Chest Pain Or A Racing Pounding Heart
Inflammation from rheumatoid arthritis may worsen or trigger heart problems. These heart problems include, but may not be limited to:
- Coronary heart disease, also known as coronary artery disease or clogged arteries, is 1.5 to 2 times more common in people with RA than in the general population.9 Coronary heart disease can lead to heart attack and stroke. It can cause a variety of symptoms, including shortness of breath and tightness in the chest, especially during physical activity.
- Pericarditis is inflammation of the delicate membrane that surrounds the heart, called the pericardium. Pericarditis can cause sudden chest pain and may be mistaken for a heart attack.
- Myocarditis is inflammation of the heart muscle itself. It can cause damage to heart tissue anddepending on severity and treatmentmay be life-threatening. Myocarditis symptoms vary and may include fatigue, shortness of breath, swelling , and chest pain. The heart may feel like it is racing, fluttering, or pounding.
A physician may refer to any one of these conditions as cardiovascular disease, which is an umbrella term used for all types of diseases that affect the heart or blood vessels. Cardiovascular disease is a leading cause of death in the United States.
Getting The Right Treatment For An Ra Skin Rash
Who do you call when your skin flares? For people with psoriatic arthritis, considering skin and joint problems in tandem makes so much sense that more than two dozen combined dermatology/rheumatology clinics have been established.
For RA, the director of the combined Center for Skin and Related Musculoskeletal Diseases at Brigham and Womens Hospital in Boston suggests contacting your rheumatologist.
Starting with the rheumatologist who is treating your joint disease and prescribing your arthritis medication would be a good first step. They can decide if a dermatology referral is appropriate, says Joseph F. Merola, MD, who is also an associate professor of dermatology at Harvard Medical School.
If you can, snap a picture of the problem area on your phone and bring it to your appointment.
I would still want to examine you in person, but it can be very helpful for me to see a picture of how the rash looked early on, says Dr. Deane.
Accurately diagnosing a skin problem sometimes requires a skin biopsy, blood tests, or allergy tests in addition to a physical examination. Once your doctor has pinpointed the problem, the answer may be a specific skin remedy or adjusting your arthritis regimen.
Can You Get A Rash With Rheumatoid Arthritis
Statistics indicate that about 1.3 million people in the United States have RA, and it affects about 1% of the worlds population. However, only a few who get RA will develop skin disease.
RA can cause a skin disease in a variety of ways. Some are relatively common, while others are rare. Not all skin manifestations are rashes.
Most commonly, skin manifestation will present as rheumatoid nodules. This is not a rash but hard lumps that form directly under the skin. They range from about the size of a pea to that of a golf ball.
These may develop over bony or fleshy areas of a persons body, such as elbows, hands, or fingers. About 40% of people with RA will have rheumatoid nodules.
Read on to learn more about RA-related skin rashes.
Recommended Reading: Can You Have Arthritis In Your Feet
Rheumatoid Arthritis And Skin Vasculitis
Rheumatoid arthritis can also cause inflammation of the blood vessels, known as vasculitis. Most often, small blood vessels are involved, notably those that supply blood to the skin on the fingertips. This usually looks like a blue or purplish rash near the fingernails, Dr. Tehrani says.
More serious forms of vasculitis can occur in larger blood vessels, such as those in the legs, and cause painful rashes or ulcers. If left untreated, these ulcers can become infected, so see a doctor immediately if you suspect an issue.
Also Check: Tomatoes Bad For Arthritis
Stage : Symptoms Are Visible
In this latter, more severe stage, blood tests and imaging are less relevant for diagnosis because you can actually see the effects of the disease. The joints start becoming bent and deformed, the fingers become crooked, Dr. Bhatt says. These misshapen joints can press on the nerves and can cause nerve pain as well, he says. In the older days we used to see more deformed joints when we did not have much treatment, but now we are seeing less and less, Dr. Bhatt says.
Recommended Reading: Can Arthritis Cause Numbness In Feet
What Causes Rheumatoid Vasculitis
Rheumatoid vasculitis may be linked to an increased immune response due to Rheumatoid Arthritis. The underlying cause of this is unknown. Most likely uncontrolled Rheumatoid Arthritis genetics, infection, or Smoking are underlying causes.
Vasculitis Foundation believes antibodies in RAs blood may cause the risk.
Smoking Stress It is unknown what causes some rheumatoid arthritis patients to develop rheumatoid vasculitis.
Risk Factors
Initiating factors increased risk of a person will develop the disease. Such infection: bacteria in the gut or mouth and gums infection are risk factors.
