Elevated White Blood Cell Count: Causes Treatments And More
Jenny Hills, Nutritionist and Medical Writer Health
Doctors test for white blood cell count to measure the number of white blood cells in your body. This blood test is usually done as part of a standard complete blood count test. White blood cells are also called leukocytes and they are part of your immune system. They attack germs, bacteria, and microbes that can cause infections or inflammation. White blood cells can be divided into five main types: neutrophils, lymphocytes, monocytes, eosinophils, and basophils.
Usually, blood test results show elevated white blood cell count if you are fighting an infection or have an inflammatory condition. Pregnancy can also cause a high or slightly elevated white blood cell count. However, other factors like stress, smoking, or allergies can elevate your white blood cell count. Doctors also check for abnormal WBC levels if they suspect an autoimmune condition, blood disorder, or problem with your immune system.
There are not always obvious symptoms if your white blood cell count is outside the normal range. A high white blood cell count could be accompanied by symptoms of a viral infection or allergic reaction like fatigue, runny nose, coughing, or digestive upset. There are also some medical conditions that cause your white blood cell count to drop lower than normal.
Recommended Reading: Arthritis Itchy Skin
Risk Factors For Heart Disease In People With Ra
People with RA share certain risk factors for heart disease with the general population, including:
- High blood pressure
- Physical inactivity
- Side effects from drugs
Dr. Navarro-Millán explained that reducing inflammation from RA is key to reducing the risk of cardiovascular disease. Having rheumatoid arthritis under control, where there is almost no swelling in your joints, no stiffness in your joints, is important in order to decrease this risk, she said.
What Is The Prognosis Of Rheumatoid Arthritis
As a rule, the severity of rheumatoid arthritis waxes and wanes. Periods of active inflammation and tissue damage marked by worsening of symptoms are interspersed with periods of little or no activity, in which symptoms get better or go away altogether . The duration of these cycles varies widely among individuals.
Outcomes are also highly variable. Some people have a relatively mild condition, with little disability or loss of function. Others at the opposite end of the spectrum experience severe disability due to pain and loss of function. Disease that remains persistently active for more than a year is likely to lead to joint deformities and disability. Approximately 40% of people have some degree of disability 10 years after their diagnosis. For most, rheumatoid arthritis is a chronic progressive illness, but about 5%-10% of people experience remission without treatment. This is uncommon, however, after the first three to six months.
Rheumatoid arthritis is not fatal, but complications of the disease shorten life span by a few years in some individuals. Although generally rheumatoid arthritis cannot be cured, the disease gradually becomes less aggressive and symptoms may even improve. However, any damage to joints and ligaments and any deformities that have occurred are permanent. Rheumatoid arthritis can affect parts of the body other than the joints.
Read Also: Does Arthritis Hurt All The Time
Also Check: Does Sugar Cause Arthritis Flare Up
The Cardiac Risks Of Rheumatoid Arthritis
As if the chronic pain and mobility challenges of rheumatoid arthritis werent burdensome enough, its becoming clearer that people with the disease face another serious health threata greater risk for heart disease.
Some 1.5 million Americans, a majority of them women, have this form of arthritis, an autoimmune disease that happens when the immune system attacks the bodys own tissues, causing pain, swelling, stiffness and loss of function in the joints.
Doctors have long known that people with rheumatoid arthritis and related conditions had a shorter lifespan than those without these conditions. Data suggest that heart disease may explain this discrepancy. In fact a review of studies in the journal Nature Reviews Rheumatology suggests that more than 50 percent of premature deaths in patients with rheumatoid arthritis result from cardiovascular conditions.
