Types Of Psoriatic Arthritis
Its helpful to understand what type of psoriatic arthritis you are diagnosed with to recognize how it can affect the way you feel in your day-to-day life. These are the five types of psoriatic arthritis:
- Distal interphalangeal predominant Ps.A. primarily involves the small joints of the hands and feet that are closest to the nails, so you may have a hard time with movements that involve those joints, like opening jars or even just standing to cook.
- Asymmetric oligoarthritis affects less than five small or large joints and can involve joints on both sides of the body. For example, you might have pain in your right wrist and in your left knee.
- Symmetric polyarthritis affects the same joint on both sides of the body. So you might feel pain in both knees or both wrists, for example.
- Spondyloarthritis happens when inflammation develops between the vertebrae of your spine and causes neck pain and mobility problems.
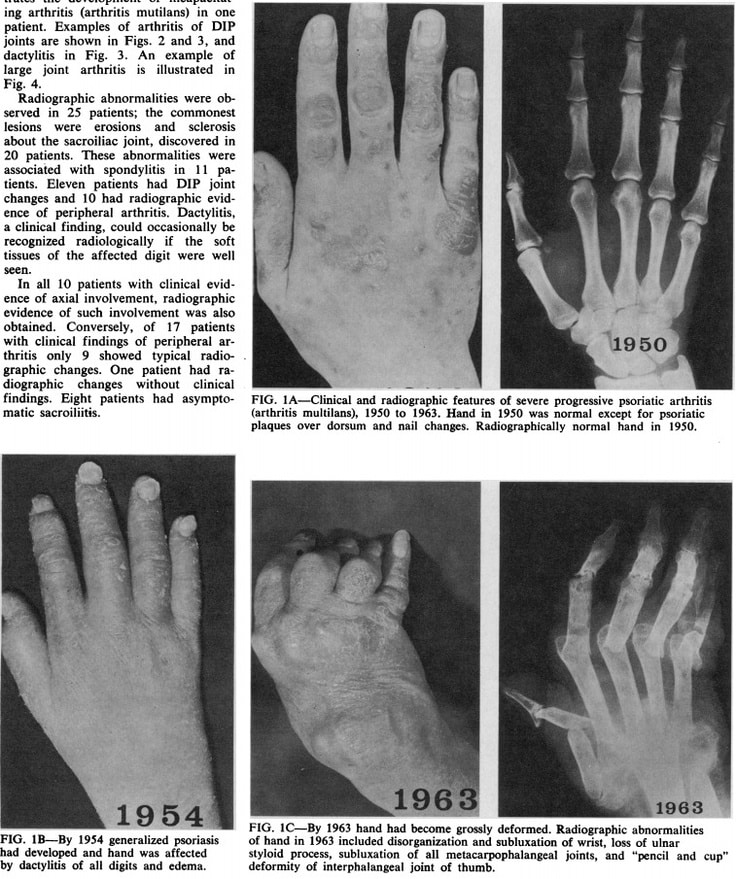
- Arthritis mutilans is a rare form of psoriatic arthritis that can severely damage your feet and make it hard to move or straighten your fingers or toes.
Myth: Having Psoriasis Automatically Means Youll Get Psa
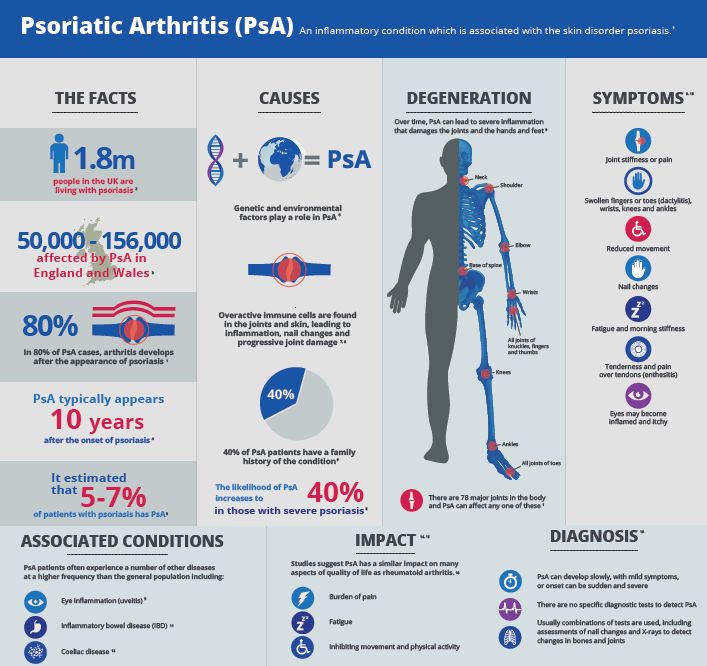
Fact: About 30% of people with psoriasis develop PsA.
