways to manage and treat these conditions.
How Ra Inflammation Affects Osteoporosis Risk
The inflammation that is central to RA is thought to be a risk factor for osteoporosis in itself. A lot of data shows that active inflammation in the bone, and systemic inflammation, lead to an increased risk of osteoporosis and osteoporotic fractures, says Seoyoung Kim, MD, a rheumatology clinician and researcher at Harvards Brigham and Womens Hospital in Boston.
Studies show that bone loss is greatest in the areas immediately surrounding the affected joints, but that systemic bone loss is also increased.
Recommended Reading: Ra In Hand Symptoms
Epidemiology Of Op In Psa And The Other Spondyloarthritides
Several observational studies have investigated the association between psoriasis or psoriatic arthritis and low BMD values or osteoporosis, with conflicting results.
A cross-sectional study performed on a large population sample with PsO or PsA found that these conditions were significantly associated with osteopenia, osteoporosis, and fragility fractures . Moreover, a 2013 population-based analysis showed a significant association between osteoporosis and previous diagnosis of psoriasis in both sexes .
On the contrary, a Norwegian study based on hospital-derived fractures data found no association between psoriasis and forearm/hip fracture risk or between psoriasis and osteoporosis . Moreover, no differences were found in lumbar spine BMD between Spanish patients with or without PsA and similar findings were underlined during another study conducted in Norway .
However, it’s to be noted that all these data refer to quantitative ultrasound estimated BMD at heel site, which has high specificity but whose sensitivity to predict BMD as defined by dual-energy x-ray absorptiometry can be significantly variable depending on QUS parameters.
Beyond PsA, data on the other Spondyloarthritides with axial involvement , such as Ankylosing Spondylitis , are heterogeneous . Moreover, in patients with axSpA the proper evaluation of vertebral deformities and BMD levels is frequently altered by the presence of syndesmophytes and periosteal bone proliferation .
Signs And Symptoms Of Later
Once bone mass has deteriorated further, you may start to experience more obvious symptoms, such as:
- Loss of height.Compression fractures in the spine can cause you to become shorter. This is one of the most noticeable symptoms of osteoporosis.
- Fracture from a fall. A fracture is one of the most common signs of fragile bones. Fractures can occur with a fall or from minor movement such as stepping off a curb. Some osteoporosis fractures can even be triggered by a strong sneeze or cough.
- Back or neck pain. Osteoporosis can cause compression fractures of the spine. These fractures can be very painful because the collapsed vertebrae may pinch the nerves that radiate out from the spinal cord. The pain symptoms can range from minor tenderness to debilitating pain.
- Stooped posture or fracture. The compression of the vertebrae may also cause a slight curving of the upper back. A stooped back is known as kyphosis, which can cause back and neck pain. It can even affect breathing due to the extra pressure on the airway and limited expansion of your lungs.
Both men and women can develop osteoporosis, but this condition is more common in women because its often caused by hormonal shifts that occur with aging.
Common risk factors for osteoporosis include:
- older age
Read Also: Home Remedy For Arthritis Pain In Hands
What Supportive Devices Are Available To Help With Osteoarthritis
Supportive or assistive devices can help to decrease pressure on the joints with osteoarthritis. Knee supports may be helpful for some people to stabilize the ligaments and tendons and decrease pain. Canes or crutches may be helpful to take pressure off certain joints.
In addition to pain relief, assistive devices improve function and prevent falls. A licensed physical therapist or other health care professional is needed to recommend what devices are best for you.
There are also many available devices to help you perform routine daily activities that may be difficult, such as housework or cooking. Ask your doctor about talking to an occupational therapist to give you ideas about which devices may help.
Signs And Symptoms Of Early
Early, detectable signs of bone loss are rare. Often people dont know they have weak bones until theyve broken their hip, wrist, or some other bone.
However, some signs and symptoms can point toward potential bone loss, such as:
- Receding gums. Your gums can recede if your jaw is losing bone. Ask your dentist to screen for bone loss in the jaw.
- Weaker grip strength. In a study of postmenopausal women and overall bone mineral density, researchers found that low handgrip strength was linked to low bone mineral density. In addition, lower grip strength can increase your risk for falls.
- Weak and brittle fingernails. Nail strength can signal bone health. But you should also take other factors into consideration that may affect your nails, such as exposure to very hot or cold temperatures, regular use of nail polish remover or acrylic nails, or submersion in water for long periods of time.
Other than changes in bone density, osteoporosis doesnt usually cause a lot of initial symptoms. Your best bet for detecting it in the early stages is to talk with your doctor or healthcare professional, especially if you have a family history of osteoporosis.
You May Like: Rash With Rheumatoid Arthritis
Ayushaktis Ayurvedic Treatment Is The Best Option To Reverse Osteoporosis Naturally Ayushaktis Arthrox Treatment Focuses On Increasing The Metabolism Nourishing The Bones Constantly And Balancing The Excess Air In The Body
What is Arthrox treatment?
Arthrox treatment is a combination of customized diet and lifestyle suggestions, herbal supplements, kitchen remedies, and detox therapies. Arthrox ensures more in-depth and long-lasting health for bones and joints.
A healthy diet to improve bone density naturally.
For Osteoporosis and Osteoarthritis, a natural calcium-rich diet is crucial to keep up the bone density optimum. It can also help prevent further degeneration.
What Medications Are Used To Treat Osteoarthritis
The first step with medication is often over-the-counter pain relievers as needed. These include acetaminophen , ibuprofen , and naproxen . Don’t take over-the-counter medications for more than 10 days without checking with your doctor. Taking them longer than that increases the chance of side effects. If over-the-counter treatments aren’t effective, your doctor may decide to prescribe a stronger anti-inflammatory drug or other medication to help ease the pain. Some medications in the form of creams, rubs, or sprays may be applied over the skin of affected areas to relieve pain. For some people with persistent pain despite these pills or creams, steroids can be injected directly into the joint. These injections can be given several times a year, though some experts believe this may ultimately accelerate joint damage.
