Ra Imaging Tests: What Tests Are Done For Rheumatoid Arthritis
Rheumatoid arthritis imaging tests are used to look for signs of RA and to monitor the diseases progression. These tests primarily look for bone damage in the patients joints caused by the inflammation associated with RA.
X-rays used to be the most common form of imaging ordered, but they werent always great for reaching an early diagnosis. Todays more modern technology provides advanced imaging techniques like MRIs and ultrasounds, which allow doctors to find early signs of RA more easily.
All types of imaging tests are a critical component of diagnosing RA and monitoring the patients disease as it develops over time. Imaging tests provide doctors with a literal picture of the patients progression so that they can pursue appropriate treatment options.
Quick Answers For Clinicians
The symptoms for rheumatoid arthritis are often nonspecific. Therefore, multiple conditions must be considered in the differential diagnosis of RA. Some of these conditions are , gout, and systemic autoimmune rheumatic diseases such as systemic lupus erythematosus, mixed connective tissue disease, and Sjögren syndrome. Careful evaluation is necessary for proper diagnosis and medical management of these conditions.
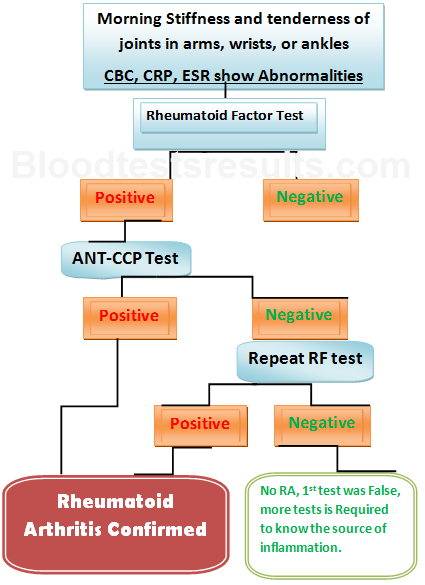
Autoantibodies such as rheumatoid factor , anticitrullinated protein antibodies , and anticarbamylated protein antibodies are a distinctive feature of rheumatoid arthritis . Additionally, their presence often precedes the onset of disease symptoms, making them useful tests for RA diagnosis. Autoantibody testing may also be useful in predicting the severity of disease course. As such, autoantibody testing leads to more accurate diagnosis and prognosis and often contributes to better disease management.
Have You Had The Following Laboratory Tests Performed To Assess The Arthritis
- Rheumatoid Factor . Is it positive or negative?
- Anti-citrullinated protein antibody . Is it positive or negative?
- Are the markers of inflammation, ESR and/or CRP in the blood elevated?
The classification criteria used worldwide to help in classifying an arthritis as RA is the 2010 ACR/EULAR Classification Criteria.
I present this here to help you screen for rheumatoid & to help determine the likelihood of having RA.
Also Check: Is Peanut Bad For Arthritis
What Is A Rheumatoid Factor Test
A rheumatoid factor test measures the amount of rheumatoid factor in your blood. Rheumatoid factors are proteins produced by the immune system. Normally, the immune system attacks disease-causing substances like viruses and bacteria. Rheumatoid factors attack healthy joints, glands, or other normal cells by mistake.
An RF test is most often used to help diagnose rheumatoid arthritis. Rheumatoid arthritis is a type of autoimmune disorder that causes pain, swelling, and stiffness of the joints. Rheumatoid factors may also be a sign of other autoimmune disorders, such as juvenile arthritis, certain infections, and some types of cancer.
Other names: RF Blood Test
The Diagnostic Criteria For Rheumatoid Arthritis
The diagnosis of rheumatoid arthritis cant be established with just one test. Instead, rheumatologists rely on a combination of your medical history, a physical exam, laboratory tests, and sometimes imaging tests to pinpoint the disease.
They also try to rule out the possibility of other conditions that may resemble RA, such as lupus, psoriatic arthritis, gout, or osteoarthritis. This is called a differential diagnosis.
To begin the diagnostic process, a rheumatologist will take your medical history, which includes asking questions about your current symptoms particularly pain, swelling, and stiffness and their location, duration, and severity.
