Broken Or Brittle Bones
Rheumatoid arthritis is associated with a loss in bone mineral density,17,18 which is the hallmark sign of osteoporosis. In fact, osteoporosis is considered typical in people who have had rheumatoid arthritis for a long time.19
Certain medications can also increase the risk of developing osteoporosis and its precursor, osteopenia. For example, prednisone and other corticosteroids, which may be prescribed to treat newly diagnosed RA and RA flares, are associated with a loss of bone mineral density.20
Osteoporosis causes bones to become porous and weaker. Osteoporotic bones are:
- More prone to breaking
- Less suitable for joint replacement or other orthopedic surgeries
A bone break can have a negative effect on joint mechanics, even after the bone has healed, increasing the risk for osteoarthritis.
Inflammation & Dry Eye
Because of the lack of basal tears, in other words, the level of tears that you need to keep your eyes from drying out you might experience inflammation. Inflammation is probably the least of your worries in this case.
Your eyes might feel itchy, puffy, and theyre red in colour as they dry out with the air. If the inflammation goes insufficiently treated, it could lead to tissue damage on your eyes outer surface.
Treatment & Management For Dry Eye & Rheumatoid Arthritis
Some very basic things that can help are simple habits:
- Dont smoke.
- Avoid sitting next to air conditioners and heaters.
- Use a humidifier in your bedroom at night.
- Take frequent screen breaks.
- Blink often.
- Eat more fish, or ask your doctor about taking fish oil pills. Omega-3 fatty acids in salmon, tuna, and sardines help block inflammation and may make your eyes feel better.
Recommended Reading: How To Decrease Arthritis Inflammation
Your Patients With Ra Pose Multiple Medical Challenges Dont Overlook These Vision
There are 4 ocular conditions that rheumatoid arthritis patients and PCPs need to be aware of, said rheumatologist Nathan Wei, MD, of the Arthritis Treatment Center in Fredrick, Maryland. Dr. Weis list includes:
Take Note
- Among their other medical challenges, patients with RA are susceptible to several eye disorders. Prompt diagnosis is essential
- Ocular dryness, burning, foreign body sensation, and photophobia in a patient with RA may suggest the most common eye complication seen in RA, keratoconjunctivitis sicca
- Scleritis typically presents with marked eye pain and photophobia. In severe cases, the patient may exhibit intense scleral inflammation, edema, and necrosis
Sjogrens disease
Episcleritis
Cataracts
Sjogrens disease can be primary or secondary, and RA is the most common cause of secondary Sjogrens. It presents with a form of dry eye called keratoconjunctivitis sicca , along with xerostomia, a positive biopsy of the minor salivary gland, and the presence of autoantibodies upon serologic testing. KCS results from pathology in the lacrimal gland. Its the most common ocular complication of RA.1
Other therapeutic options include topical cyclosporine A and punctal occlusion for severe KCS. The latter is best performed by a specialist.
Primarily a nuisance, episcleritis rarely threatens a patients vision and can be managed with symptom relief. That can include topical lubricants, topical NSAIDS, topical glucocorticoids, and oral NSAIDs.
How Does Arthritis Affect The Eyes

Overview
Joint pain and inflammation are probably the main symptoms you think of when it comes to arthritis. While these are the primary signs of osteoarthritis , other forms of the joint disease can affect other parts of your body, including your eyes.
From infections to vision changes, inflammatory arthritis can pose risks to specific parts of the eye. Keep reading to learn how to keep arthritis under control to protect your eyes.
Also Check: Is Salmon Good For Arthritis
Eye Concern #: Blurred Vision From Peripheral Ulcerative Keratitis
PUK is, fortunately, rarebut its a serious condition involving inflammation in the blood vessels of the eye or an ulceration in the cornea, the clear layer over the front of the eye. Symptoms of PUK are similar to those of uveitis and scleritis , including redness, pain, sensitivity to light but PUK can also lead to blurred vision. Sometimes patients with PUK complain that things look fuzzy because swelling can distort the lens of the eye, says Dr. Feinberg.
Stomach Pain Or Indigestion
RA and medicines used to treat it are linked to mouth and stomach ulcers, stomach bleeding, acid reflux, diarrhea, and constipation. Painful diverticulitis and colitis are also possible if you have RA.
RA drugs like NSAIDs often cause ulcers or an upset stomach.
Belly pain is sometimes a sign of a rare RA complication called rheumatoid vasculitis — when inflammation spreads to your blood vessels. Weight loss and lack of appetite are other symptoms. Vasculitis is serious, so see a doctor right away. Learn more about vasculitis symptoms and types.