Injections of hyaluronic acid directly into the knee joint can relieve pain in some people with osteoarthritis.
When osteoarthritis pain is severe and other treatments are not working, some doctors will give stronger pain pills, such as narcotics.
Unfortunately, none of these will reverse or slow the progression of joint damage caused by osteoarthritis.
Read Also: Rheumatoid Arthritis Pain At Night
How Is Osteoarthritis Of The Knee Diagnosed
The diagnosis of knee osteoarthritis will begin with a physical exam by your doctor. Your doctor will also take your medical history and note any symptoms. Make sure to note what makes the pain worse or better to help your doctor determine if osteoarthritis, or something else, may be causing your pain. Also find out if anyone else in your family has arthritis. Your doctor may order additional testing, including:
- X-rays, which can show bone and cartilage damage as well as the presence of bone spurs
- magnetic resonance imaging scans
MRI scans may be ordered when X-rays do not give a clear reason for joint pain or when the X-rays suggest that other types of joint tissue could be damaged. Doctors may use blood tests to rule out other conditions that could be causing the pain, such as rheumatoid arthritis, a different type of arthritis caused by a disorder in the immune system.
Ways To Prevent The Condition
You cannot prevent all forms of osteoporosisâespecially those that are caused by underlying diseases or the aging process. However, you can try to slow the process.
Your age, your sex, and your genetics are not factors that you can control, but there are several risk factors that contribute to osteoporosis that you can have an effect on by making lifestyle changes.
You can help prevent bone loss and osteoporosis by:
- Quitting smoking
- Preventing falls
Also Check: High Rheumatoid Factor Causes
What Are The Complications Of Osteoporosis
Osteoporosis can increase the risk for bone fractures, particularly fractures of the wrist, spine, or hip.
According to the International Osteoporosis Foundation, globally 1 in 3 women and 1 in 5 men, over age 50, will experience osteoporosis fractures.
The effects of spinal fractures can cause a person to become shorter because these fractures can shorten the spinal column. In some instances, bone fractures may require surgery.
According to , bone fractures can increase your risk of disability or death. Hip fractures, in particular, are associated with a 15 to 20 percent increase in mortality within a year, especially among men.
Osteoporosis can also cause bone pain that can affect your ability to perform daily activities.
Treatment for osteoporosis includes medications to help build bone mass. These medications often have hormonal influences, stimulating or acting like estrogen in the body to encourage bone growth. Examples of medications used to treat osteoporosis include:
- bisphosphonates
- parathyroid hormone , such as teriparatide
- parathyroid hormone-related protein, such as abaloparatide
- raloxifene
Romosozumab is a newer medication that the Food and Drug Administration approved in April 2019 to treat osteoporosis in women who have gone through menopause and are at a high risk of experiencing fractures.
It has a boxed warning because the medication may increase the risk of heart attacks or strokes. Its not recommended for people with a history of these conditions.
Take Supplements If You Cant Get These Nutrients From Your Diet Or Lifestyle
We check patients vitamin D levels once every year or so, and because were in Boston, a number of our patients are deficient, says Dr. Kim. In those cases, over-the-counter or even prescription strength supplements can help.
For people who take PPI drugs because of NSAID side effects, Dr. Kim recommends taking the drug on an empty stomach before breakfast, and then taking a calcium supplement with food to promote better absorption.
You May Like: Is Peanut Bad For Arthritis
How Ra And Osteoporosis Share Similar Demographic Risk Factors
In the general population, the risk factors for osteoporosis include being female, Caucasian, and postmenopausal. And, of course, rheumatoid arthritis is much more common in women than in men.
But its hard to say who within rheumatology is at highest risk, says Dr. Wysham. She adds, If youre diagnosed with a rheumatic disease at a younger age, you may have more risk of osteoporosis because youre exposed to inflammation and medications like prednisone for longer periods of time, so theres more time to develop the condition.
Medicare Rebates For A Bone Density Test
There is a Medicare rebate for a bone density test if you:
- Have been previously diagnosed with osteoporosis
- Have had one or more fractures due to osteoporosis
- Are 70 years or over in age
- Are taking corticosteroids, or have Cushings syndrome
- Have not had a menstrual period for more than 6 months, under age 45
- Are male and have low testosterone
- Have rheumatoid arthritis, chronic kidney or liver disease, overactive thyroid or parathyroid or coeliac disease.
Read Also: Arthritis At 30 Symptoms
How Is Osteoarthritis Diagnosed
The diagnosis of osteoarthritis is based on a combination of the following factors:
- Your description of symptoms
- Physical exam
- X-rays
Your doctor may use X-rays to help confirm the diagnosis and make sure you don’t have another type of arthritis. X-rays show how much joint damage has occurred. An MRI may be necessary to get a better look at the joint and surrounding tissues if the X-ray results do not clearly point to arthritis or another condition.
Sometimes, blood tests will be performed to determine if you have a different type of arthritis.
If fluid has accumulated in the joints, your doctor may remove some of the fluid for examination under a microscope to rule out other diseases.
Lifestyle Changes And Healthy Habits
Some risk factors for osteoporosis are preventable with lifestyle changes, including:
- Quitting smoking
- Doing daily physical activity and maintaining a healthy weight
- Doing weight-bearing exercises to help strengthen bones and prevent fractures
- Eating a diet rich in calcium and vitamin D for good bone health
- Limiting amounts of sodium, caffeine, and alcohol in your diet
Also Check: How To Slow Arthritis In Hands