Theyll also ask about your familys medical history as it pertains to RA and other autoimmune conditions. Conditions like RA can be more common in families with RA or other immune system-related health problems. For example, research recently published in the journal Arthritis Care & Research found that people who have a first-degree relative with RA are more than twice as likely as the general population to develop RA. A family history of lupus, scleroderma, thyroid disease, or inflammatory bowel disease also substantially increased the risk of RA.
Your rheumatologist will also perform a physical examination, testing each of your joints for things like swelling, tenderness, and limited range of motion. The location of affected joints is important to diagnosis.
You May Like: What Drugs Are Used To Treat Rheumatoid Arthritis
Getting Tested For Rheumatoid Arthritis
Testing for rheumatoid arthritis is ordered by a doctor or specialist if indicated by a patients symptoms. Blood and urine samples used for testing can be obtained in a doctors office or other medical setting.
Synovial fluid is a liquid that is located in spaces between a persons joints, helping to cushion ends of bones and reduce friction during movement. For a synovial fluid analysis, a sample of synovial fluid is obtained during a procedure called a joint aspiration or arthrocentesis. During a joint aspiration, a doctor uses a needle to withdraw a sample of synovial fluid from a joint.
Ra Blood Tests: What Lab Tests Show Rheumatoid Arthritis
To diagnose rheumatoid arthritis there is no one test that can on its own reach a diagnosis. Instead, there are a number of criteria that must be established in order to reach a rheumatoid arthritis diagnosis.
As part of the criteria for diagnosing rheumatoid arthritis, doctors will order multiple blood tests. These blood tests look for specific indicators that support the possibility that the patient could have rheumatoid arthritis.
Read Also: What Is The Best Cream For Arthritis Pain
Diagnosing Rheumatoid Arthritis With Blood Tests
Rheumatoid arthritis blood tests are only one way to help doctors reach a diagnosis. If a patient is positive for any of these tests, they must also exhibit specific symptoms of rheumatoid arthritis. Doctors look at multiple other criteria besides blood test results when determining their diagnosis.
In some cases, patients can still be diagnosed with rheumatoid arthritis even if they dont test positive for the various types of antibodies found in rheumatoid arthritis blood tests.
Read more about diagnosing rheumatoid arthritis and the different types of rheumatoid arthritis here.
How Your Ra Treatment Plan Prevents Disease Progression
Perhaps the biggest factor that affects how RA progresses is if youre in treatment with a specialist who can put you on medications to slow the disease. Being on a DMARD or biologic therapy for RA is the best way to prevent progression, Dr. Lally says.
Disease-modifying anti-rheumatic drugs are usually the first line in medication. Methotrexate is the anchor drug for rheumatoid arthritis, Dr. Bhatt says. Some patients are scared because methotrexate is also used for cancer chemotherapy so they dont want to take a chemo pill, but those we use for RA are a very small dose with lesser chance of side effects. Your doctor will reassess in a month or so and see if its necessary to add in other drugs.
If after three to six months they have still not responded then we progress to medications called biologics, Dr. Bhatt says. These genetically engineered drugs target the inflammation process specifically, and are usually self-injected or infused via IV in your doctors office or a medical center. There are sub-classes and different types, Dr. Bhatt says. Your doctor will try various medications to see which you respond best to.
Recommended Reading: What Is Good For Rheumatoid Arthritis
Ra Progression Isnt Inevitable
Thanks to the newer treatments available and more on the horizon RA doesnt have to mean a life of eventual disability or even limited mobility. Its not an inevitable thing nowadays, says Dr. Bhatt. People can have a normal life.
But patients do have to be sure to follow their treatment plan and doctors recommendations. Routine follow-up with a rheumatologist who performs joint exams, follows levels of systemic inflammation in the blood and can assess function is the best way to ensure RA is being controlled and is not progressing, Dr. Lally says.
Tests That Help Diagnose Ra
To help confirm or disprove RA, your rheumatologist will also have lab tests done. The lab tests would point to likelihood of rheumatoid arthritis, as well as potentially rule out other possibilities on the differential diagnosis, says Dr. Neogi. These tests may include:
Erythrocyte sedimentation rate and C-reactive protein blood tests detect and measure inflammation in your body. If inflammation levels are elevated, it helps build the case for an RA diagnosis. If inflammation levels are normal, says Dr. Neogi, That might dissuade us from thinking about an inflammatory arthritis like rheumatoid arthritis, but would not rule it out. Since inflammation is present in many diseases, these tests do not confirm whether you have RA by themselves.