You May Like: Can You Get Rid Of Arthritis In Your Neck
Cataracts & Glaucoma: Vision Problems Linked With Rheumatoid Arthritis
Everyone should go to regular appointments with their optometrist, but if you are diagnosed with rheumatoid arthritis, you may need to go more often. Two chronic eye diseases, cataracts, and glaucoma are more likely to develop if you have rheumatoid arthritis. If your optometrist or ophthalmologist can diagnose these diseases early, they can help you maintain your sight with treatment.
- Cataracts: This is a condition in which damaged proteins in the lens of your eye bunch together, creating darker spots, cloudy film, or white clumps of material. As they grow larger, these obstruct your vision. Eventually, your lens must be removed and replaced with an artificial lens.
- Glaucoma: This eye disease is caused by damage to the retina from high fluid pressure in your eye. You will develop spots of lost vision or poor peripheral vision. Over time, these become tunnel vision as your retina degenerates. Glaucoma is treatable with special eye drops that lower your fluid pressure, laser surgeries to relieve fluid pressure, or more permanent shunts that allow for ongoing drainage in your eye.
RA may damage the tissues of your eyes because your cornea and sclera are made from collagen, just like your connective tissues. This is what the autoimmune disease attacks.
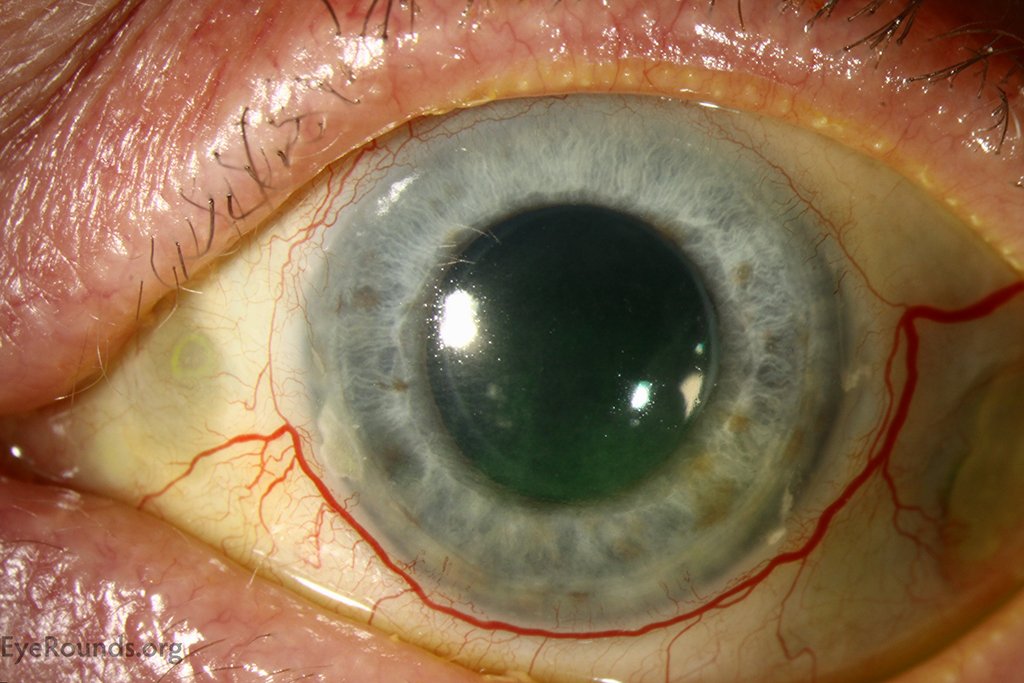
Eye Concern #: A Red Painful Eye From Scleritis
Another type of eye inflammation, scleritis is more concerning than episcleritis because the inflammation is more severe and involves the sclera, the next layer down in the white of the eye. People with RA, as well as other inflammatory or autoimmune diseases, are at increased risk for scleritis. Symptoms include redness and pain, and it can lead to blindness, says Dr. Bhatt. The eye may also have a bluish tinge in the later stage. Patients with scleritis usually make a doc appointment right away because the pain, while not severe or stabbing, is difficult to tolerate.
Don’t Miss: Is Banana Good For Rheumatoid Arthritis
How Do I Know If Rheumatoid Arthritis Is Causing My Dry Eye
Consult with your optometrist or ophthalmologist and receive an eye examination focusing on eye disease diagnosis and management. If you know you have rheumatoid arthritis and begin experiencing dry eye disease, your arthritis is most likely the cause of your condition. This is not always the case though,but it is important to consult with an eye doctor first before seeking treatment options.
Diagnosis Of Eye Problems Tied To Ra
Your doctor will ask questions about your medical history and symptoms. They’ll also take a close look at your eyes. In some cases, they might take a small sample of fluid, pus, or other material from your eye.