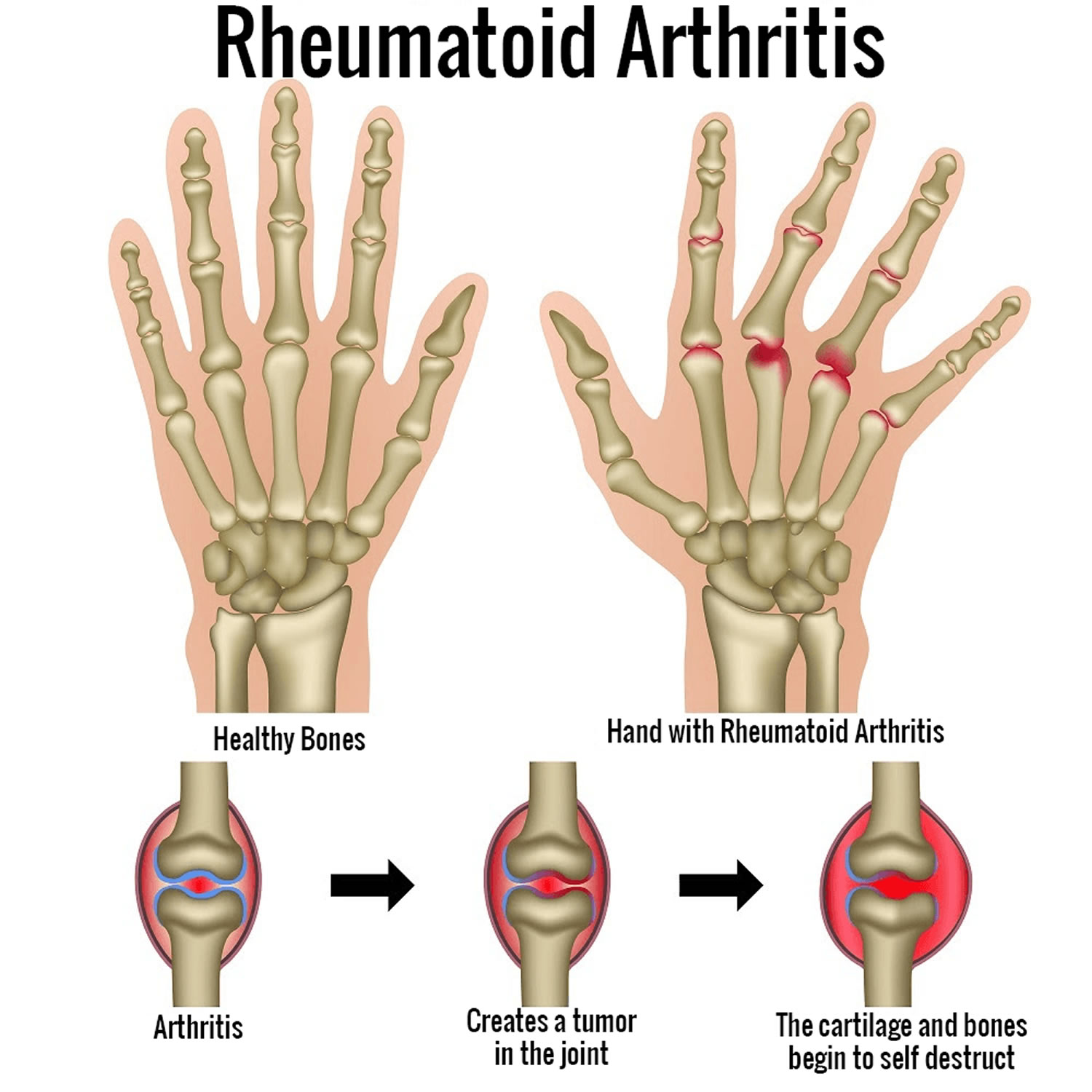
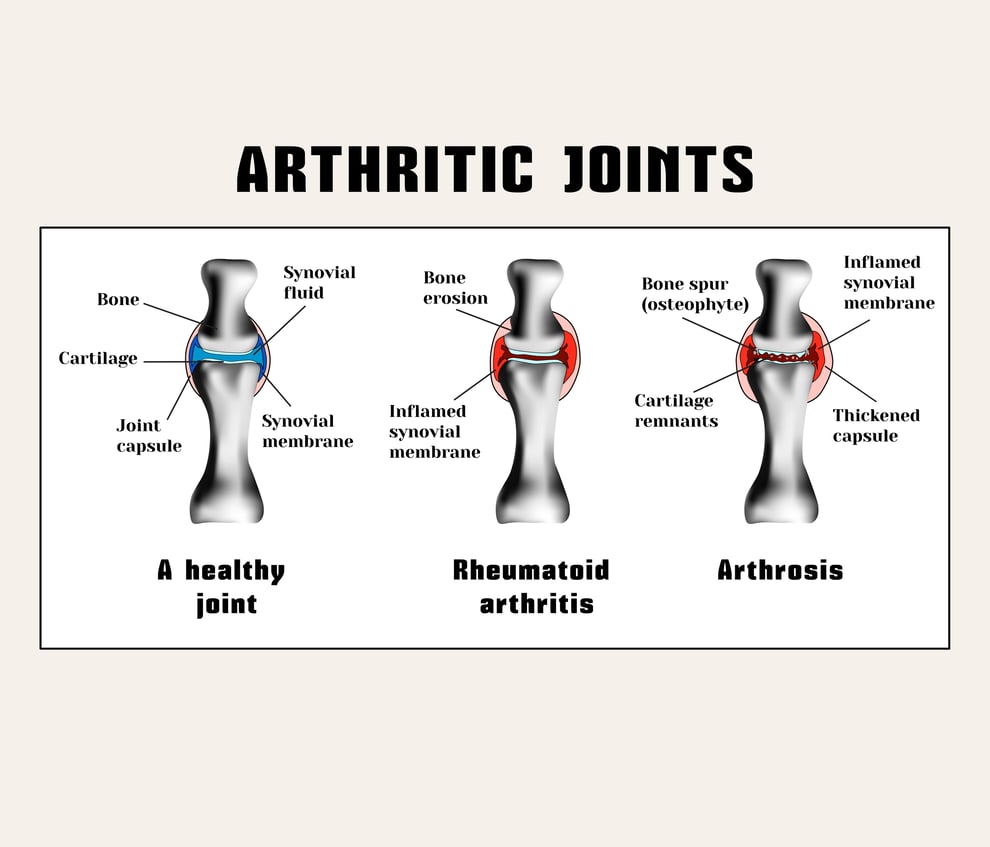
The link between the two diseases: inflammation. In people with rheumatoid arthritis, the immune system attacks the synoviumthe lining of the membranes around the joints. This causes the synovium to thicken, eventually damaging the cartilage and bone.
But the process doesnt stop at the joints. The inflammation can damage systems throughout the body, including the skin, eyes, lungs, and heart. Inflammation narrows the arteries, raising blood pressure and reducing blood flow to the heart, for instance.
Regulator Of The Costimulatory Signal Of T Cell Activation
Abatacept has a short-term effect on endothelial function. The short-term improvement of microvascular endothelial function on abatacept administration coincides with the gradual deterioration of vascular endothelial function , a phenomenon that can induce a shift in the polarization of adipose tissue macrophages from the pro-inflammatory M1 phenotype to the anti-inflammatory M2 phenotype , increase the proliferation and inhibitory activity of Treg cells , improve insulin resistance, increase insulin sensitivity index, and reduce the risk of CVD . Compared with TNF inhibitors, the risk of using abatacept combined with CVD in patients with basic diseases is reduced by 20%, which indicates that abatacept has higher CVD safety than TNF inhibitors, especially for patients with RA who are older and have CVD .
Don’t Miss: What Foods Ease Arthritis Pain
How Does Cardiovascular Disease Relate To Ra
Cardiovascular disease, also known as heart and blood vessel disease, or just âheart disease,â happens when your blood vessels narrow because of plaque buildup. This can lead to a number of problems like heart attack, stroke, heart failure, and heart rhythm problems.