Rheumatoid factor and anti-cyclic citrullinated peptide antibody blood tests look for proteins associated with RA. Testing positive for one increases your chances of RA diagnosis, while testing positive for both raises your odds even more. However, up to 50 percent of RA patients dont have RF or anti-CCP antibodies. They are diagnosed based on other factors. In these cases, the RA is considered to be seronegative.
The possibility of some autoimmune disorders, such as lupus and Sjögrens syndrome, can be eliminated with the help of an antinuclear antibody blood test, while a synovial fluid analysis, which examines the fluid that lubricates your joints, can help count out gout by looking for crystals under the microscope.
Don’t Miss: What To Take For Arthritis Pain
People With Seronegative Ra Often Have Different Symptoms
The conventional wisdom is that seropositive patients have more severe symptoms, but recent studies suggest that the difference between the two forms of the disease may have more to do with the joints affected than with the severity of the RA symptoms. And a report published in June 2016 in BMC Musculoskeletal Disorders found that further research is needed to better understand the long-term outcomes of patients with seronegative RA. My experience has been that while the symptoms are similar, seronegative patients are more difficult to treat, says Vinicius Domingues, MD, a rheumatologist in Daytona Beach, Florida, and a medical adviser to CreakyJoints.
Is There Anything Else I Need To Know About An Rf Test

An RF test is not used to diagnose osteoarthritis. Although rheumatoid arthritis and osteoarthritis both affect the joints, they are very different diseases. Rheumatoid arthritis is an autoimmune disease that affects people at any age, but usually occurs between the ages of 40 and 60. It affects more women than men. Symptoms may come and go and vary in severity. Osteoarthritis is not an autoimmune disease. It is caused by the wear and tear of joints over time and usually affects adults over the age of 65.
Read Also: How To Cure Arthritis In Shoulder
The Role Of Rheumatoid Arthritis Testing
Rheumatoid arthritis testing is used to diagnose RA, evaluate the severity of a patients disease, monitor treatment, and detect potential side effects of treatment drugs:
- Diagnosis: Diagnostic testing helps determine the cause of a patients symptoms. If a doctor is concerned that a patients symptoms may be related to rheumatoid arthritis, testing can assist in diagnosing RA and ruling out other health conditions.
- Evaluating severity: The results of several laboratory tests can inform doctors about the severity of a patients RA, the amount of joint damage, and the prognosis or expected course of the disease.
- Treatment monitoring: Monitoring patients diagnosed with RA involves regular medical care, including doctors visits, laboratory testing, and imaging tests. Combining these strategies can assist doctors in tracking the progression of RA and understanding if treatment is effective.
- Detecting side effects: Testing may also be used to detect side effects caused by treatment drugs, as well as other health conditions that are more common in patients with rheumatoid arthritis, including osteoporosis, heart disease, and diabetes.
A Final Word From Creakyjoints
If youre diagnosed with rheumatoid arthritis, youll likely have many questions about next steps and starting treatment. Our downloadable guidelines, A Patients Guide to Living with Rheumatoid Arthritis, provide key info you need to know.
You can also , to start tracking your RA symptoms and have the opportunity to participate in voluntary research studies.
Read Also: How To Deal With Arthritis
Imaging Testing Used In Rheumatoid Arthritis Prognosis
All three imaging tests can be used to monitor progression over the disease course. However, it is difficult for doctors to deliver a firm prognosis for RA as the disease manifests itself uniquely in each patient.
Beyond using x-rays and other RA imaging tests to assess bone erosion levels, doctors cannot conclusively determine if deterioration will worsen or slow down other than what the image tests reveal at the time.
Take This Test: Do You Have Rheumatoid Arthritis
Related Article
The most common cause for a swollen knee in a young woman?
A swollen knee in a young woman needs a reason. Whats the most common cause? Actually, I dont know the answer to that exactly. But when a 30-something year-old presents to her doctor with a swollen knee thats stiff and …
Like this article? Share the love!
Take this test: Do you have Rheumatoid Arthritis?
Lots of people have joint pain or other joint problems. Most of the time, there are not due to rheumatoid arthritis .
There is no single test to diagnose RA. The diagnosis is made from a combination of clinical symptoms and findings, supported by various blood tests .
