Can Psoriatic Arthritis Attack Other Organs Of The Body
Apart from the skin, nails and joints, increased cardiovascular morbidity is considered part of psoriatic disease, as is the association with inflammatory bowel disease. An itchy, red eye due to conjunctivitis is more common in people with psoriatic arthritis and some people occasionally develop a painful, red eye caused by inflammation around the pupil of the eye, which is called iritis or uveitis. Anaemia may also be found but this is the result of long-term inflammation and is not a specific feature of psoriatic arthritis.
How To Get The Right Arthritis Diagnosis
There is no single test for psoriatic arthritis, says Azar. Along with a physical exam, youll likely need a series of both imaging procedures and blood tests for a diagnosis, and to rule out other forms of arthritis, such as rheumatoid arthritis or gout.
Theres no one test to diagnose rheumatoid arthritis either, but, as with PsA, blood tests are part of the workup. The presence of autoantibodies in the bloodstream, either rheumatoid factor or cyclic citrullinated peptide antibodies, will suggest an RA diagnosis. These antibodies tend to be less typical in people with psoriatic arthritis, according to an article published in Rheumatic and Musculoskeletal Diseases in August 2018.
As part of the physical exam, the doctor will closely evaluate the affected joints. RA involves the joints in a symmetrical fashion, and often, when rheumatoid factor is very high, there may be nodules under the skin, Azar says. According to the National Rheumatoid Arthritis Society, 20 percent of patients with RA develop these firm lumps.
Psoriatic arthritis, on the other hand, can reveal itself in a variety of ways, affecting a large joint or a single small finger joint of the hand, says Azar.
Another notable difference between the two diseases is bone involvement. RA is characterized by bone loss or erosion near the joint, while PsA is marked by both bone erosion and new bone formation, Azar says. An X-ray or other imaging method can help reveal whats going on.
Medications For People With Rheumatoid Arthritis
Inflammation in RA is associated with a different interleukin than those in PsA. The IL-6 inhibitor drugs Actemra and Kevzara work against RA, but have not been proven to help with PsA.
In addition, Rituxan and Kineret can be helpful for RA that has not responded to other types of treatment. However, these drugs are not useful in treating PsA.
You May Like: How To Deal With Arthritis
Symptoms Of Seronegative Rheumatoid Arthritis
Seronegative rheumatoid arthritis patients must possess a distinct set of symptoms in order to be diagnosed. This is because the lack of antibodies in the blood makes it more difficult to reach a rheumatoid arthritis diagnosis.
Some of the most important symptoms in diagnosing seronegative rheumatoid arthritis include:
- Joint pain, stiffness specifically in the hands but also in knees, elbows, hips, feet and ankles
- Joint swelling and redness
- Morning stiffness lasting longer than 30 minutes
- Fatigue
- Eye redness
Though this is not an exhaustive list, the majority of these will support a rheumatoid arthritis diagnosis. If we compare these symptoms to seropositive rheumatoid arthritis symptoms, there are many similarities. However, many patients see these symptoms evolve and change over time.
It is thought that seropositive patients experience a more severe disease course than seronegative patients. But studies have also shown that in some patient cases, the progression is comparable and sometimes is there is little difference. This is where it becomes complicated in trying to classify rheumatoid arthritis into sub-types and to reach a solid diagnosis.
There are some symptoms that are thought to be rheumatoid arthritis in seronegative patients, but later turn out to be other conditions. These cases mainly involve differences in the types of joints and areas affected as well as the levels of inflammation.
Causes Of Psoriatic Arthritis
Almost 1 in 3 people with psoriasis also have psoriatic arthritis.
It tends to develop 5 to 10 years after psoriasis is diagnosed, although some people may have problems with their joints before they notice any skin-related symptoms.
Like psoriasis, psoriatic arthritis is thought to happen as a result of the immune system mistakenly attacking healthy tissue.
But it’s not clear why some people with psoriasis develop psoriatic arthritis and others do not.