Not everyone with psoriasis will get PsA. In fact, PsA only affects about 30% of people with psoriasis. This means that the majority of people with psoriasis wont get PsA. Its possible for some people with psoriasis to develop another type of arthritis, such as rheumatoid arthritis.
Its important to consider the incidence of autoimmune diseases in your family. Though theres no single identifiable cause of PsA, genetic predisposition seems to have a role. About
Fact: PsA can cause flare-ups, along with periods of remission.
PsA is a chronic condition, which means a person will have it for life.
Having a flare-up with joint pain and skin symptoms is common with this disease. If your case is mild, you may also have remission periods in which you dont notice any symptoms at all.
However, a lack of symptoms merely means that your immune system is dormant in its attacks on cells and tissues. This doesnt mean that its not PsA or that the PsA has suddenly disappeared.
The only way to be sure about the state of your PsA is to get a diagnosis from a rheumatologist. Avoid relying on symptoms alone as a method of self-diagnosis.
What Causes Psoriatic Arthritis
The genes you inherit from your parents and grandparents can make you more likely to develop psoriatic arthritis. If you have genes that put you at risk of this condition, the following may then trigger it:
- being overweight
There is also an element of chance, and it might not be possible to say for certain what caused your condition.
Psoriasis and psoriatic arthritis are not contagious, so people cant catch it from one another.
Don’t Miss: Are Oranges Good For Arthritis
How Psoriasis Affects Your Immune System
Your bodyâs immune system is supposed to protect you from diseases. When itâs working the way it should, immune cells identify and attack invaders like bacteria and viruses. But when you have an autoimmune disease, cells in your immune system go haywire.
With psoriasis, your T cells become highly active and attack skin cells by mistake. Then other parts of your immune system spring into action. Inflammation happens, and skin cells grow too fast.
Whatâs âtoo fastâ? In healthy people, new skin cells normally travel from deep within the skin to the surface of the skin in about a month. The process is called cell turnover. With psoriasis, new skin cells rise to the surface within days. The rapid cell turnover leads to thick patches of skin.
Pregnancy Fertility And Breastfeeding
Psoriatic arthritis wont affect your chances of having children. But if youre thinking of starting a family, its important to discuss your drug treatment with a doctor well in advance. If you become pregnant unexpectedly, talk to your rheumatology department as soon as possible.
The following treatments must be avoided when trying to start a family, during pregnancy and when breastfeeding:
- retinoid tablets and creams.
Theres growing evidence that some other drugs for psoriatic arthritis are safe to take during pregnancy. Your rheumatology department will be able to tell you which ones.
It will help if you try for a baby when your arthritis is under control.
Its also important that your arthritis is kept under control as much as possible during pregnancy. A flare-up of your arthritis during pregnancy can be harmful for you and your baby.
Psoriasis and psoriatic arthritis can run in families. If you have either condition, you could pass on genes that may increase your childrens risk though its difficult to predict.
As treatments continue to improve, people with psoriatic arthritis in years to come can expect a better outlook. If you have any questions or concerns, talk to your doctor.
Don’t Miss: Is Massage Good For Arthritis In The Neck
Who Will Be Responsible For My Healthcare
Youre likely to see a team of healthcare professionals.
Your doctor, usually a rheumatologist, will be responsible for your overall care. And a specialist nurse may help monitor your condition and treatments. A skin specialist called a dermatologist may be responsible for the treatment of your psoriasis.
You may also see:
- A physiotherapist, who can advise on exercises to help maintain your mobility.
- An occupational therapist, who can help you protect your joints, for example, by using splints for the wrist or knee braces. You may be advised to change the way you do some tasks to reduce the strain on your joints.
- A podiatrist, who can assess your footcare needs and offer advice onspecial insoles and good supportive footwear.
Types Of Rheumatoid Arthritis
The two types of rheumatoid arthritis are seropositive RA and seronegative RA, as follows:
- Seropositive RA, known as RA, indicates that a person with RA has positive blood results for anti-CCP and rheumatoid factor along with all the signs and symptoms of the disease.
- Seronegative RA is called seronegative because of the negative results of these antibody blood tests that are typically done when healthcare providers diagnose RA.
Also Check: Why Does Psoriasis Cause Arthritis
Treatments For Your Skin
If your psoriasis is affecting your quality of life, or your treatment is not working, you may be referred to a dermatologist.
There are a number of treatment options for psoriasis.
