Psoriatic Arthritis Imaging Test: Mri
If the X-rays dont show inflammation, and the doctor wants more evidence, they may do an MRI, Rubenstein says. Thats because MRIs are more precise than X-rays. This noninvasive imaging technique uses a magnetic field and computer-generated radio waves to create detailed three-dimensional images.
During an MRI, you lie inside a machine and remain very still while the device moves a strong magnetic field, then radio waves, through your body to excite protons found in the water that makes up human tissue, according to the National Institute of Biomedical Imaging and Bioengineering. The procedure is painless and, unlike X-ray imaging, does not emit radiation.
A radiologist analyzes the MRI, then reports back to the rheumatologist. Inflammation, swelling, and bone erosion all indicate that psoriatic arthritis is active, notes Rubenstein.
Frequency of Testing A doctor may order an MRI during initial testing to help with making a psoriatic arthritis diagnosis, as well as later to monitor the disease or look for any changes in a patients psoriatic arthritis symptoms. Tests may be done several times a year, says Cadet.
What Are The Symptoms Of Psoriatic Arthritis
The symptoms of psoriatic arthritis may be gradual and subtle in some patients in others, they may be sudden and dramatic. It may be mild, affecting only one joint or can be severe, affecting multiple joints. Not all patients experience all symptoms.
The most common symptoms of psoriatic arthritis are:
Joint symptoms
- Pain or aching, tenderness, and/or swelling in one or more joints – most commonly hands, feet, wrists, ankles, knees.
- Joint stiffness most notable in the morning or with prolonged inactivity such as sitting for a long time.
- Reduced range of motion in affected joints.
- Pain or stiffness in the lower back.
- Tenderness, pain, or swelling where tendons and ligaments attach to the bone , such as the Achilles tendon of the heel.
- Swelling of an entire finger or toe with a sausage-like appearance .
Skin symptoms
- Silver or gray scaly spots on the scalp, elbows, knees, and/or the lower spine.
- Small, round spots called papules that are raised and sometimes scaly on the arms, legs and torso.
- Pitting of the nails.
- Detachment or lifting of fingernails or toenails.
Other symptoms
Talk With Others Who Understand
On MyPsoriasisTeam, the social network for people with psoriasis and psoriatic arthritis, more than 108,000 members come together to ask questions, give advice, and share their stories with others who understand life with psoriatic arthritis.
Have you been diagnosed with psoriatic arthritis? How was your diagnostic process? Share your thoughts in the comments below, or start a conversation by posting on MyPsoriasisTeam.
Don’t Miss: How Does Psoriatic Arthritis Feel
Rheumatoid Factor Blood Test
Rheumatoid factor is a type of protein known as an autoantibody. Because RF targets the bodys own healthy tissues, elevated levels of the substance in the blood often indicate the presence of an autoimmune disease.
As its name suggests, a rheumatoid factor blood test is often used to screen for rheumatoid arthritis . During this test, your doctor will draw a small sample of blood usually from a vein in your arm and send it off for laboratory testing. Lab technicians will assess the levels of rheumatoid factor in your blood.
Positive RF test results indicate that your body is producing more rheumatoid factor antibodies than it normally would. Generally, the normal range for RF is between 0 IU/mL and 15 IU/mL. Mild elevation in the upper teens and 20s isnt usually a cause for concern. However, significantly higher rheumatoid factor results may indicate unusual autoimmune activity.
While doctors frequently order rheumatoid factor blood tests to confirm RA, the test can also indicate other RF-elevating diseases, such as cancer, Sjogrens syndrome, systemic lupus erythematosus , and sarcoidosis. That said, the test isnt perfect. According to the The United Kingdoms National Health Service, about one in 20 people without RA still receive positive RF results. Some may have one of the diseases mentioned above, while others may be healthy and simply have a high rheumatoid factor.
Who Is At Risk For Psoriatic Arthritis
Psoriasis affects 2-3 percent of the population or approximately 7 million people in the U.S. and up to 30% of these people can develop psoriatic arthritis. Psoriatic arthritis occurs most commonly in adults between the ages of 35 and 55 however, it can develop at any age. Psoriatic arthritis affects men and women equally.
It is possible to develop psoriatic arthritis with only a family history of psoriasis and while less common, psoriatic arthritis can occur before psoriasis appears. Children of parents with psoriasis are three times more likely to have psoriasis and are at greater risk for developing psoriatic arthritis. The most typical age of juvenile onset is 9-11 years of age.
