Polymyalgia Rheumatica Vs Rheumatoid Arthritis
This autoimmune disease is challenging to diagnose for two reasons. First, its symptoms overlap with many other inflammatory and autoimmune conditions. Second, it can cause a variety of symptoms, and an individual may experience just a few symptoms that are not considered typical to the disease.
How is it similar to RA? Polymyalgia rheumatica joint pain is often symmetrical 1 and most noticeable after getting out of bed in the morning. In one study, researchers found inflammation of joints lininga condition called synovitis, a classic sign of RAin 23% of polymyalgia rheumatica cases.2
People with polymyalgia rheumatica also may feel like they have the flu, have a fever, feel weak, or experience weight loss.
See Rheumatoid Arthritis Treatment
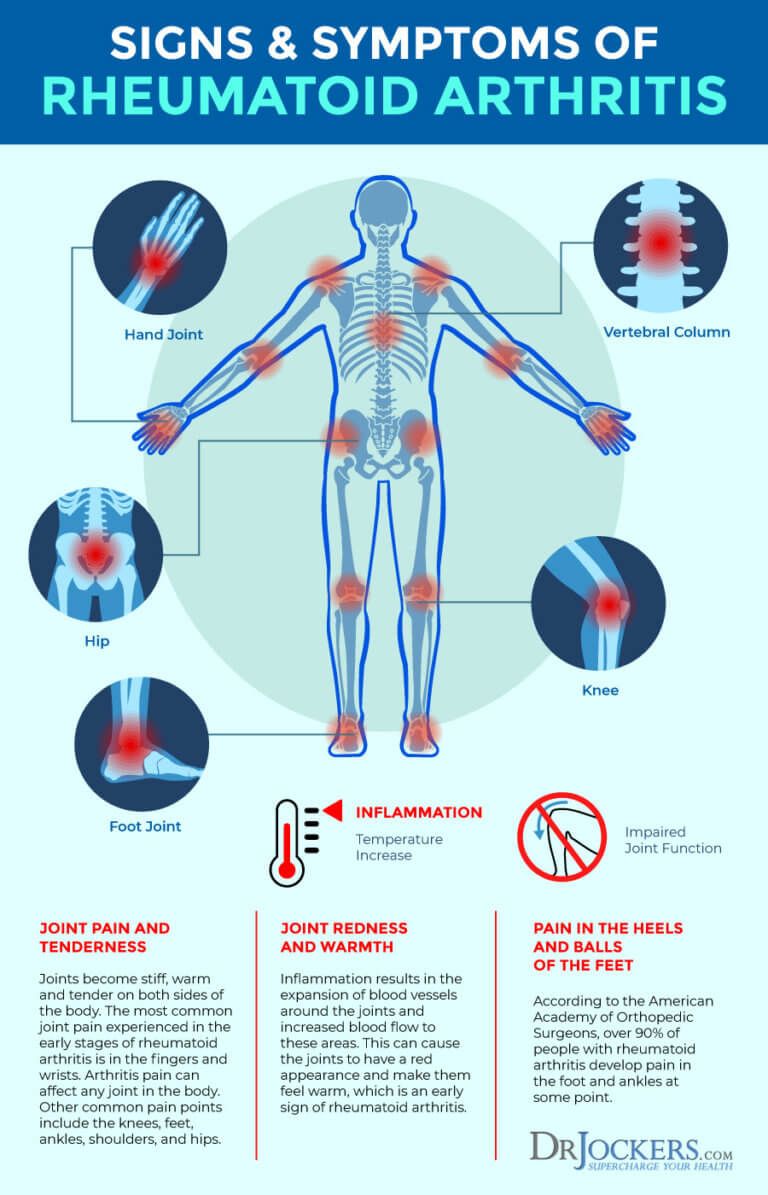
How is it different? Polymyalgia rheumatica usually affects the shoulders, neck, or hips first, whereas RA usually affects hands, feet, or knees first. People with polymyalgia rheumatica typically also experience muscle pain: myalgia means muscle pain, and polymyalgia means muscle pain in multiple locations.