However, you can try this arthritis screen to determine the likelihood of having the disease by this series of questions which may act as a rheumatoid arthritis test.
Recommended Reading: What Does The Rash From Psoriatic Arthritis Look Like
What Is Rheumatoid Arthritis
Rheumatoid arthritis is a chronic form of arthritis that causes stiffness, pain, and loss of mobility in the joints. Unlike more common forms of arthritis caused by wear and tear on the joints over time, RA is a type of autoimmune disorder.
In RA, the immune system attacks otherwise healthy joint tissue, causing inflammation and degeneration of the joints. Over time, cartilage, bone, and ligaments of a persons joint can wear away and can cause the joint to become bent, twisted, or scarred.
Rheumatoid arthritis usually occurs in a symmetrical way. For example, if one wrist is affected, the other wrist is likely affected as well. Although RA most often affects the wrists and fingers, it can also impact other joints, including the elbows, neck, shoulders, hips, knees, and feet. RA may also cause other health conditions of the blood vessels, heart, lungs, nerves, eyes, and skin.
Although the cause of rheumatoid arthritis is unknown, researchers believe that this condition may develop when a person with an increased risk for RA is exposed to factors in their environment that trigger inflammation. Increasing age, female sex, and genetics increase a persons risk for RA, while environmental triggers that can lead to inflammation and RA include certain bacterial infections, cigarette smoking, and stress.
Seronegative Ra Could Become Seropositive Down The Road
Your rheumatoid arthritis markers may change over time from negative to positive, since many people with seronegative rheumatoid arthritis begin to develop RF or ACPA antibodies. It happens, but its not that common, says Dr. Domingues. Dr. Cush says people with seronegative rheumatoid arthritis may start to develop RF or ACPA within the first two years of diagnosis.
RELATED: Rheumatoid Arthritis Myths Debunked
Don’t Miss: How To Tell What Kind Of Arthritis I Have
Stage : Antibodies Develop And Swelling Worsens
In many cases, RA progresses to the second stage without being diagnosed. In the second stage the body makes the antibodies and the joints start swelling up, Dr. Bhatt says. It can affect other organ systems and cause inflammation there: the lungs, the eyes, a skin rash, and it can even affect the heart. Lumps on the elbows called rheumatoid nodules may also develop.
When it comes to imaging results, the second stage is more confirmative for the diagnosis, Dr. Bhatt says. It has kind of a moth-eaten, chipped off appearance on the X-rays. Ultrasound can also be done, and the most sensitive is an MRI, which would pick up if there are any problems even if the X-ray is normal.
Heres Why The Disease Progresses What To Expect And How To Stop It
Rheumatoid arthritis is a chronic condition for which there is no cure. But even though the disease is progressive, newer disease-modifying drugs may actually be able to slow or even halt it getting worse. We have many effective treatments for RA that help control the symptoms of joint pain and stiffness, but also prevent progression of the disease and the development of permanent damage, says Lindsay Lally, MD, a rheumatologist at Hospital for Special Surgery in New York City.
Early treatment for RA is key, because whatever joint damage has already occurred cant be reversed. Find out how to recognize the symptoms at each stage of RA, and what can be done to treat it.
Don’t Miss: Is Spicy Food Good For Arthritis
Can A Bone Density Test Detect Arthritis
As the name suggests, a bone mineral density test measures the density, or mass, of your bones. This helps to determine overall bone strength while also detecting weaknesses that could potentially lead to fractures.
This type of test is primarily used to diagnose either osteopenia or osteoporosis. Osteopenia is an early loss of bone mass, and is considered a precursor to osteoporosis. Unlike osteoporosis, there arent any symptoms of osteopenia, and its usually found via bone density tests.
Bone density tests may also be used in some types of arthritis, particularly rheumatic versions. Rheumatoid arthritis and psoriatic arthritis can both accelerate bone loss.
Inflammatory arthritis may also increase your risk of developing osteoporosis for the following reasons:
- joint inflammation may trigger bone loss in surrounding areas
- common medications, like glucocorticoids, may speed up bone loss and also decrease calcium and vitamin D metabolism
- reduced activity levels due to pain and overall loss of joint function
But this type of test is not a first-line diagnostic tool for arthritis alone because it focuses on bone mass rather than joint damage.