Don’t Miss: Does Aleve Work For Arthritis
Comorbidities Of Psoriatic Arthritis
PsA is linked to a number of chronic illnesses that can shorten life and reduce the quality of life. Even though most studies suggest that overall mortality in individuals with psoriatic arthritis is not greater than in the general population, obesity and cardiovascular comorbid conditions are more common, which might affect lifespan and quality of life.
When compared to the general population, the prevalence of cardiovascular risk factors such as hypertension, hyperlipidemia, type 2 diabetes mellitus, and the combination of these is higher in psoriatic arthritis. Even after adjusting for established risk variables, psoriatic arthritis is linked to an elevated risk of cardiovascular events like myocardial infarction. Similarly, people with psoriatic arthritis have a higher chance of developing type 2 diabetes and fatty liver.1
PsA has also been linked to extra-articular symptoms such as uveitis and inflammatory bowel disease, such as Crohns disease and ulcerative colitis. In patients with psoriatic arthritis, a meta-analysis found a 3% prevalence of uveitis and a 3% prevalence of inflammatory bowel disease. Because not all psoriatic arthritis treatments cover various manifestations, these conditions can have a significant impact on treatment choices.1
Blood Fluid And Tissue Tests For Arthritis
Checking blood, tissues and various body fluids help doctors diagnose and monitor arthritis.
Blood and other lab tests play a critical role in diagnosing and monitoring arthritis. When your doctor needs to confirm an arthritis diagnosis, monitor disease progress, check medication effectiveness or determine if medications are causing potentially dangerous but not evident side effects, lab tests are ordered.
Most tests require drawing and testing the blood, but some may involve testing urine, joint fluid or even small pieces of skin or muscle.
Diagnosing and Monitoring Disease Activity
If your doctor suspects you have inflammatory arthritis, these are the most common tests used to diagnose as well as monitor the disease:
Blood Tests
Other Lab Tests
- Skin biopsy A small piece of skin is removed by a doctor. Its usually done under local anesthetic. The sample is tested in a lab and the results help determine the presence of lupus, vasculitis and psoriatic arthritis.
- Muscle biopsy A doctor takes the tissue sample from a muscle with a biopsy needle. The sample is reviewed for signs of damage to muscle fibers to help confirm a diagnosis of polymyositis or vasculitis.
- Joint fluid tests A doctor removes a small amount of fluid from a joint to determine the presence of uric acid and diagnose gout.
Monitoring Medication Response and Side Effects
Checking for Comorbidities
Hello,
Also Check: Does Drinking Water Help Arthritis
Having Psoriasis Isnt Always A Reliable Clue
Around 70 percent of people with psoriatic arthritis develop psoriasis first, but in the other 30 percent of the time, the arthritis and skin symptoms occur around the same time, people have psoriasis but dont realize it, or the psoriasis may develop later on after the arthritis-like symptoms show up. Some people can develop psoriatic arthritis without having psoriasis.
Is Psoriatic Arthritis Genetic
There is no single gene that causes psoriatic arthritis to develop, but experts believe there is probably a genetic component9, as nearly half of those who develop the condition have a family history of either psoriasis or psoriatic arthritis. A family of genes known as the human leukocyte antigen complex may be involved. HLA genes help the immune system know which proteins to attack, and variations in this group of genes may alter your risk of getting psoriatic arthritis10. However, there is still a lot of research to be done. Some people with psoriatic arthritis test positive for the HLA antigen, but a positive test is not a requirement for a psoriatic arthritis diagnosis.
Don’t Miss: Are Bananas Good For Rheumatoid Arthritis
Treatments For The Arthritis
Non-steroidal anti-inflammatory drugs
NSAIDs, or non-steroidal anti-inflammatory drugs, can reduce pain, but they might not be enough to treat symptoms of psoriatic arthritis for everyone.
Some people find that NSAIDs work well at first but become less effective after afew weeks. If this happens, itmight help to try a different NSAID.
There are about 20 different NSAIDs available, including ibuprofen, etoricoxib, etodolac and naproxen.
Like all drugs, NSAIDs can have side effects. Your doctor will reduce the risk ofthese, by prescribing the lowest effective dose for the shortest possible period of time.
NSAIDs can sometimes cause digestive problems, such as stomach upsets, indigestion or damage to the lining of the stomach. You may also be prescribed a drug called a proton pump inhibitor , such as omeprazole or lansoprazole, to help protect the stomach.