Polymyalgia rheumatica is rarely diagnosed in people under age 50 and it is most commonly diagnosed in people between the ages 70 and 80. 1,4 RA is more commonly diagnosed in people ages 30 to 60.
Maximizing Imaging Procedure Use
The amount of data obtained in a single MR or CT scan is very extensive. Some of the data that radiologists discard could save patients time and money, while reducing their exposure to radiation and risk of complications from invasive procedures. Another approach for making the procedures more efficient is based on utilizing additional constraints, e.g., in some medical imaging modalities one can improve the efficiency of the data acquisition by taking into account the fact the reconstructed density is positive.
For People Autoimmune Conditions Or Taking Immunosuppressants
The clinical trials studying these new vaccines did not include people with significant medical issues, such as autoimmune conditions. This is a common approach for most new drug research since the main goal is to find out how the vaccine would be tolerated by people without these conditions. It does not mean that people with autoimmune conditions should not get vaccinated.
Some people have also wondered whether being on immunosuppressing drugs will impact how well a person responds to the vaccine. There has been concern that if a persons immune system is weakened because of immunosuppressants, they will not be able to produce a strong antibody response to the vaccine. The theory is that these people may not be as protected as someone with a regularly functioning immune system.
At this time, COVID-19 and its vaccines are so new that we do not know what puts a person at higher risk for severe illness or what might impact a persons vaccine response. However, many major organizations, including the American College of Rheumatology, have suggested that the benefits of getting the vaccine and avoiding severe COVID-19 may greatly outweigh the potential risk for those with rheumatic conditions or who are taking immunosuppressants.1,2,5-8 The Center for Disease Control has also stated that people with autoimmune conditions may get the vaccine.9
You May Like: Does Rheumatoid Arthritis Affect Your Toes
What Can I Do To Prevent Osteoarthritis
Maintaining a healthy lifestyle may help prevent osteoarthritis. Eating nutritious foods, maintaining a healthy weight throughout your life, and exercising regularly to strengthen muscles that protect the joints are three very important methods that may reduce your risk of developing osteoarthritis.
Rheumatoid Arthritis Jaw Pain
Jaw involvement is common in people with RA whose disease is not well controlled. Although estimates of its prevalence vary widely between 2 and 88% of people with RA, only a small number of people experience symptoms.Rheumatoid arthritis causes pain and inflammation in the joints. When RA affects the jaw, it often causes tenderness, stiffness, and pain when chewing. In advanced stages, the joint may be painful and make noises when moving.
RA usually affects the joints symmetrically so people may notice the symptoms in both sides of the jaw.
In this article, we examine how RA can affect the jaw, its symptoms, diagnosis, and ways to relieve RA related jaw pain.
Recommended Reading: How To Relieve Arthritis Pain In Thumb
Ra Facts And Statistics
RA is a chronic disease affecting over 1.3 million Americans and as much as 1% of the worldwide population. The specific cause of RA is not known, and as a result there is no known cure for the disease.
Researchers do know, however, that RA is the result of an autoimmune disorder. It is one of the most common autoimmune disorders more common than psoriasis, Crohns disease, multiple sclerosis, and lupus. RA symptoms are triggered when a persons antibodies mistakenly attack the normal synovial joint fluid, causing chronic inflammation.
Women are up to three times more likely to develop RA than men. Women are also more likely to develop the disease at a younger age than men. RA generally begins to affect people between the ages of 30 and 60 years old. The average person doesnt develop symptoms of RA until they reach their 60s.
Lupus Vs Rheumatoid Arthritis
A complex autoimmune disease, lupus can cause a wide range of symptoms that vary in severity, making it challenging to diagnose. Many people refer to lupus by its full medical name, systemic lupus erythematosus .
How is it similar to RA? One of the most common symptoms of lupus is pain and swelling in the hands, knees, and other joints. People often report fatigue, fever, and a general feeling of being unwell.
See Rheumatoid Arthritis Symptoms
How is it different? A person with lupus may find it painful to take a deep breath. He or she may have sensitivity to light, hair loss, mouth sores, and/or a skin rash, particularly over the face. Digestive difficulties and neurological problems, such as headaches and tingling, are also possible.