Risk factors that may increase the chances a person with RA will develop RV include:
Chronic, severe RA for ten years or more
Smoking,
High concentrations of rheumatoid factor antibodies and specific other proteins in the blood, such as Feltys syndrome, are a complication of RA.
Other Types Of Arthritis
Another less common type of arthritis is called gout. Gout occurs due to a high uric acid concentration in your blood, which forms sharp urate crystals in your joints. These crystals cause the intense sensations of pain, swelling, and tenderness characteristic of a gout attack. These attacks are frequently sudden and often occur in the big toe.
There are also many other types of arthritis. Additional types with a brief description are listed below:
Recommended Reading: Is Hot Or Cold Better For Arthritis
What Causes Rheumatoid Arthritis Rashes
People with RA are prone to episodes known as flares. A flare indicates that theres increased disease activity in a persons body.
During a flare, they may have more symptoms associated with the condition, including fever, joint swelling, and fatigue. An RA rash is more likely to occur during a flare.
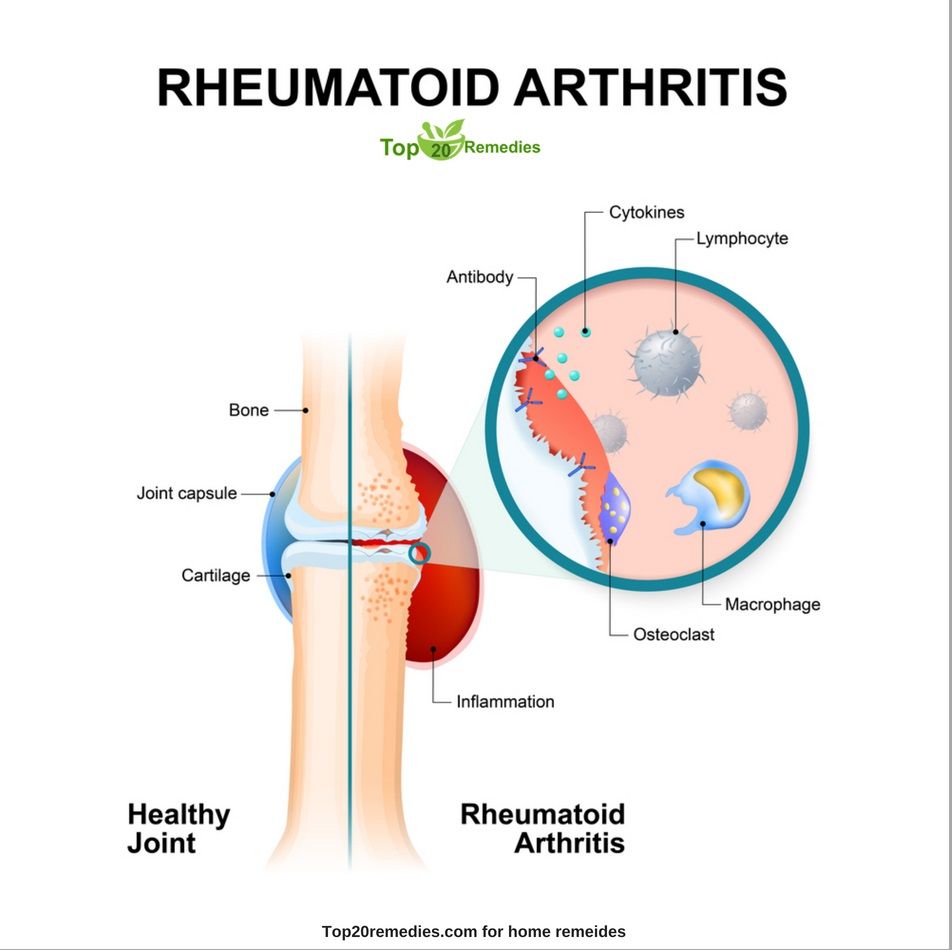
RV is a complication of RA. Its caused by the immune system and high levels of rheumatoid factor in the blood interacting with blood vessels.
This triggers inflammation of small arteries and veins. It can be serious and, while rare, RV
RA can cause complications beyond a rash. Vasculitis can affect blood flow in arteries and veins. The results of severe episodes of vasculitis can be:
- numbness and tingling in the nerves, including loss of sensation in the hands and feet
- affected blood flow to the extremities that can cause gangrene in the fingers or toes
- systemic vasculitis that affects blood flow to the brain or heart that can result in a heart attack or stroke
The occurrence of RV is rare, and the complications above are even rarer. However, its possible that a rash could be a indicate that something more severe may occur. See a doctor if you experience any symptoms of RV.
What Is The Treatment For Rheumatoid Arthritis Rashes
The treatment for an RA-related rash depends on its cause and severity. A treatment that works well for one type of rash may be useless for another.