For some people, NSAIDs can increase the risk of heart attacks or strokes. Although this increased risk is small, your doctor will be cautious about prescribing NSAIDs ifthere are other factors that may increase your overall risk, for example, smoking, circulation problems, high blood pressure, high cholesterol, or diabetes.
Some people have found that taking NSAIDs made their psoriasis worse. Tell your doctor if this happens to you.
Steroid treatment
Steroid injections into a joint can reduce pain and swelling, but the effects do wear off after a few months.
Disease-modifying anti-rheumatic drugs
Biological therapies
Psoriatic Arthritis Blood Test: C
C-reactive protein is a protein in the blood that indicates inflammation. If a blood test shows high CRP levels, you might have psoriatic arthritis, explains Dr. Husni.
Your doctor may use the test if your ESR is normal, since CRP is more accurate at detecting inflammation in some people, adds Cadet.
Again, different labs may have slightly different interpretations of readings.
Frequency of Testing CRP analysis may be done for diagnosis and then several times a year to assess whether inflammation has responded to treatment, notes Cadet.
Don’t Miss: What Can You Do For Arthritis In The Neck
Delays In Getting Diagnosed With Psoriatic Arthritis Are All Too Common Knowing What To Expect May Help Speed Up The Process
If your shoes are feeling tighter than usual or youre having difficulty or pain opening jars, a type of autoimmune disorder called psoriatic arthritis could be to blame. PsA is an inflammatory arthritis linked to psoriasis . It is characterized by pain, stiffness, and swelling in the joints although these general arthritis symptoms can take on specific characteristics when they are caused by psoriatic arthritis
As with many conditions, early diagnosis and prompt treatment are important. If you put off seeing the doctor, there are two major concerns with a delayed psoriatic arthritis diagnosis, says Bharat Kumar, MD, Associate Rheumatology Fellowship Program Director at University of Iowa Health Care and member of the American College of Rheumatology.
First, he explains, disease activity may worsen and cause lasting joint damage. Second, PsA is linked to a higher rate of heart disease, so the sooner youre diagnosed the quicker you can address cardiovascular factors like high cholesterol and hypertension. Rheumatologists are eager to see anyone with psoriasis who is also experiencing joint pain, Dr. Kumar says.
Psoriatic Arthritis Diagnosis & Presentation