Don’t Miss: What Can You Do To Help Arthritis In Your Hands
What Is Seronegative Rheumatoid Arthritis
When a patient tests negative for RF and anti-CCP antibodies, yet they still display strong symptoms consistent with rheumatoid arthritis, they are given a diagnosis of seronegative rheumatoid arthritis.
The term seronegative means they dont possess the antibodies that seropositive patients do. In other words, seronegative patients may also simply possess extremely low levels of the antibodies not enough for the test to detect.
Many seronegative rheumatoid arthritis patients go on to develop antibodies years after their initial diagnosis, which then changes their diagnosis to seropositive rheumatoid arthritis. This is one of the many reasons that a patient can still be diagnosed with rheumatoid arthritis even if they are seronegative.
What Can I Do To Help My Feet
The most important action is to seek advice and help when you notice any changes in your foot, whatever they may be. You can talk to your GP or local pharmacist for advice. Some problems can be resolved simply. For issues that are more persistent you may be referred to a specialist, such as a dermatologist, rheumatologist, physiotherapist, surgeon or chiropodist/podiatrist.
For general foot care, personal hygiene is important, particularly in avoiding fungal and viral infections. Change shoes and socks regularly, avoid shoes which are ill-fitting or cause bad posture. If you are overweight, losing weight could relieve the pressure on your joints and improve your walking gait.
If you are diagnosed with psoriasis, develop a treatment regime that works for you often, applying treatment after a bath or shower, along with the use of an emollient, can make the process easier.
If you have nail involvement, keep nails trimmed and clean. If they are thick, try trimming them after soaking them in a bath or shower, as this makes them softer and easier to cut. Alternatively, seek an appointment with a chiropodist, which is often available via the NHS.
If you have psoriatic arthritis, it is important to rest inflamed joints. Sourcing footwear that supports the foot and helps to reduce the pressure on the inflamed areas can help, as can inner soles and orthotic supports. Once again, a chiropodist is best placed to advise you.
This article is adapted from The psoriatic foot leaflet.
You May Like: Symptoms Of Arthritis In Your Hands
What The Hot Feeling Feels Like
We were first tuned into this symptom by CreakyJoints member Frances D., who has psoriatic arthritis. When she posted about it on , she got a ton of responses from fellow patients. I feel hotter than most people constantly, she told us when we asked her more about it. Sometimes at night I wake up sweaty with damp sheets. Often at night and sometimes during the day, my feet feel like they are on fire and are burning. My hands are usually warm when everyone else has cold hands. Ive mentioned it to three rheumatologists, and they didnt offer any explanation or remedy.
When we asked about this symptom on Facebook, we got an overwhelming response from the CreakyJoints community. I will go from fine to feeling like Im on fire in a matter of seconds. This has been happening for several years, since being diagnosed, Rene Marie B. told us. My face and scalp sweat the most and I can be around people who say its not hot while Im dripping sweat. At night I have blankets on and off a million times. I hate it.
Nearly all the responses echoed similar situations. Yes, this happens to me every day. My face feels like its going to catch fire its so hot, Diana M. shared. Its embarrassing when you are out around people and they ask if you are all right. I just feel like I want to sit on a block of ice and everyone else has their coats on. Very frustrating!
What Are The Causes Of Psoriatic Arthritis And Rheumatoid Arthritis
We don’t have an understanding of what causes many autoimmune conditions, including RA and PsA, but there are common links among people who develop these diseases.
“We don’t know exactly what causes RA or PSA, but we do know there are genetic components and stress components to both,” Magdalena Perez-Rivera, MD, rheumatology specialist with Conviva Care Centers tells Health.
Here are some of the primary risk factors for RA and PsAyou’ll see there is a good amount of overlap.
Don’t Miss: Rheumatoid Arthritis In Lower Back Symptoms
Monitoring And Diagnosis For Fatty Liver Disease
Since there are few to no symptoms of NAFL, doctors must determine which patients are at increased risk when deciding to monitor for the condition. Many dermatologists routinely screen their psoriasis patients. Some rheumatologists make liver testing a routine part of their practice, too. I always do a liver function panel at baseline to make sure patients are ready if I need to put them on meds, says Dr. Bose. The blood tests are also used for monitoring drug treatment.