Ointments, creams, and gels that can be applied to the skin include:
- ointments made from a medicine called dithranol
- steroid-based creams and lotions
- vitamin D-like ointments such ascalcipotriol and tacalcitol
- vitamin A-like gels such astazarotene
- tar-based ointments.
For more information about the benefits and disadvantages of any of these talk to your GP, dermatologist, or pharmacist.
If the creams and ointments dont help, your doctor may suggest light therapy, also known as phototherapy. This involves being exposed to short spells of strong ultraviolet light in hospital.
Once this treatment has started, youll need to have it regularly and stick to the appointments youve been given, for it to be successful. This treatment is not suitable for people at high risk of skin cancer or for children. For some people, this treatment can make their psoriasis worse.
Retinoid tablets, such as acitretin, are made from substances related to vitamin A. These can be useful if your psoriasis isnt responding to other treatments. However, they can cause dry skin and you may not be able to take them if you have diabetes.
Some DMARDs used for psoriatic arthritis will also help with psoriasis.
Do You Need To Modify Psoriatic Arthritis Medications Before Or After Getting The Vaccine
Temporarily stopping certain immunosuppressant medications after receiving the vaccine, or timing when you get the vaccine in the course of your treatment, might help increase the effectiveness of the COVID-19 vaccine if you have PsA.
But this only applies to a select few psoriatic arthritis medications. It is recommended, in most cases, that PsA patients who are to receive a COVID-19 vaccine continue their biologic or oral therapies for psoriatic arthritis, says Dr. Gupta.
The American College of Rheumatology and National Psoriasis Foundation guidance differs on this matter, which is why its important to discuss this with your doctor and make a decision thats right for your situation.
Here are the psoriatic arthritis drugs for which the ACR guidance suggests changes may be recommended:
- Methotrexate: Skip for 1 week after each vaccine dose
- JAK inhibitor : Skip for 1 week after each vaccine dose
- Abatacept , injectable form: Skip one week before and after the first vaccine dose only
- Abatacept , IV form: Get COVID-19 vaccine 4 weeks after your last infusion, then skip a week and get next infusion
The NPF guidance recommends that patients continue their biologic or oral therapies for psoriatic arthritis in most cases. For the Johnson & Johnson COVID-19 vaccine, which is only one dose, the guidance says that certain patients can consider holding methotrexate for two weeks after getting the vaccine:
Also Check: How Do You Fix Arthritis In The Knee
What Are The Treatment Options For Psoriatic Arthritis
The aim of treatment for psoriatic arthritis is to control the disease and relieve symptoms. Treatment may include any combination of the following:
Choice of medications depends on disease severity, number of joints involved, and associated skin symptoms. During the early stages of the disease, mild inflammation may respond to nonsteroidal anti-inflammatory drugs . Cortisone injections may be used to treat ongoing inflammation in a single joint. Oral steroids, if used to treat a psoriatic arthritis flare, can temporarily worsen psoriasis. Long-term use of oral steroids should be avoided when possible due to the negative effects on the body over time.
DMARDs are used when NSAIDs fail to work and for patients with persistent and/or erosive disease. DMARDs that are effective in treating psoriatic arthritis include: methotrexate, sulfasalazine, and cyclosporine.
Biologic agents are an important consideration when disease control is not being achieved with NSAIDS or DMARDs. Biologics have been utilized for the treatment of psoriatic arthritis since 2005 and are highly effective at slowing and preventing progression of joint damage. Your healthcare provider will complete additional laboratory tests and review safety considerations before initiating a medication regimen. Gaining good control of psoriatic arthritis and psoriasis is important to avoid increased systemic risks, particularly heart disease.
Exercise
Heat and cold therapy
Joint protection and energy conservation
Digestive Disorders And Psoriatic Arthritis
Did you know having psoriatic arthritis might also affect your gut?
A study published in Clinical Rheumatology found people with psoriatic arthritis are at risk for having the following conditions:
- Crohns disease, a chronic inflammatory bowel disease that affects the lining of the digestive tract
- Ulcerative colitis, a chronic inflammatory bowel disease that causes inflammation in the digestive tract
- Reflux esophagitis, a condition where inflammation damages the esophagus
- Peptic ulcer disease, a condition that causes painful sores or ulcers in the lining of the stomach or small intestine
Another study, published in JAMA Dermatology, revealed people with psoriasis were around 2 times more likely to develop Crohns and ulcerative colitis compared with the general population.
The authors concluded: These findings suggest that psoriasis is significantly associated with IBD. Gastroenterology consultation may be indicated when patients with psoriasis present with bowel symptoms.
Scientists believe that the same gene mutations that are associated with psoriasis may also be related to the gut disorders.