Recommended Reading: Is Peanut Bad For Arthritis
What Are Newer Rheumatoid Arthritis Medications And Side Effects
Newer “second-line” drugs for the treatment of rheumatoid arthritis include the following:
Each of these medicines can increase the risk for infections, and the development of any infections should be reported to the doctor when taking these newer second-line drugs.
While biologic drugs are often combined with DMARDs in the treatment of RA, they are generally not used with other biologics due to the risk of serious infections. Similarly, JAK inhibitor medication is not used with traditional biologic medicines.
How Does The Autoimmune Response Develop In Ra
In its earliest stages, even before joint inflammation occurs, RA is thought to begin with a series of events in which the immune system loses its ability to distinguish between what belongs to the body and what is foreign to the body . This process, which occurs systemically begins with inadequate clearance of cells as they die. Normally, dying cells do not come in contact with the immune system and are not identified as a potential threat to the body.1
As cells reach the end of their lifespan, they undergo citrullination, a process in which enzymes called peptidylarginine deiminases transform proteins within the cell. This is a normal part of cell physiology.1
However, in most patients who develop RA , citrullinated proteins and PADs leak from dying cells throughout the body. The leaked PADs transform proteins in the extracellular fluid . These citrullinated proteins are recognized as antigens by the immune system. In response to these antigens, the immune system generates anti-citrullinated protein antibodies . The creation of ACPA indicates a loss of tolerance to the self. The presence of ACPA is an accurate predictor of RA, as is rheumatoid factor , and can even predict the disease some 15 years before it becomes clinically apparent with joint symptoms.1
You May Like: Is Glucosamine And Chondroitin Good For Arthritis
How Are Autoimmune Diseases Treated
There are no cures for autoimmune diseases, but symptoms can be managed. Everyones immune system, genetics and environment are different. That means that your treatment must be unique.
Some examples of medications used to treat autoimmune diseases include:
- Painkillers.
- Limiting processed foods from your diet.
Ra Autoimmune Process And Evolution Of Joint Damage
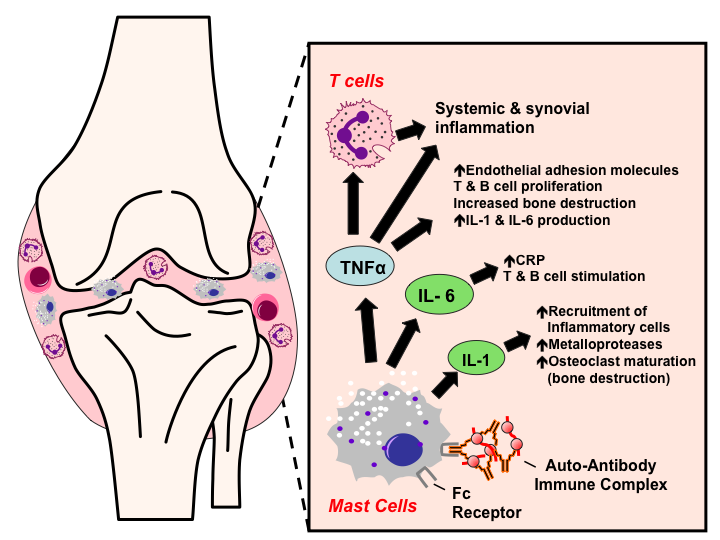
In RA, the immune system malfunctions and attacks healthy joint tissue as if it were a foreign invader. Leukocytes travel to joint cavities, launching an inflammatory response. White blood cells, including B- and T-cells, neutrophils, dendritic cells, and macrophages, and other types of immune cells including mast cells multiply in the joint cavity.2,3
These immune cells release inflammatory mediators, including cytokines, leukotrienes, and prostaglandins. Some of these substances promote the growth of blood vessels, which supply nutrients to the growing mass of leukocytes, resulting in the formation of pannus , a flap of fibrous tissue that forms over the synovial cartilage. The synovial lining on the inside of the joint becomes inflamed and swollen. With continued exposure to inflammation, thickening of the synovial lining and pannus formation, over time the joint space decreases and the bony structure of the joint itself may become deformed and, in extreme cases, the joint may cease to function.2,3
You May Like: Is Papaya Good For Arthritis
About Rheumatoid Arthritis And Lupus
Rheumatoid arthritis and lupus are relatively common, severe disorders. About 1.5 million people or about 0.6 percent of the U.S. adult population have rheumatoid arthritis. Estimating how many people in the U.S. have lupus is difficult because symptoms vary widely and onset is often hard to pinpoint. Both conditions are autoimmune diseases that occur when the immune system mistakenly attacks parts of the body that it is designed to protect. They represent just two of a larger number of autoimmune disorders, including multiple sclerosis, Crohns disease, ulcerative colitis, type 1 diabetes, and psoriasis. These diseases share common flaws in immune function and regulation, leading to inflammation that destroys tissues. They can last a lifetime, cause severe disability, greatly affect quality of life, and are associated with increased risk of death.
