Rheumatoid Arthritis Jaw Pain Relief
Aside from medications, there are supportive care measures you can take to help relieve TMJ pain from rheumatoid arthritis, especially during flare ups. These measures include:
- Jaw exercises: Physical therapy exercises for the jaw can help improve mobility and decrease pain.
- TMJ diet: A TMJ diet optimized for rheumatoid arthritis will include soft foods, avoid hard foods, and be anti-inflammatory.
- Hot/Cold therapy: Alternating hot and cold therapy on the joint can help with pain and mobility.
- Oral Splint Therapy: Anterior bite blocks are a type of mouth guard that can be used temporarily to relieve jaw tension and pain.
The resources listed above are available as part of the Speed2Treat Home Healing Kit. This kit can be invaluable for treating inflammatory flare-ups of TMJ rheumatoid arthritis. Start your journey towards TMJ pain relief with the Home Healing Kit today!
Founder and CEO of Orofacial Therapeutics
- Ann C McCulloch
Recommended Reading: Does Collagen Help Psoriatic Arthritis
Can Rheumatoid Arthritis Affect Your Jaw
Rheumatology Arthritis
Rheumatology arthritis is an autoimmune disease caused by an overactive immune system. This inflammatory condition affects your joints and causes severe pain and inflammation. Seeking medical help immediately is very important if you are diagnosed with rheumatology arthritis because this autoimmune condition can lead to joint damage and immobility.
One important thing you need to note is that rheumatoid arthritis can affect your jaw also. When it affects your jaw, you will experience stiffness, tenderness, and severe pain when you chew your food. In advanced cases of rheumatoid arthritis, the joint may make noises when moving and it will be very painful.
Can Jaw Pain Go Away On Its Own
Pain in the jaw is not too likely to be seen as a serious issue as long as your jaw doesnt ache for a longer period. However, if we know the cause of jaw pain, it could be treated with some combination of medication.
It is something you would not need to worry about. Sometimes, the cause may be as common as stress which makes your teeth grind and your jaw clench which would treat itself better.
Meanwhile, jaw pain is of several ranges starting from mild to severe that depending on if it could go away on its own.
Also Check: Can Arthritis In The Spine Be Cured
Also Check: How Do I Know What Type Of Arthritis I Have
Psoriatic Arthropathy Of The Temporomandibular Joint
Traditionally, TMJ involvement in PA has been thought to be rare with fewer than 40 cases reported in the last 50 years. However, some studies have suggested that dysfunction occurs in 90% patients with PA . More recently, Dervis and Dervis found the TMJ to be symptomatic in 29% and 35% of patients with psoriasis and PA, respectively. This incidence is no higher than that found in the general population without psoriasis therefore, PA does not necessarily increase the risk of TMJ dysfunction. However, when it occurs, the symptoms tend to be worse. PA can also affect the TMJ in the form of monoarthritis, rather than polyarthritis in 0.010.2% of the population .
The duration and severity of PA and the number of somatic joints affected are the main risk factors for TMJ symptoms and signs, but the degree of skin involvement is not . Typical findings include clicking, crepitus, or other joint sounds TMJ pain on mouth opening and chewing morning stiffness and muscle tenderness . As the disease progresses, pain is replaced by the limitation of movement due to the development of fibrosis. Like RA, crepitus is found in the latter stages and is associated with structural joint changes, which may progress to joint collapse or ankylosis.