If you have RA you have almost double the chance of developing cardiovascular disease compared with people without RA. There are two main reasons for this.
First, the tiny proteins called cytokines that inflame your joints in RA can also fuel blood vessel damage and plaque buildup in heart disease.
Second, RA and heart disease share many of the same risk factors. Risk factors are simply conditions or activities that raise your chances of getting a certain condition. These shared risk factors include high blood pressure, obesity, smoking, metabolic syndrome and â most importantly for our purposes here â unhealthy cholesterol levels.
In fact, heart disease is the primary risk associated with unhealthy cholesterol levels â sometimes called âhigh cholesterol.â
American Heart Association News Stories
American Heart Association News covers heart disease, stroke and related health issues. Not all views expressed in American Heart Association News stories reflect the official position of the American Heart Association. Statements, conclusions, accuracy and reliability of studies published in American Heart Association scientific journals or presented at American Heart Association scientific meetings are solely those of the study authors and do not necessarily reflect the American Heart Associationâs official guidance, policies or positions.
Copyright is owned or held by the American Heart Association, Inc., and all rights are reserved. Permission is granted, at no cost and without need for further request, for individuals, media outlets, and non-commercial education and awareness efforts to link to, quote, excerpt or reprint from these stories in any medium as long as no text is altered and proper attribution is made to American Heart Association News.