Treatment usually focuses on managing pain and discomfort and preventing an infection. Its also important that treatments target the underlying condition, since rashes may be a sign that your RA isnt well controlled.
Common over-the-counter medications that may reduce the pain of a rash include acetaminophen . Dont take nonsteroidal anti-inflammatory drugs for RA rashes, as these can be organ threatening.
Drugs to avoid can include:
- naproxen sodium
If your pain is severe, a doctor may also consider prescription pain relievers. Opioid pain drugs are usually only prescribed for very severe pain since they have a high risk of addiction.
A doctor may also prescribe corticosteroids to reduce the inflammation of your rash, which may in turn reduce painful symptoms.
But these drugs arent recommended for long-term use. If the doctor is concerned that your rash could get infected, theyre likely to prescribe either a topical or oral antibiotic or both.
When it comes to treating the underlying condition, there are several different medication options available:
Read Also: What Helps With Arthritis In The Back
How Are Rheumatic Skin Conditions Treated
The answer to this question is complex. The skin lesions in a large number of the 100 or so diseases that cause arthritis are treated differently. For example, in a disease like lupus, the skin lesions can be treated quite nicely with cortisone-containing creams and oral medications such as the antimalarials. However, these same forms of treatment usually do not help the skin changes that we see in scleroderma.
The treatment really has to be individualized to the specific disease and to the specific conditions related to a given case. Some drugs might be riskier in women compared to men, for example.
Some drugs like the corticosteroids suppress the immune response in a broad fashion and can be very useful in a number of autoimmune diseases, including the rheumatic diseases . Corticosteroids like prednisone taken by mouth can certainly suppress various manifestations of rheumatoid arthritis, including the skin changes like vasculitis.
However, long-term use of corticosteroids by mouth can produce a lot of troublesome and serious side effects. Therefore, physicians are constantly trying to find other drugs that will prevent having to rely on corticosteroids for long periods of time.
Living With Rheumatoid Arthritis Rash
The addition of a skin rash while dealing with other symptoms of rheumatoid arthritis is not easy, but rest assured, theres hope. If you struggle with RA skin rashes or related symptoms, reach out to your rheumatologist, who can help you determine the cause and work on an effective treatment. Your physician can also connect you with other specialists so you can feel better and live your best lifehopefully, rash-free.
Recommended Reading: How Can I Relieve Arthritis Pain
What Actually Is Hives
Also called as urticaria, it is a skin reaction that leads to itchy nettle rash. It can range in size from tinny spots to large blotches as large as your hand . It may appear suddenly on a small area of the skin or affect across large areas, depending on the severity of the problem.
The symptoms of itchy nettle rash associated with hives include:
The risk factors, conditions /factors that increase your risk of developing hives, are as follows:
Hives is common, and having some of risk factors mentioned above can put you at higher risk than others.
It can be acute or chronic. Acute or short-term hives can affect about 1 out of 5 people at some point in their lives. Chronic or long-term hives is less common, but it is more difficult to treat.
Causes
Some people have hives when a trigger leads to high levels of histamine and other certain chemicals in the skin.
Tips For Managing Skin

One of the first things you can do is contact your rheumatologist if you notice new or worsening skin problems. They can help determine if the issues are related to your RA or treatment. You may also want to work with a dermatologist or other specialist.
In addition to a doctors care, you can try to take some additional steps to help protect your skin. These might include:
- quitting smoking
- using moisturizers to keep the skin moist
- getting the shingles vaccine
Don’t Miss: What Can I Use For Arthritis Pain
Treatment Of Skin Issues
Some skin issues may require treatments, while others might not. Treatment will depend on the cause and severity. The goal of treatment is to reduce pain, discomfort, and inflammation, and also to prevent infection.
It is very important to treat the underlying cause of skin problems, as these conditions are a sign that rheumatoid arthritis symptoms are not well-managed.
Common over-the-counter medications, including acetaminophen , can help with pain, while NSAIDs, including ibuprofen, can help control and reduce inflammation. Severe pain may need prescription NSAIDs. Corticosteroids can also help reduce skin inflammation, but these medications cannot be used in the long-term. If there is a possibility of infection, a topical or oral antibiotic may be prescribed. Hives are usually treated with antihistamines.
If medications are the cause of RA skin symptoms, medication replacement or reduction may help prevent or reduce skin symptoms.
Can A Blood Test Detect Psoriatic Arthritis
There is no single blood test that can check for psoriatic arthritis , a chronic, inflammatory disease of the joints that can also cause a skin disorder called psoriasis. Your doctor will order a series of blood tests to check for different signs of psoriatic arthritis.