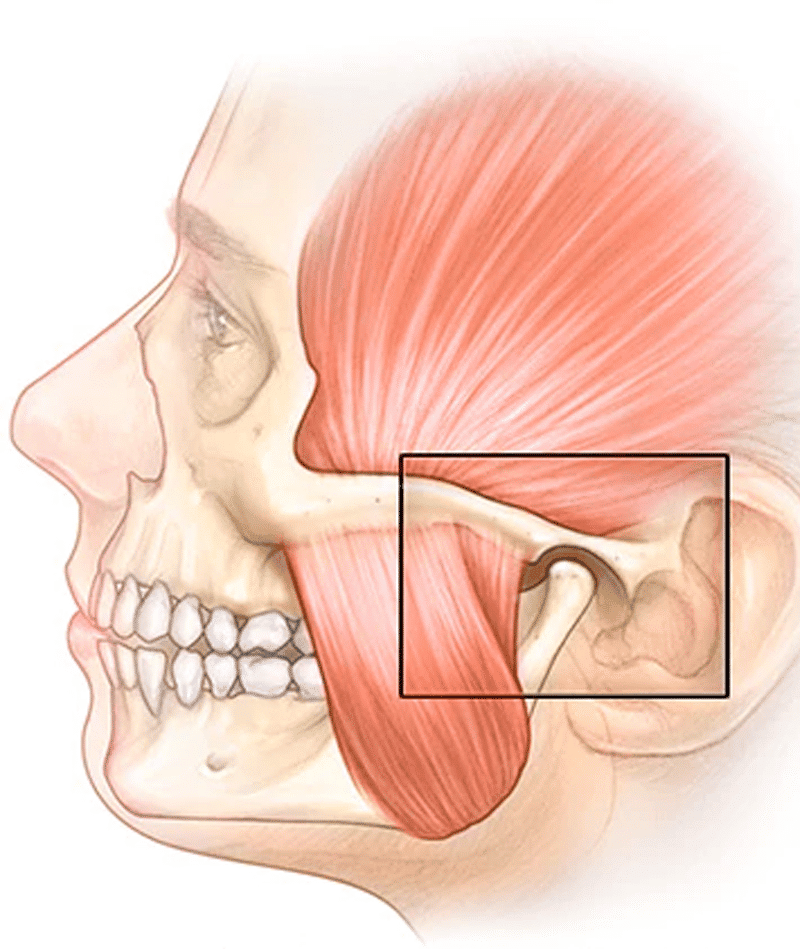
What Is The Temporomandibular Joint

The temporomandibular joint is the joint that connects the jaw to the skull. There is a TMJ on each side of the face, in front of each ear. These joints allow the movements needed for speaking, eating and facial expression.
TMJ dysfunction can cause pain, abnormal jaw movements and joint noises. They are quite common.
Read Also: Does Otezla Treat Rheumatoid Arthritis
What Are The Temporomandibular Joints
The temporomandibular joints are the 2 joints that connect your lower jaw to your skull. More specifically, they are the joints that slide and rotate in front of each ear, and consist of the mandible and the temporal bone . The TMJs are among the most complex joints in the body. These joints, along with several muscles, allow the mandible to move up and down, side to side, and forward and back. When the mandible and the joints are properly aligned, smooth muscle actions, such as chewing, talking, yawning, and swallowing, can take place. When these structures are not aligned, nor synchronized in movement, several problems may occur.
This Is How The Jaw Joint Is Constructed
Your jaw is one of the most flexible joints of your body. The upper jaw cannot be moved and is firmly attached to the skull. Just in front of your ear is the joint that forms the connection with the lower jaw. The end of the lower jaw protrudes into the joint, with a cartilage disc in between, called discus, surrounded by ligaments and tendons to keep the joint in place. The chewing muscles cause your lower jaws to move in every direction. Not only open and close, but also front to back and left to right. This allows your teeth to efficiently grind your food.
Read Also: What Causes Rheumatoid Arthritis Symptoms
Home Remedies For Jaw Pain
Jaw pain is seen as a basic and general thing for all, especially women. And it has several home remedies to be taken care of. It helps you through difficult times instantly. So make sure you do what is mentioned below:
Switch your diet to soft foods.
Do not chew gums or any other object.
Let your jaw relax.
Help your jaw to compress using warm or cold water.
Stretch your jaw by trying out exercises.
Avoid stress.
You May Like: How Does It Feel To Have Rheumatoid Arthritis
How Is The Condition Treated
Temporomandibular joint dysfunction can be treated by addressing the underlying causes, such as controlling the stress that may be causing you to grind your teeth or taking medication that can relieve arthritis inflammation.
Self-treatment for TMJ can be helpful as well. TMJ exercises, for one, can both loosen and strengthen the joints and surrounding structures. Other options for self-care of temporomandibular joint dysfunction include:
- Eating softer foods
- Applying heat packs to the area
- Practicing relaxation techniques to control jaw tension, such as meditation
Dental treatments for temporomandibular joint dysfunction include creating a mouthguard that can protect your teeth while you sleep at night. The dentist also may prescribe medications such as muscle relaxants, analgesics, anti-anxiety drugs, or anti-inflammatory medications.
The first step, however, is pinpointing whats causing your condition. From there, we will determine whether the disorder itself must be treated or its causes must be addressed. Make an appointment with Dr. Holtzman for a review of your symptoms. Fortunately, many of the causes and symptoms of TMJ are highly treatable, and the results can offer tremendous relief.