Other rheumatologists screen or monitor for NAFLD on a case-by-case basis. Somebody who is taking a high dose of methotrexate. Somebody with psoriasis who also has type 2 diabetes. Someone age 50 or older with diabetes and another inflammatory condition. In cases like these its probably reasonable for the liver to be evaluated, says Dr. Loomba.
A blood test with a complete metabolic profile is the first step. Ask What is my ALT , advises Dr. Loomba. ALT is an enzyme primarily found in the liver high levels in the blood may indicate a liver problem. Imaging scans like ultrasounds, CTs, or MRIs can diagnose NAFLD. In fact, many times NAFLD is detected incidentally, when someone has an abdominal scan for another reason.
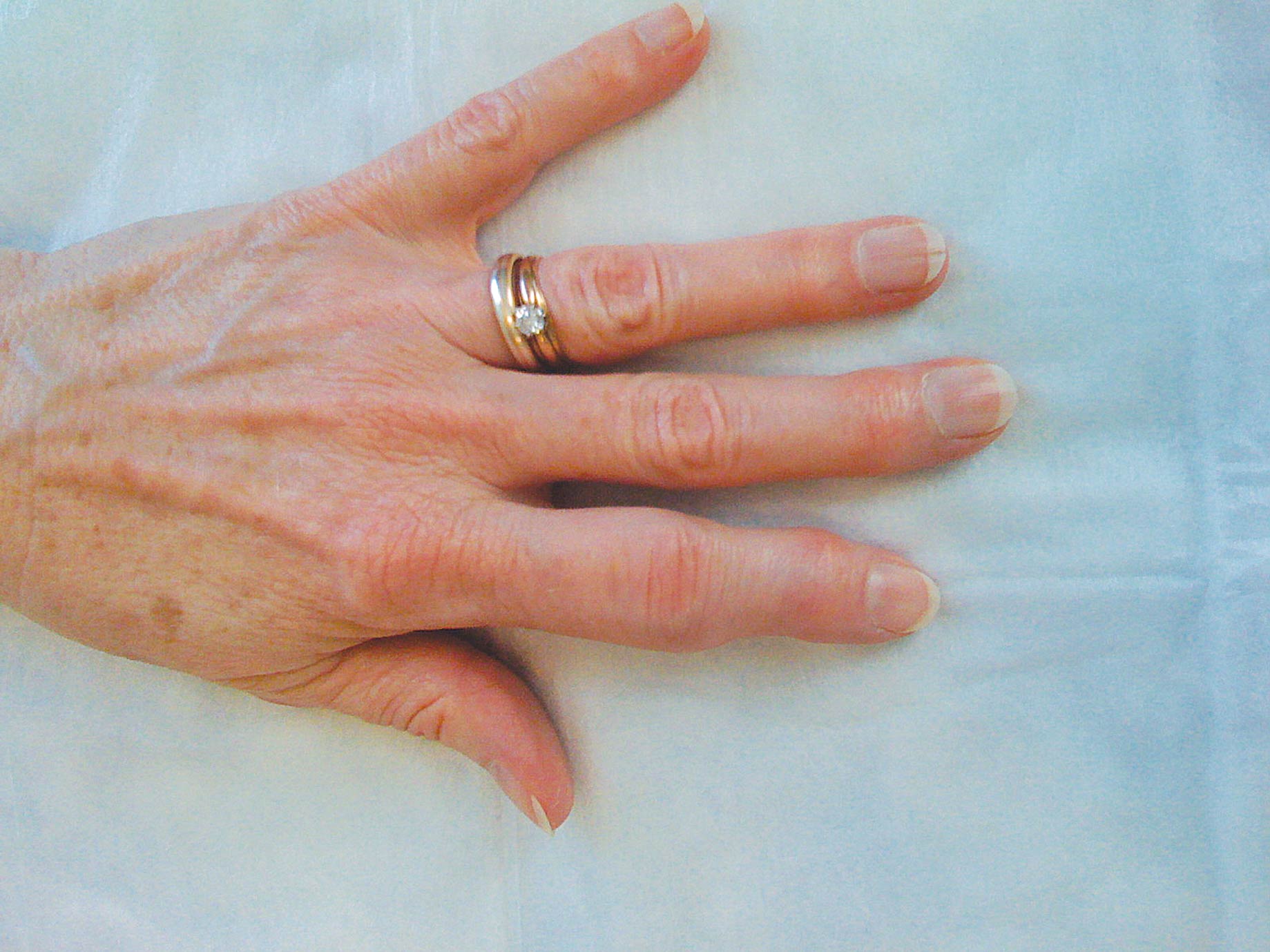
Fingers Toes And Skin
Another telling clue is the presentation of the disease on the fingers and toes. With PsA, the distal joints will be the focus of pain, swelling, and stiffness. By contrast, RA primarily involves the proximal joints .