Heart And Blood Vessels
People with RA are more prone to atherosclerosis, and risk of myocardial infarction and stroke is markedly increased.Other possible complications that may arise include: pericarditis, endocarditis, left ventricular failure, valvulitis and fibrosis. Many people with RA do not experience the same chest pain that others feel when they have angina or myocardial infarction. To reduce cardiovascular risk, it is crucial to maintain optimal control of the inflammation caused by RA , and to use exercise and medications appropriately to reduce other cardiovascular risk factors such as blood lipids and blood pressure. Doctors who treat people with RA should be sensitive to cardiovascular risk when prescribing anti-inflammatory medications, and may want to consider prescribing routine use of low doses of aspirin if the gastrointestinal effects are tolerable.
Don’t Miss: What To Do For Arthritis In The Thumb
The Difference Between Rheumatoid Arthritis And Osteoarthritis
Like RA, people with osteoarthritis can experience painful and stiff joints that make moving around difficult.
People with OA may have joint swelling after extended activity, but OA doesnt cause any significant inflammatory reaction that typically results in redness of the affected joints.
Unlike RA, OA isnt an autoimmune disease. Its related to the natural wear and tear of the joints as you age, or it can develop as a result of trauma.
OA is most often seen in older adults. However, it can sometimes be seen in younger adults who overuse a particular joint such as tennis players and other athletes or those whove experienced a severe injury.
RA is an autoimmune disease. The joint damage from RA isnt caused by normal wear and tear. Its caused by your body attacking itself.
Rheumatoid Arthritis: Causes Symptoms Treatments And More
Rheumatoid arthritis is an inflammatory type of arthritis that can causes joint pain, swelling and damage. Learn what causes RA and how to treat it.
Rheumatoid arthritis causes joint inflammation and pain. It happens when the immune system doesnt work properly and attacks the lining of the joints . The disease commonly affects the hands, knees or ankles, and usually the same joint on both sides of the body. But sometimes, RA causes problems in other parts of the body as well, such as the eyes, heart and circulatory system and/or lungs. For unknown reasons, more women than men get RA, and it usually develops in middle age. Having a family member with RA increases the odds of developing RA.
Causes
In a healthy person, the immune system fights invaders, such as bacteria and viruses. With an autoimmune disease like RA, the immune system mistakes the bodys cells for foreign invaders and releases inflammatory chemicals that attack, in the case of RA, the synovium. Thats the tissue lining around a joint that produces a fluid to help the joint move smoothly. The inflamed synovium gets thicker and makes the joint area feel painful and tender, look red and swollen and moving the joint may be difficult.
Researchers arent sure why some people develop RA. They think that these individuals have certain genes that are activated by a trigger in the environment, like a virus or bacteria, or physical or emotional stress or some other external factor.