Other uses, including educational products or services sold for profit, must comply with the American Heart Associationâs Copyright Permission Guidelines. See full terms of use. These stories may not be used to promote or endorse a commercial product or service.
Don’t Miss: Does Glucosamine Help Arthritis Pain
Effect Of Heart Disease Therapies In Patients With Ra
There have been relatively few patients with rheumatic diseases enrolled in major clinical trials of primary or secondary prevention. While commonly used CV therapies are presumed to be effective in patients with RA, there is little direct evidence of their efficacy.
Statins appear to reduce vascular inflammation and, have been tested for efficacy in the treatment of RA. Atorvastatin treatment resulted in a small reduction in RA disease activity compared with placebo, suggesting that statins may reduce inflammation directly . Small studies in patients with RA have also shown improvements in arterial stiffness and endothelial dysfunction with atorvastatin . Statin discontinuation for 3 months in patients with RA resulted in a 2% increased risk of acute MI for each month of discontinuation . Notably, statin therapy has also been found to impair the effectiveness of rituximab , so drug interactions will be important to consider in the clinical management of patients with RA.
What The Research Says
Inflammation can hurt your body in all kinds of ways. When inflammation is chronic , it can contribute to a variety of health problems and complications. Chronic inflammation has been linked to the development of heart conditions such as coronary artery disease and heart failure.
Overall, heart disease is the leading cause of death in people with RA.
If your RA is severe or not well controlled, your risk of heart disease goes up even further.
People with RA primarily experience inflammation in their joints, but this inflammation actually affects their entire body. According to research, high C-reactive protein levels an indicator of inflammation in the bloodstream was linked to a higher risk of heart disease in people with RA.
According to a review of research studying more than 5 million people, people with RA were nearly twice as likely as the general population to develop heart failure.
Heat failure appears to be most common among women with RA. According to the research, which identified participants as either men or women, women with RA were
Its important to note that some of these medications, including over-the-counter NSAIDs, can worsen heart failure in people who already have it. Be sure to check with a doctor before starting any new medications.
The other way people with RA can lower their risk of heart problems is by dealing with other cardiac risk factors.
Examples include:
You May Like: What Are The Symptoms Of Arthritis In Your Back
How To Reduce Cardiovascular Morbidity And Mortality In Ra
Much has to be learned from future studies on cardiovascular diseases, i.e. to determine the prevalence and incidence of cardiomyopathy and valve disease that may be detected more easily with new imaging techniques like echocardiography and cardiovascular MRI, and may explain why congestive heart failure is more important than ischaemic heart disease in the mortality of RA. In the mean time, strategies to reduce cardiovascular disease implied in the general population should be used extensively in RA. Also, more RA oriented strategies will be needed as RA-specific factors are important as well , and, therefore, more knowledge is needed on these factors and among those drugs used in RA. Finally, it has been shown that untreated comorbidity in patients with RA is an important problem and joint efforts of rheumatologists and cardiologists may help to improve the cardiovascular morbidity and mortality in RA .
The authors have declared no conflicts of interest.
What Is Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune form of arthritis. Autoimmune means that your immune system overreacts and attacks otherwise healthy cells by mistake. When this happens, it causes chronic swelling and inflammation that can lead to pain and deformity in the affected areas.
RA normally the joints in the following areas:
Chronic inflammation from RA can affect other areas of the body besides the joints. It can also lead to problems with the heart, lungs, and eyes.
You May Like: How Do I Know If I Have Hip Arthritis
Hdl Cholesterol Doesnt Do Its Job As Well
Bad LDL is the type of cholesterol that raises your risk of heart disease and stroke by forming plaque in your arteries. Good HDL cholesterol is supposed to scoop up LDL and shuttle it to the liver so it can get flushed out of the body.
But research suggests that HDL might not be as beneficial as it is in people without RA.
At UCLA, rheumatologist Christina Charles-Schoeman, MD, and her colleagues were among the first to identify the association between RA and dysfunctional HDL that doesnt do a good job of clearing LDL from your vessels.
In particular, higher RA disease activity was associated with alteration in the protein composition of HDL and impairment of its function, she says.
Her group also found that a protein related to HDL, called PON1, was less active in RA patients, and that this shift was associated with higher levels of inflammation and cardiovascular risk in RA patients as evidenced by the plaque visible on carotid artery ultrasounds.
Heart Issues From Ra Take A Toll
So, if you have RA, your likelihood of heart disease goes up. Unfortunately, heart disease also seems to take a particularly high toll on people with RA.