With severe PsA, the fingers can also take on a sausage-like appearance , making it difficult to ball your fist. While this can occur with RA, it is not the hallmark that it is with PsA.
Around 85% of people of PsA with also have the most typical form of psoriasis, characterized by dry, flaky skin plaques. Moreover, half will have nail psoriasis at the time of their diagnosis. Neither of these occurs with RA.
Recommended Reading: Ra Symptoms In Knees
Living With Psa And Fibromyalgia
Last year, Diane Talbert of Waldorf, Maryland, who has lived with psoriatic disease for 30 years was diagnosed with fibromyalgia, a disorder characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory, and mood issues.
I think it is very common to have at once. It just gets missed by our doctors, says Talbert. The biggest change I noticed was brain fog and fatigue. I felt like my psoriatic arthritis was getting worse. I was having more pain, stiffness, and tenderness in my muscles. It felt like the pain was all over my body. I know with my psoriatic arthritis I had pain also, along with swelling, but the tenderness is in certain joints.
Talbert stresses that patients have to be aware of changes in their bodies so they can get the proper diagnosis. She started keeping a journal when she noticed she was having symptoms that were different from her usual psoriatic arthritis.
I was feeling pain in different parts of my body, and the pain would get worse even after I rested, she says. I couldnt sleep but two or three hours. I was tired all the time and couldn’t move like I used to. I would get restless legs along with numbness.
Talbert now takes one medication for her PsA and a different one for her fibromyalgia.
Theres a higher rate of uric acid formation in patients who have active psoriasis because of the cellular turnover and that may increase the rates of gout in that population, he says.
What Are The Symptoms Of Psoriatic Arthritis And Rheumatoid Arthritis

Most people who develop psoriatic arthritis show the skin symptoms of psoriasis first, although some individuals experience PsA without ever having psoriasis symptoms. About 30 percent of people with psoriasis will eventually develop PsA.
The severity of a persons psoriasis symptoms is not linked to the severity of their PsA symptoms. Some people may have severe psoriasis skin lesions but mild PsA symptoms, and others may have mild skin lesions but severe PsA joint pain.
You May Like: Mild Psoriatic Arthritis Rash
Can Psoriatic Arthritis Affect Children Too
As many as 12,000 children in the UK are affected by arthritis. It is known as juvenile chronic arthritis , of which there are three main types, stills disease, polyarticular juvenile chronic arthritis and polyarticular onset juvenile chronic arthritis. Psoriatic arthritis is a minor subset of JCA and is uncommon.
Blood Tests For Psa And Ra
Blood tests can also help tell the difference between PsA and RA.
About 80 percent of people with RA are said to have seropositive RA, which means they test positive for rheumatoid factor or for cyclic citrullinated peptide antibodies.
Most people with PsA do not have RF or CCP antibodies and are considered seronegative. However, it is also possible to have seronegative RA.
Also Check: Finger Arthritis Relief
Managing Symptoms Of Autoimmune Arthritis
Several medications work for both psoriatic arthritis and rheumatoid arthritis:
- Nonsteroidal anti-inflammatory medications reduce pain and swelling.
- Disease-modifying antirheumatic drugs protect joints and slow the disease, and less of the joint is destroyed, meaning theres less swelling, pain and less loss of joint function.