Read Also: Where Do You Feel Hip Arthritis Pain
Recommended Reading: What Is The Normal Dose Of Methotrexate For Rheumatoid Arthritis
Use An Occlusal Splint
Also known as an intra-oral appliance, this is a type of mouthguard. It can help ease pain by allowing the chewing muscles to rest in a neutral position, relieving pressure on the jaw.
The appliance should not result in any changes to the teeth or bite. However, it is unclear how effective these appliances are.
Local Anesthetic And Steroid Injections
Pain emanating from the TMJ can be confirmed, and temporarily relieved, by infiltration of local anesthetic into the joint space. Resolution of the pain after 10 min establishes an intra-articular etiology rather than a muscular source. The site of injection is 10 mm along and 2 mm inferior to a straight line from the tragus to the lateral canthus of the eye .
Don’t Miss: How Much Is Tylenol Arthritis At Walmart
Early Detection Is Key
Itâs up to you to reach out to your rheumatologist, dentist, general practitioner or other health care provider if you think thereâs a problem. While Primackâs story of struggling to find a doctor who could correctly diagnose her PsA is an exception â and while more than a third of PsA patients will experience some symptoms in their TMJ â medical professionals could do a better job of identifying issues in the jaw, says Orbai.
âIn clinical practice, rheumatologists arenât necessarily used to looking at the TMJ. They are part of the 66/68 joint count, which was just recently recommended as a best practice measure for clinical trials, longitudinal studies and even in clinical practice,â Orbai says. âBut most people in practice will just look at patientsâ hands. Because practitioners arenât doing the full joint count, they may miss the TMJ.â
Itâs a matter of rheumatologists getting in the habit of checking the full range of joints, and patients bringing up the range of their symptoms, which Orbai says is happening more frequently today than it was when Primack first began experiencing joint pain.
Thatâs why projects like the NPF PsA Diagnosis Project are so important. The PsA Diagnosis Project aims to create a reliable diagnostic test to catch psoriatic arthritis early. Whether in the jaw, knee, foot or any other joint, an early diagnosis can help you get the treatment you need as soon as possible.
Dealing With Arthritis In The Jaw Joint
My boyfriend and I were binge-watching The Mandalorian on a recent Sunday morning. I was so relaxed that I let out a big yawn. But as I opened my mouth, my jaw made a loud cracking sound. My boyfriend looked terrified and asked if anything was broken. I admit it did sound like something had snapped. But I was OK, the cracking sound was due to stiffness caused by arthritis in my jaw.
Its common for kids with juvenile idiopathic arthritis to have arthritis in their temporomandibular joint , or jaw. Pediatric rheumatologists often check their patients jaws because symptoms can be silent or mild at first. I remember my doctor palpating my jaw long before I had issues, and Im glad we caught my problems early.
Don’t Miss: Are Apples Good For Rheumatoid Arthritis
Are There Alternative Tmj Treatments Available
Many healthcare providers recommend using alternative therapies in combination with traditional treatments. These therapies may include:
- Relaxation techniques. Mindfulness or meditation can help you slow your breathing and relax tense muscles. As a result, pain can be reduced.
- Acupuncture. This technique involves inserting thin needles into the body at various points. Acupressure points may trigger the central nervous system and stimulate your bodyâs natural healing processes.
- Biofeedback. Electronic instruments can be used to detect areas of stress and tightness in your body. This gives you a greater awareness of where youâre holding tension so you can focus on relaxing these muscles.
- Pain management referrals. In some cases, you may be referred to a pain psychologist or pain management clinic to help ease your symptoms.
Is Tooth Grinding A Cause Or Effect Of Tmj
Its both. If you have a habit of grinding or clenching your teeth, this may irritate your jaw.
On the other hand, if you are experiencing jaw pain for another reason, this pain may cause you to involuntarily grind or clench your teeth. In that case, its a never-ending cycle, so our dentist and your general physician should help you pinpoint the source of your condition.
Also Check: Does Rheumatoid Arthritis Cause Itchy Skin
Lockjaw Syndrome: How To Recognize The Symptoms And Seek Treatment
Have you ever experienced jaw locking or difficulty opening your mouth? This can be a sign of lockjaw syndrome.
The causes of lockjaw syndrome vary, including poor posture, bruxism , jaw injury or trauma, arthritis, and stress. This article will discuss the symptoms, diagnosis, and treatment of lockjaw syndrome.