Symptoms
Don’t Miss: How To Beat Rheumatoid Arthritis Naturally
What Are Rheumatoid Arthritis Causes And Risk Factors
The cause of rheumatoid arthritis is unknown. Even though infectious agents such as viruses, bacteria, and fungi have long been suspected, none has been proven as the cause. The cause of rheumatoid arthritis is a very active area of worldwide research. It is believed that the tendency to develop rheumatoid arthritis may be genetically inherited . Certain genes have been identified that increase the risk for rheumatoid arthritis. It is also suspected that certain infections or factors in the environment might trigger the activation of the immune system in susceptible individuals. This misdirected immune system then attacks the body’s own tissues. This leads to inflammation in the joints and sometimes in various organs of the body, such as the lungs or eyes.
It is not known what triggers the onset of rheumatoid arthritis. Regardless of the exact trigger, the result is an immune system that is geared up to promote inflammation in the joints and occasionally other tissues of the body. Immune cells, called lymphocytes, are activated and chemical messengers are expressed in the inflamed areas.
Gut bacteria, smoking, and gum disease
Environmental factors also seem to play some role in causing rheumatoid arthritis. For example, scientists have reported that smoking tobacco, exposure to silica minerals, and chronic periodontal disease all increase the risk of developing rheumatoid arthritis.
Understand that many forms of joint disease mimic rheumatoid arthritis.
Major Players In The Autoimmune Response: Leukocytes
Leukocytes or white blood cells are key immune system cells that play a central role in the autoimmune response that occurs during RA. Leukocytes include a number of different types of white blood cells with different functions. Those with key involvement in the RA autoimmune response include neutrophils, lymphocytes , monocytes, macrophages, and dendritic cells . In addition to leukocytes, another immune system cell called a mast cell plays an important role in the autoimmune process, releasing cytokines, chemokines, and enzymes called proteases.
- Synthesize range of immune system chemicals
Read Also: How To Treat Arthritis In Lumbar Spine
What Questions Might A Healthcare Provider Ask To Help Diagnose An Autoimmune Disease
When your healthcare provider interviews you, they might ask you one or more of the following questions:
- What medications are you taking?
- What are your symptoms?
- How severe are your symptoms?
- Have you had to go to the emergency department because of your symptoms?
- How long have you had these symptoms?
- In what ways are your symptoms affecting your quality of life?
- Is there anything that triggers your symptoms? Anything that makes them worse?
- Is there a history of autoimmune diseases in your family?
- Which autoimmune diseases run in your family?
- What over-the-counter or alternative medicines have you tried, if any?
Ra And The Autoimmune Attack On Joints
In patients with ACPA and/or RF, autoantibody production and inflammation occurs systemically before it occurs in the joints. Therefore, it is thought that some other factor or trigger is involved in causing the early systemic autoimmune response to move to the synovium , leading to the symptoms characteristic of RA.1
This unknown factor causes leukocyte migration and infiltration into the synovium. As the immune system is activated and the disease progresses, a cascade of inflammatory cell types and immune system chemicals are produced. These immune system cells and the wide range of chemicals they produce play a role in the autoimmune process, which ultimately causes joint destruction.1
Don’t Miss: How To Ease Arthritis Pain In Ankle
Genetics Of Rheumatoid Arthritis
The strongest genetic association in RA is observed with the major histocompatibility complex class II, DR1 gene. This highly polymorphic gene encodes a cell surface molecule that is primarily expressed in antigen-presenting cells, such as dendritic cells, macrophages, and B cells. This molecule mediates the presentation of peptide antigens to T cells, which stimulates the cellular response to these antigens. Many variants of HLADR1 are associated with RA, and some variants are also associated with periodontitis. This association is due to five key amino acids on the side wall of the HLADR1 molecule . This sequence is a shared epitope, and predisposition to the disease requires the presence of positively charged arginine and lysine residues at position 71 in the HLADR1 molecule. This positively charged motif sequence presents citrulline residue-containing peptides to T cells.
When To Get Medical Advice

See a GP if you think you have symptoms of rheumatoid arthritis, so they can try to identify the underlying cause.
Diagnosing rheumatoid arthritis quickly is important, because early treatment can prevent it getting worse and reduce the risk of joint damage.
Find out more about diagnosing rheumatoid arthritis.
You May Like: What Does Psoriatic Arthritis Back Pain Feel Like