Because there are no particular biomarkers for psoriatic arthritis, the diagnosis is primarily based on the detection of clinical and radiological findings.8 PsA is a clinically heterogeneous disease that affects peripheral joints or the sacroiliac joints, as well as the spine , where inflammatory responses in other tissues, such as enthesitis and dactylitis, are seen in addition to synovitis. Chronic inflammatory spinal pain, bi- or unilateral sacroiliac joint pain, and pain at entheses, defined clinically as enthesitis, peripheral arthritis, dactylitis, and skin and nail psoriasis are all seen in the course of PsA.10
Psoriatic arthritis has a wide range of clinical manifestations. Moll and Wrights first classification of psoriatic arthritis comprised five subtypes:11
- Oligoarticular arthritis shows asymmetric involvement. It affects less than 5 small or large joints
- Polyarticular arthritis shows symmetric involvement with presentation identical to rheumatoid arthritis but it involves the distal interphalangeal joints and rheumatoid factor is negative
- Distal arthritis shows the involvement of the DIP joints predominantly
- Arthritis mutilans shows the severe form of the destructive joint disease with the presence of deformities, particularly in hands and feet
- Spondyloarthritis pattern with the presence of sacroiliitis and spondylitis. .11
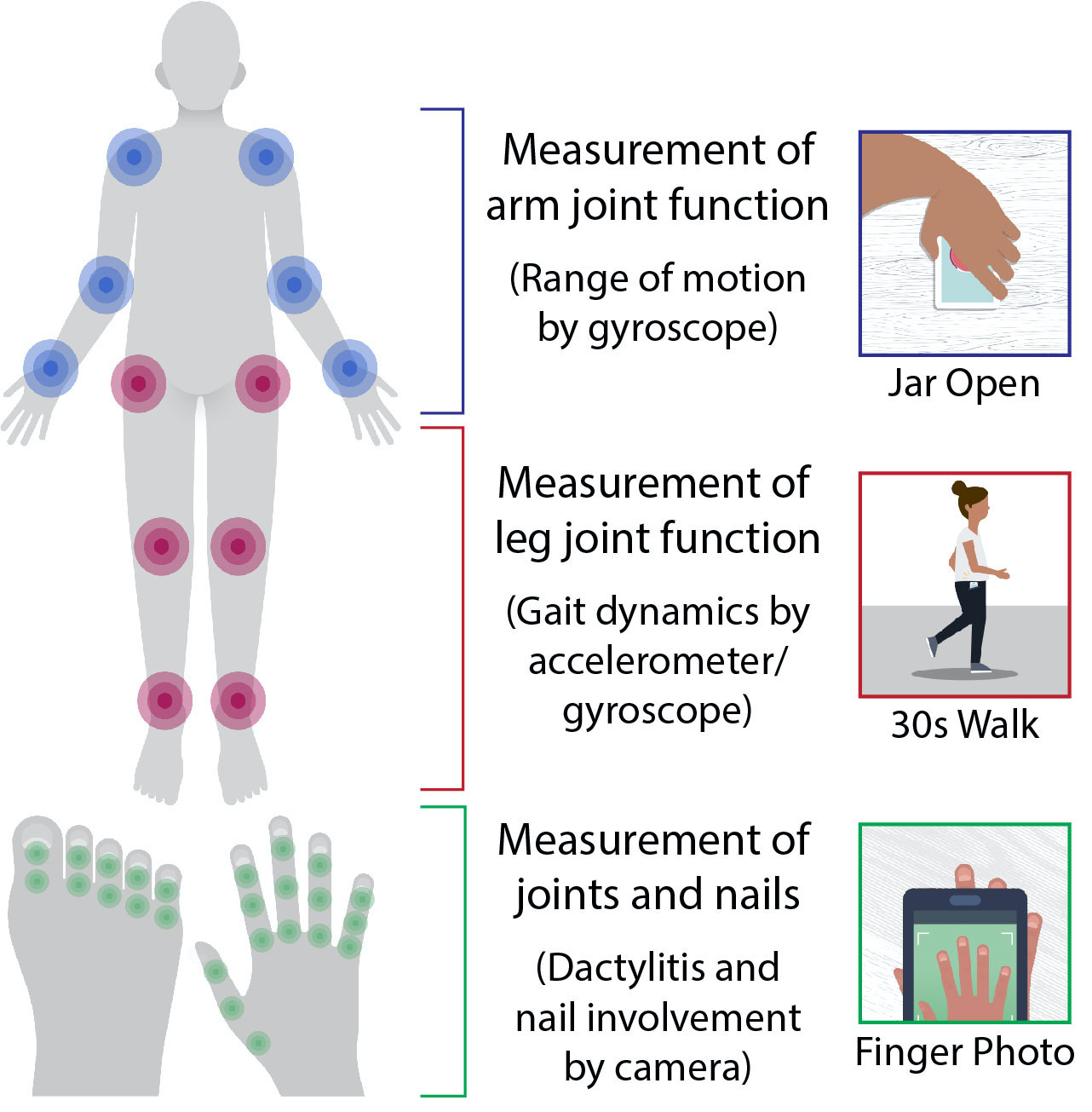
Figure 2: Presenting features of psoriatic arthritis.13
You May Like: Is Calcium Good For Rheumatoid Arthritis
Psoriatic Arthritis Blood Test: Anti
Blood tests that look for the presence of anti-cylic citrullinated peptide antibodies , which are inflammatory, are commonly used to diagnose rheumatoid arthritis, but anti-CCPs can also indicate psoriatic arthritis.
Roughly 8 to 16 percent of people with psoriatic arthritis will test positive for anti-CCPs, says Rubenstein.
Frequency of Testing Some physicians will perform the test yearly, says Cadet.
Treatment For Psoriatic Arthritis
Treatment for psoriatic arthritis aims to:
- relieve symptoms
- slow the conditions progression
- improve quality of life
This usually involves trying a number of different medicines, some of which can also treat the psoriasis. If possible, you should take 1 medicine to treat both your psoriasis and psoriatic arthritis.
The main medicines used to treat psoriatic arthritis are:
- non-steroidal anti-inflammatory drugs
Recommended Reading: Does Lidocaine Work For Arthritis
Also Check: How To Cure Arthritis In Hip
What Is Psoriatic Arthritis Video
Psoriatic arthritis can cause pain, swelling and stiffness inand around your joints.