Treatment Of Osteoarthritis In The Jaw
We cannot say it often enough: cartilage that has disappeared will never return. The most important advice of the doctor will be to give the jaw joint as much rest as possible. Measuring a biting plate which needs to be worn at night can help keep the tension of the chewing muscles under control. The chances are that without treatment most symptoms will disappear automatically over time. In the tissue string behind the discus, scar tissue will develop which will take over the function of the damaged or lost cartilage. The jaw can then usually be moved to a sufficient extent. In severe cases bone growth may occur in order to distribute pressure on the joints over a large area. This can cause the jaw to no longer be moved. Then a surgical procedure is required, in which an artificial joint is placed in very rare cases.
You May Like: What Type Of Turmeric Is Best For Arthritis
How Doctors Diagnose Arthritis Jaw Pain
The underlying causes for jaw pain can be hard for doctors to suss out, as the TMJ is a very complex joint with multiple factors affecting it. Your rheumatologist or dentist may recommend a specialist who deals with TMJ disorders, called an oral and maxillofacial surgeon. A thorough comprehensive evaluation and history taking is crucial to accurately diagnosing the etiology of jaw pain, Dr. Levi says.
Osteoarthritis is often diagnosed based on symptoms and imaging, and is commonly is associated with joint sounds, known as crepitus, Dr. Levi says. Osteoarthritis is also often associated with morning stiffness, jaw tightness, and decreased range of motion of the jaw.
Jaw bone and cartilage changes due to arthritis may be seen on imaging tests such as an X-ray, CT scan, or MRI. Changes that can be visualized on imaging include condylar beaking or flattening , and decreased joint space, Dr. Levi says.
Other forms of arthritis, such as rheumatoid arthritis, may be diagnosed with help from blood tests, Dr. Levi says. With inflammatory or autoimmune diseases, you will have elevated inflammatory markers like c-reactive protein or erythrocyte sedimentation rate many rheumatoid arthritis patients also test positive for antibodies such as rheumatoid factor and anti-CCP.
But if you have inflammatory arthritis, chances are jaw pain wont be your first symptom and if youve already been diagnosed, your doctor will have an indication that jaw pain may be due to your condition.
Arthritis: A Common Cause Of Tmj Disorders
by headpain | Jul 14, 2021 | TMJ / TMD
If you are experiencing discomfort in your jaw, headaches, and ear pain, they might be signs of arthritis, which is also a common cause of TMJ disorders. Arthritis can affect the joint where the skull and jaw meet, which is known as the temporomandibular joint . The joint allows your jaw to function and move, and acts like a hinge.
Read Also: Can Psoriatic Arthritis Affect Your Eyes
What Are The Symptoms
TMD often causes severe pain and discomfort. It can be temporary or last many years. It might affect one or both sides of your face. More women than men have it, and itâs most common among people between the ages of 20 and 40.
Common symptoms include:
- Pain or tenderness in your face, jaw joint area, neck and shoulders, and in or around the ear when you chew, speak, or open your mouth wide
- Problems when you try to open your mouth wide
- Jaws that get “stuck” or “lock” in the open- or closed-mouth position
- A tired feeling in your face
- Trouble chewing or a sudden uncomfortable bite — as if the upper and lower teeth are not fitting together properly. Learn more about the pros and cons of teeth alignment surgery.
- Swelling on the side of your face
You may also have toothaches, headaches, neck aches, dizziness, earaches, hearing problems, upper shoulder pain, and ringing in the ears .