Do you always have a rash with psoriatic arthritis? About 85 to 95 percent of psoriatic arthritis patients develop the rash of psoriasis before they develop psoriatic arthritis, but some people develop joint pain before the rash, or they both come at the same time, says Rebecca Haberman, MD, Clinical Instructor of Rheumatology at NYU Langone Health in New York City.
What do autoimmune rashes look like?
Autoimmune rashes can look like scaly red patches, purplish bumps, or more. The appearance of autoimmune rashes will be different, depending on which autoimmune condition is triggering the skin rash. For example, cutaneous lupus may cause a scaly red patch that does not hurt or itch.
What does butterfly rash look like? The rash is red or purple and may be either blotchy or solid in appearance. It is commonly known as a butterfly rash due to its distinctive butterfly shape. A malar rash may be flat or slightly raised, and it can feel rough and scaly. It may be itchy and, in severe cases, it may be painful.
Read Also: Are Bing Cherries Good For Arthritis
What Is Butterfly Rash
Malar rash, also named a butterfly rash, is a common facial presentation of multiple disorders. It is characterized by an erythematous flat or raised rash across the bridge of the nose and cheeks, which usually spares nasolabial folds. It may be transient or progress to involve other areas of facial skin.
Join our Advertising Community and share you ideas today !
Soreness In Your Ankles And Feet
RA can cause problems in the ankle and foot, including pain, sore joints, redness, swelling and inflammation, or warmth. Treatments may involve medications known as DMARDs, physical therapy, different footwear, braces, orthotics, or surgery. Some of the foot issues that can be caused by RA include bunions, hammertoe, bursitis, Charcot arthropathy, plantar fasciitis, rheumatoid nodules, and heel pain.
RELATED: Treating Rheumatoid Arthritis With Disease Modifying Therapies
Don’t Miss: Why Are Rheumatoid Arthritis Drugs So Expensive
Who Can Diagnose And Treat Psoriatic Arthritis
If you have painful, swollen joints and other symptoms, start with your primary care doctor, says Dr. Parody. They may refer you to a rheumatologist, who specializes in diagnosing and treating arthritis and other diseases that affect the joints, muscles and bones.
Some psoriatic arthritis treatments will also help calm skin symptoms. But if you have bothersome psoriasis symptoms, it can be helpful to see a dermatologist, too .
How Seasonal Allergies Impact Chronic Illness
Seasonal allergies are uncomfortable and can cause or aggravate other health problems.
When my seasonal allergies strike in the Spring, I feel it in my joints and in my gut, says patient advocate Zoe Rothblatt, who lives with spondyloarthritis and Crohns disease. Along with the sniffles and congestion headache, my joints get a fiery ache and I get a crampy ache in my gut.
Read Also: What Is Arthritis Of The Spine
Allover Weakness Or Fatigue
What doctors call anemia of inflammation and chronic disease shouldnt be confused with iron-deficiency anemia, the most common form of this condition. AI/ACD is the second most common form of anemia and, as the name suggests, its associated with chronic diseases, inflammatory disorders like RA, lupus, and cancer.
In both AI/ACD and iron-deficiency anemia, there are low levels of iron circulating in the blood. In AI/ACD, however, blood iron levels are low even though stored iron levels are normal or high, according to the National Institutes of Health. This occurs because inflammatory conditions like RA interfere with the way the body uses stored iron and iron from diet.
Common signs of AI/ACD include weakness, fatigue, pale skin, fast heartbeat and shortness of breath. Your doctor can order a complete blood count to determine whether you have AI/ACD. Typically, doctors will focus on treating the chronic illness thats causing AI/ACD. For people with AI/ACD caused by RA, anti-inflammatories may be prescribed.
How To Treat Rheumatoid Nodules
Specific treatment for rheumatoid nodules isnt generally advised. This is because most nodules are only unsightly as opposed to debilitating, and therefore are not aggressively treated. However, if nodules cause the skin to become infected or ulcerated, then treatment will be necessary.
Nodules that form on the heels or beneath the feet can be debilitating to the patient limiting their mobility. In these cases, treatment would not just be advised but likely necessary.
Certain disease-modifying antirheumatic drugs have been known to reduce the appearance of rheumatoid nodules. Other treatments like steroid injections can also help to decrease the size of rheumatoid nodules.
Some patients report that even after treatment or having their rheumatoid nodules removed, they do grow back. Unfortunately, the nature of rheumatoid arthritis and its symptoms mean that the nodules can recur after treatment.
With this in mind, it is important to have a discussion with your physician about your symptoms, and the available treatment options that can help reduce the size of rheumatoid nodules or even remove them.
You May Like: Can You Put Heat On Arthritis