It usually affects 3 in 10 people who already have the skin condition psoriasis .
Psoriasis causes patches of red, flaky skin which is covered with silvery-like patches.
Some people may develop psoriatic arthritis before the psoriasis is even present. In rare cases people have psoriatic arthritis and never have any noticeable patches of psoriasis.
Psoriatic arthritis and psoriasis are both autoimmune conditions, caused by a fault in the immune system.
Our immune system protects us from illness and infection. But in autoimmune conditions, the immune system becomes confused and attacks healthy parts of the body, often causing inflammation.
Psoriatic arthritis is a type of spondylarthritis. This is a group of conditions with some similar symptoms.
People with psoriasis are as likely as anyone else to get othertypes of arthritis, such asosteoarthritisorrheumatoid arthritis. Theseconditionsare not linkedto psoriasis.
Prognosis Of Psoriatic Arthritis
Estimating prognosis in PsA is difficult due to a lack of evidence and significant individual variability. PsA can evolve over time with variable joint and extra-articular involvement, according to multiple investigations. The pattern of peripheral joint disease appears to evolve with time, with oligoarthritis being more common in early disease patients than late disease individuals. In majority of the cases, increasing disease duration leads to increased joint involvement, with a large proportion of individuals with monoarthritis or oligoarthritis progressing to polyarthritis. Axial involvement becomes more likely as the disease progresses.1
PsA is a disease that can cause severe morbidity and have a negative impact on patients quality of life. Some characteristics are thought to indicate a severe disease course and a poor prognosis. A high number of actively inflamed joints or polyarticular presentations, raised ESR, clinical or radiographical damage, loss of function and a lower quality of life are all indicators.11
Recommended Reading: What Does Rheumatoid Arthritis Feel Like In Fingers
Symptoms Of Psoriatic Arthritis
The severity of the condition can vary considerably from person to person. Some people may have severe problems affecting many joints, whereas others may only notice mild symptoms in 1 or 2 joints.
There may be times when your symptoms improve and periods when they get worse .
Relapses can be very difficult to predict, but can often be managed with medicine when they do occur.
Psoriatic Arthritis Vs Rheumatoid Arthritis
PsA and RA are both inflammatory forms of arthritis that occur due to the immune system attacking healthy body cells and tissues.
The key difference between the two conditions is that PsA involves the skin as well as the joints. Other differences include:
- Disease symmetry: RA affects joints on both sides of the body, whereas PsA may affect joints on one side of the body.
- Joints affected: RA typically affects the middle joints of the fingers and toes, while PsA typically affects the joints closest to the fingernails and toenails.
- Diagnostic markers: Blood tests for RA will usually reveal a positive RF or CCP antibody, whereas blood tests for PsA will typically reveal a negative RF and CCP. Doctors may use such tests to help differentiate between the two diagnoses.
Also Check: What Specialist Treats Rheumatoid Arthritis
Getting Tested For Psoriatic Arthritis
Testing for psoriatic arthritis is ordered by your doctor or a specialist, such as a rheumatologist, a doctor who specializes in joint diseases, or a dermatologist, a doctor whose specialty is treating the skin. Blood and urine specimens used in testing can be provided in a doctors office or laboratory.
Synovial fluid analysis involves collecting a small amount of joint fluid using a process called arthrocentesis. During this procedure, a needle is used to withdraw fluid from the space around a joint. It is usually done at a doctors office.
Some diagnostic imaging tests, like x-rays, may be done in a doctors office. Others may need to be performed at an imaging center or hospital radiology department.
Psoriatic Arthritis Blood Test: Anemia

When you have psoriatic arthritis, ongoing inflammation may cause anemia, a decrease in healthy red blood cells that can lead to dizziness, shortness of breath, and exhaustion, says Cadet.
By measuring your blood levels of hemoglobin , your doctor can determine if you have anemia. A normal reading for women is 12 to 16 grams of hemoglobin per deciliter of blood 14 to 18 grams is normal for men, according to the Mayo Clinic.
If blood work reveals anemia, your doctor will give you an exam and other blood tests to find the cause. In people with psoriatic arthritis, treatments that reduce inflammation also help with anemia, explains Cadet.
Frequency of Testing Doctors may order tests to be done several times a year to see if the anemia has worsened or improved.
Additional reporting by .
Read Also: What Is Advanced Rheumatoid Arthritis