What Types Of Arthritis Affect The Jaw
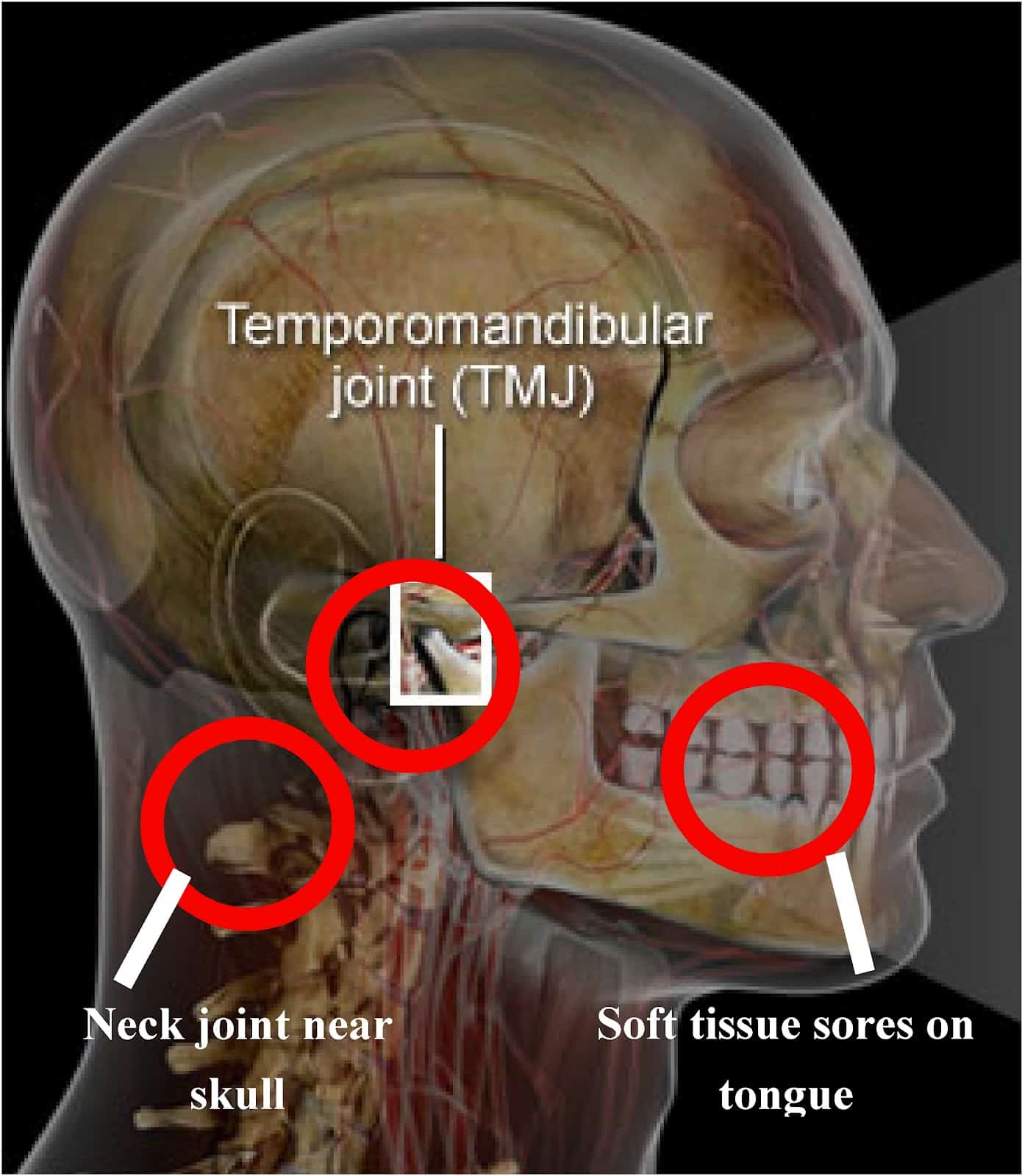
The joint responsible for jaw pain is the temporal mandibular joint . This is where the lower jaw hinges at the level of the ear, Dr. Bykerk says. Responsible for talking as well as eating, the TMJ is the most frequently used joint in the body. This frequency of use also makes the jaw susceptible to different kinds of arthritis.
Like other joints, the TMJ is at risk for osteoarthritis, along with other types of arthritis such as rheumatoid arthritis, says Lauren Levi, DMD, dentist at The Mount Sinai Hospital in New York City. Osteoarthritis is the most common type of arthritis that affects the TMJ.
Some people may be more at risk for arthritis in the jaw than others. Macro or microtrauma, through grinding or clenching, along with decreased lubrication in the joint may increase the risk for developing arthritis, Dr. Levi says.
Stress and chronic pain in the body, such as may occur with arthritis elsewhere, can cause clenching so in a vicious cycle, jaw pain and arthritis may become a chicken or the egg scenario, Dr. Bykerk says.
People will clench if they have pain, if they are stressed, or pain can result if they clench too much or grind their teeth, called bruxism, she says. If bruxism and clenching go on too long the TMJ can wear out, the cartilage in the joint can break down and degenerative arthritis occurs.
Read Also: What Is Degenerative Arthritis In The Neck
How Can I Reduce Inflammation In My Jaw Joint
Apply a hot or cold compress to the affected area. Ice can assist to reduce swelling and pain, while heat can help to stimulate blood flow and relax the muscles in your mouth. Apply a hot or cold compress to your jaw for 15 to 20 minutes at a time, ensuring that just a thin layer of skin is between the compress and your skin. Repeat this process several times.
Dont Miss: Are You Born With Rheumatoid Arthritis