You may need a special eye doctor called an ophthalmologist to pinpoint your eye problem. An arthritis doctor called a rheumatologist might help assess your RA. Together, these two doctors can figure out which treatment is best for you.
Recommended Reading: How Can You Treat Rheumatoid Arthritis
What Is Dry Eye
Dry eye stems from the inability to produce quality tears that lubricate the surface of your eye. This can be due to an imbalance in the ratio of meibum , water, and mucin contained in your tears. Dry eyes can also arise from the inability to produce enough volume tears or from tears evaporating too quickly to get their intended result of lubrication.
Eye Concern #: Vision Issues And Floaters From Uveitis

Below the episclera and sclera layers of the eye is another layer called the uvea, and when inflammation occurs here its known as uveitis. There are two types: Anterior uveitis, at the front of the eye, and posterior uveitis, which is at the back of the eye and very rare. Patients with uveitis start having vision problems and seeing floaters around the eye, says Dr. Bhatt. They may also experience redness and pain. Symptoms can have a quick onset and also worsen rapidly.
You May Like: Can You Get Arthritis From Popping Your Fingers
Eye Dryness Irritation Pain Or Blurred Vision
Several conditions that affect the eyes are associated with rheumatoid arthritis. These conditions may be temporary or life-long and can cause a wide range of symptoms.
- Sjögrens syndrome can cause dry eye as well as dry mouth. This condition affects the bodys ability to produce saliva and tears. About 30% of people with RA develop Sjögrens syndrome.1
- Keratoconjunctivitis sicca2,3 affects 15% to 25% of people with RA.4 This condition occurs when the eyes cannot produce enough tears. The lack of moisture may cause eyes to feel dry, irritated, itchy, burning, and/or sensitive to light.
- Episcleritis2 can cause eye irritation, redness, and swelling. Episcleritis may only affect one small part of an eyeball. The affected area may appear raised, red, and/or yellowish. This condition typically goes away on its own, but it can be treated medically.
- Scleritis2,3 can cause deep aching pain in the eye. The eye may water excessively and be sensitive to light. Part or all of the eye may become discolored, appearing red or purple. This is an uncommon but serious condition that can permanently affect vision.
- Keratitis,2,3 or inflammation of the cornea, can cause blurred vision and sensitivity to bright light. It may feel like there is something stuck in the eye.
Report changes in vision to a health care provider immediately.
Treating Rheumatoid Arthritis & Getting Regular Eye Exams Will Keep Your Eyes Healthy
A rheumatologist will diagnose rheumatoid arthritis, but if you think you have this condition and your symptoms include itching or dry eyes, pain, or vision problems, you need to also work with an ophthalmologist. They can prescribe eye drops or other treatments to help you manage eye issues associated with this condition. They can also inform you of potential vision-related side effects from certain rheumatoid arthritis medications.
Treatments include a combination of eye drops, medications, and lifestyle changes.
- Use a humidifier to keep the air in your home from becoming too dry and irritating your eyes.
- Use artificial tears or eye drops to keep your eyes moist.
- Take prescription corticosteroid eye drops if necessary.
- Take your rheumatoid arthritis medication as prescribed to reduce overall inflammation.
You cannot prevent conditions like cataracts or glaucoma from developing, but you can manage these chronic eye diseases with regular checkups and guidance from your ophthalmologist. Eye surgery for these serious conditions may become necessary. Work with your eye doctor and rheumatologist to understand how chronic inflammation and medications to manage this autoimmune disorder may impact your bodys ability to heal.
Don’t Miss: Is Egg Bad For Arthritis
Visiting An Eye Care Specialist
People with RA who experience any change in vision should be evaluated right away. Even if you do not have symptoms of eye problems, regular eye exams may be recommended to monitor for changes in your vision.
There are several different types of eye care professionals. The training and expertise of each type of professional is different, so it is important that you see the right doctor for your needs:7,8
- Ophthalmologist These are doctors who are licensed to practice medicine and surgery. An ophthalmologist can diagnose and treat all eye diseases, perform eye surgery, and prescribe/fit corrective lenses. Many ophthalmologists often conduct research on the causes and cures for eye disease and disorders. Some ophthalmologists also specialize in specific areas of eye care, allowing them to treat more complex or specific conditions of the eye. In many cases, people with RA are referred to an ophthalmologist to manage eye problems.
- Optometrist An optometrist provides primary vision care. This involves performing eye exams, diagnosing certain eye abnormalities, prescribing drugs for eye disease, and prescribing/fitting corrective lenses. An optometrist is not a medical doctor, but has received a doctor of optometry degree from a 4-year optometry school.