Not only is heart disease common in patients with RA but outcomes appear to be worse, Dr. Sallam explains. A number of studies have shown that patients with RA have a higher risk of death when suffering a heart attack.
According to a recent review of medical studies, people with RA are 45% to 60% more likely to die of heart disease than people who dont have RA. People with RA also tend to have more heart disease risk factors, such as smoking, lack of exercise, and , research tells us.
Some of the medications used to treat RA also can contribute to heart disease. Dr. Liu points to non-steroidal anti-inflammatory drugs , a class of painkiller, and systemic steroids in particular. NSAIDs include Advil , Aleve , and Celebrex , while Deltasone is a commonly prescribed steroid. These types of drugs raise the risk of both CAD and heart failure, says Dr. Liu. Thats true for anyone who takes them. Though its not clear why, these drugs up your odds of dangerous blood clots. They also elevate blood pressure.
If these must be used, it is generally best to use them at as low of a dose as possible and for short durations, he says.
Also Check: How To Care For Rheumatoid Arthritis
Whats The Lipid Paradox In Rheumatoid Arthritis
The lipid paradox is this: Though people with RA have a higher risk of heart disease, they often have lower total cholesterol and LDL levels than the general population. These numbers should lower your risk of heart disease, not raise it. And yet â hereâs the paradox â in those with RA, as total cholesterol and LDL levels go up, the risk of heart disease goes down.
One theory is that in those with RA, inflammation is the main driver behind increased heart disease risk. Lower the inflammation, and you lower the risk of heart disease. So even though certain RA medications can raise your TC and LDL levels, they lower your heart disease risk by getting rid of some of that inflammation.
For example, one such medication, tumor necrosis factor inhibitor , raised TC and LDL as much as 30% while at the same time lowering risk of heart disease.
It also may be that more complex measures of cholesterol, including something called HDL cholesterol efflux capacity, could be more helpful in predicting heart disease in people with RA.
Much more study is needed to be sure.
How Heart Disease Affects People With Ra
Dr. Navarro-Millán is an advocate for coordinated care, in which people with RA get primary care along with seeing a rheumatologist. She emphasized that primary care doctors and rheumatologists need to stay in close communication when risk factors are identified. As rheumatologists, we are really focused on controlling pain, decreasing inflammation, and decreasing and monitoring side effects of medication, Dr. Navarro-Millán said.
But people with RA need to have regular screenings by primary care providers for cardiovascular disease risk factors like hyperlipidemia high cholesterol and high blood pressure. Many of my patients with rheumatoid arthritis say, Well, I don’t have anything else but rheumatoid arthritis. Why should I see a primary care provider? And that is where things start to fall through the cracks, she noted.
One myRAteam member described her experience discovering heart problems unexpectedly. I am in the hospital with high blood pressure and a high heart rate, she said. I went to see my rheumatologist and she sent me straight to the emergency room. I dont have a history of heart problems or high blood pressure.
Also Check: Is Cymbalta Good For Arthritis Pain
Traditional Cv Risk Factors
RA is associated with both traditional and nontraditional CV risk factors 39, 4753. Therefore, assessments based only on traditional risk factors are insufficient to capture the extent of CV risk in RA. A higher Framingham risk score is independently associated to coronary calcification in RA 54. Age and hypertension correlate with increased CV risk RA, but so do factors associated with inflammation, including neutrophil count and radiographic score13. It also appears that physically inactive RA patients have significantly worse CVD risk profile compared with those who are physically active55. While smoking is associated with RF and anti-CCP Ab production and is now recognized as an independent risk factor for RA development56, 57, it does not appear to predict CV events or cardiac-associated mortality in seropositive patients with inflammatory arthritis58. 13. However, the prevalence and severity of coronary calcification in established RA has been linked in part to tobacco use 26. Indeed, a personal history of ischemic heart disease, smoking, hypertension and diabetes mellitus has been found to contribute to CV death in RA59.
Are There Any Risks To The Test
After a blood test, you may have slight pain or bruising at the spot where the needle was put in, but most symptoms go away quickly.
There is very little risk to your baby or child with a needle stick test. Your child may feel a little pinch when the site is poked, and a small bruise may form at the site. This should go away quickly.
Read Also: Joint Pain Medical Term
Recommended Reading: Does Barometric Pressure Affect Arthritis