- Biologics target the specific parts of the immune system that drive inflammation.
As researchers learn more about the causes of inflammatory arthritis, theyre developing new medications to manage these diseases. Some of these new drugs are designed to specifically target one disease or the other.
Both psoriatic arthritis and rheumatoid arthritis are chronic diseases. They cant be cured, but they can be managed, Dr. Rosian says. By working with your doctor to get the correct diagnosis, you can manage symptoms to feel your best.
What Causes Ra And Psa
RA runs in families. If you have a close relative with the disease, your chances of having it are higher. Women are more likely than men to get RA. Usually the symptoms start between ages 40 and 60.
PsA also runs in families. Certain genes may be linked to the condition. Compared to RA, PsA often starts between ages 30 and 50.
Researchers don’t know exactly what triggers either type of arthritis. But they think it probably comes from a mix of genes and other factors, including hormones and bacterial or viral infections that may send the immune system into overdrive.
Read Also: How To Get Rid Of Arthritis In Wrist
Is There A Typical Psoriatic Arthritis
Eighty-percent of the time, psoriasis symptoms appear first. However, in some patients, the psoriasis is barely even perceptible. Or only the nail tissues may be affected.
Like RA, PA symptoms can vary greatly between patients. Psoriatic Arthritis may be symmetrical or asymmetrical. The spine and sacroiliac joints may or may not be involved. Fingers and toes may swell into a sausage-shaped deformity called dactylitis. A very destructive hand deformity called arthritis mutilans is caused by destruction of joint tissue.
How Are Psa And Rheumatoid Arthritis Similar Yet Different
Psoriatic arthritis and rheumatoid arthritis are autoimmune diseases, in which the immune system mistakenly attacks healthy cells, causing swelling, pain, and stiffness in the joints.
Psoriatic and rheumatoid arthritis are similar but separate diseases, sometimes with manifestations that look quite similar, says , the director of the rheumatology clinic at Stanford Health Care in Palo Alto, California. In general, the two diseases do not coexist together.
Dr. Genovese points out, however, that during the months or even years when the arthritis is first developing, the type of arthritis a patient has may be unclear.
One of the features that distinguishes psoriatic arthritis from rheumatoid arthritis is dactylitis, according to Jason Faller, MD, a rheumatologist at Lenox Hill Hospital in New York City. With this condition, fingers or toes swell and take on a sausage-like appearance.
Enthesitis, or inflammation of the areas where ligaments or tendons enter into the bones, is also a characteristic of psoriatic arthritis that does not occur in rheumatoid arthritis or osteoarthritis.
As many as 30 percent of individuals who have psoriasis develop psoriatic arthritis, according to the National Psoriasis Foundation. Signs of the condition, such as red, scaly skin, can help doctors differentiate PsA from RA.
Often both types of arthritis benefit from anti-inflammatory medications such as nonsteroidal anti-inflammatory drugs , corticosteroids, and immunosuppressants.
Also Check: Arthritis In Arms Symptoms
Other Possible Explanations For Feeling Hot With Arthritis
A couple people we heard from on Facebook noted that in addition to inflammatory arthritis, they also have something called autonomic dysfunction. This occurs when the body isnt properly managing the autonomic nervous system , which controls subconscious functions like breathing and surprise body temperature. The Cleveland Clinic lists autoimmune conditions like rheumatoid arthritis as a secondary cause of autonomic dysfunction one journal paper even suggests that the autonomic dysfunction may precede RA.
But this still doesnt answer the question of why.
Another study suggested that inflammation from rheumatoid arthritis may affect the brain, although that research looked more specifically at the development of cognitive dysfunction and fatigue. But, through the field of psycho-neuroimmunology, we now understand that immune cells do reside in the brain as well as the rest of the body, so all of these systems are connected, says Hillary Norton, MD, a rheumatologist in Santa Fe, New Mexico.
Since the brain plays a key role in regulating body temperature, perhaps if inflammatory conditions like arthritis affect brain function, it could help explain the link between inflammatory arthritis and body temperature fluctuation. But this is all still theoretical and more research is needed.