Some people with RA may be referred to a neuro-ophthalmologist.
What Is The Role Of The Rheumatologist
Rheumatologist become involved in the care of patients with eye disease when the eye disease is difficult to control. Rheumatologist have experience in the diagnosis of autoimmune and inflammatory diseases. They can further evaluate the patient for systemic conditions that can be associated with eye inflammation. They also have extensive knowledge of the immunosuppressive medications that may be used to treat the disease. They can monitor for potential side effects of the medications being used as well. The role of the rheumatologist is important in the care of patients with eye inflammatory disease so regular follow up is necessary.
Recommended Reading: Can You Work With Rheumatoid Arthritis
Ocular Manifestations Of Autoimmune Disease
SAYJAL J. PATEL, LT, MC, USNR, and DIANE C. LUNDY, CAPT, MC, USN
Naval Medical Center, San Diego, California
Am Fam Physician. 2002 Sep 15 66:991-998.
Patients with autoimmune diseases are frequently encountered by family physicians. It is important to understand not only the systemic effects of these diseases but also their ocular manifestations . Most ocular complications involve the cornea but may also include the conjunctiva, uvea, sclera, retina, and surrounding structures . The majority of these diseases will ultimately need to be referred to an ophthalmologist.
Ocular Manifestations of Autoimmune Disease
Rheumatoid arthritis
Ocular Manifestations of Autoimmune Disease
Rheumatoid arthritis
Cross section of the eye.
FIGURE 1.
Cross section of the eye.
For Many People Joint Pain And Eye Problems Go Hand In Hand Heres Why And How To Protect Your Vision
Inflammatory arthritis is a systemic disease, which means that it affects much more than just your joints. Types of inflammatory arthritis, such as rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis as well as other autoimmune diseases like Sjögrens syndrome and lupus affect organs and systems all over the body.
The eyes are no exception.
The connection between eye health and inflammatory arthritis goes two ways. In some cases, people dont learn that they have a form of inflammatory arthritis until they develop eye symptoms, see an eye doctor, and get referred to a rheumatologist for further evaluation. Some people can present with eye disease early, says Todd Dombrowski, MD, a staff rheumatologist at Dartmouth Hitchcock in Keene, New Hampshire. Early signs of arthritis in the eye can be overlooked or misdiagnosed until additional systemic symptoms crop up. In other cases, people have inflammatory arthritis and then develop eye complications that also require ongoing management from an eye doctor.
Either way, rheumatologists and ophthalmologists or optometrists need to work together to manage the eye manifestations of inflammatory arthritis.
Read Also: What Tests Are Done For Rheumatoid Arthritis
What Is Juvenile Idiopathic Arthritis Of The Eyes
Although it might not seem possible, a disease that affects the joints can sometimes also affect the eyes.
Children with juvenile idiopathic arthritis or JIA can develop eye problems either as a result of the disease itself or, rarely, as a side effect of some medicines.
This information will help you learn more about how JIA might affect your child’s eyes.
How the eye works
- The eye functions in the same way as the inner workings of a camera. The front of the eye admits light rays through the cornea, the pupil , and a transparent fluid known as the aqueous humor in the anterior chamber.
- Next, the lens focuses that light through a clear gel-like substance called the vitreous humor, onto the retina. The retina is a thin layer of tissue that makes up the inner lining of the back of the eye.
- The retina works like film in a camera, transforming light into images. It converts the light rays to impulses that travel along the optic nerve to the brain. The brain integrates the images sent from both eyes and interprets them as a single, three-dimensional image, allowing us to perceive depth and distance.
If any of the parts of the eye become damaged, changes in eyesight can occur.
Shortness Of Breath Or Coughing
The lungs are often affected in people diagnosed with rheumatoid arthritis. Lung conditions may cause coughing, shortness of breath, and chest pain. Rarely, these conditions become life-threatening.
- Interstitial lung disease is an umbrella term used to describe many disorders that cause scarring of the walls of the lungs and certain nearby structures. In people with RA, scarring is typically caused by chronic inflammation. The initial symptoms of interstitial lung disease typically include shortness of breath and a cough.
- Pleural effusion, also called pulmonary effusion or water on the lungs, occurs when fluid collects in the chest cavity outside the lungs. Pleural effusion can cause sharp chest pain, coughing, and shortness of breath. It may be noticeably more difficult to breathe when lying down.
nodules in the lungs typically have no symptoms but may increase the risk for potentially life-threatening conditions, such as a collapsed lung.5,6Rheumatoid nodules in the lungs are rare and account for less than 1% of all rheumatoid nodules.
The chances of developing lung conditions related to RA are increased by smoking.
Don’t Miss: How To Help With Arthritis In Fingers