You May Like: Is Ibuprofen Safe For Dogs With Arthritis
Myth: Most Psa Cases Are The Same
Fact: There are five subtypes of PsA.
PsA is currently diagnosed as one of five subtypes. These are based on the severity of the condition, as well as the location of the affected joints. As the disease progresses, patients may be diagnosed from one subtype to another.
The five subtypes include:
- Oligoarticular: affects one to four joints asymmetrically
- Symmetric: affects the same joints on both sides of the body
- Spondylitis: PsA of the spine
- Distal interphalangeal: primarily affects finger and toe joints and can also cause nail deformities)
- Arthritis mutilans: a rare form of PsA that mainly causes severe destruction in feet and hand joints
Psoriatic Disease: An Autoimmune Disease Experts View
Psoriatic disease is a condition you have your whole life. Skin plaques are the main symptom, but many people also get joint pain. It requires lifelong observation by medical professionals. Although there isnât a cure for psoriatic disease, there are great medications to help control the symptoms.
The news that you have it can sometimes come as a surprise. You may see your primary care doctor because youâre having joint pain, but be unaware of plaques because theyâre hiding on your backside, scalp, chest, or groin.
If your psoriasis is mild enough, a primary care doctor should be able to prescribe topical steroids or other topical medications to help, depending on how much of your body is involved.
But many people with psoriasis require more than just topical therapies, especially if they have joint pain and swelling. If your psoriasis care goes beyond the scope of a primary care doctor, youâll need to see other specialists to get the treatment you need.
Recommended Reading: What Is The Most Effective Medication For Arthritis
Effects On The Digestive System
There is a link between inflammatory bowel disease , such as Crohns disease, and PsA because inflammation underlies both conditions. IBD causes diarrhea and other gastrointestinal symptoms.
People with PsA have a significantly increased risk of developing IBD, according to research from 2017. Other studies suggest that psoriasis is eight times more common in people with Crohns disease.
Genetic And Epigenetic Findings Of Autoimmunity In Psa
2.1.1. Human leukocyte antigen associations
Given their strong risk association, explaining the functional role of the HLA risk alleles, particularly the HLA-C*06:02, is essential for elucidating the pathogenesis of PsA. A fascinating case study with a unique methodology identified ADAMTS-like 5 as an HLA-C*06:02-presented melanocytic autoantigen to the lesion-infiltrating autoreactive CD8+ T cells in psoriasis . More interestingly, peptide motifs of the HLA-C*07:01, -C*07:02, and -B*27, which are three of the other psoriasis risk-related leukocyte antigens, utilize the same anchor residues with the HLA-C*06:02, have overlapping peptide-binding properties, and belong to the same HLA supertype . Synovial/entheseal counterpart of this picture is yet to be studied but seems to be more complicated since different disease phenotypes in PsA exhibit different HLA associations and contribution of the HLA-C*06:02 polymorphism to PsA risk is lesser compared to psoriasis .
Read Also: What Helps Arthritis Pain In Ankle
Risk Factors And Prevalence
Psoriasis, a family history of PsA, being between 30 and 50 years of age, cigarette smoking, obesity, having the HLA-B gene and other genetic markers, being male, and environmental triggers .
Dykes, L. . Females at Greater Risk of Developing Psoriatic Arthritis in Recent Years. Rheumatology Network. .
Feintuch, S. . 11 Psoriatic Arthritis Complications You Need to Know About. CreakyJoints. .
Feintuch, S. . Psoriatic Arthritis Risk Factors and Causes You Need to Know About. CreakyJoints. .
Haddad, A., & Zisman, D. . Comorbidities in Patients with Psoriatic Arthritis. Rambam Maimonides medical journal, 8, e0004. .
Jaw Pain And Psoriatic Arthritis
Psoriatic arthritis can affect any joint, including the temporomandibular joint that connects the jawbone to the skull. The TMJ is linked to the masseter the strongest muscle in your body based on its weight. Because it works so hard, the TMJ is at risk for damage.
About 35 percent of people with psoriatic arthritis will have symptoms in their TMJ, according to the National Psoriasis Foundation.
Rheumatologists are encouraged to perform a 66-68 joint count, which essentially measures swelling in 66 joints and tenderness and pain in 68 joints. Still, doctors often miss signs of TMJ damage.
In clinical practice, rheumatologists arent necessarily used to looking at the TMJ. They are part of the 66-68 joint count, which was endorsed as a mandatory measure for clinical trials and longitudinal studies, Ana-Maria Orbai, MD, an assistant professor of rheumatology at Johns Hopkins University in Baltimore, and an NPF medical board member, told the National Psoriasis Foundation. But most people in practice will just look at patients hands. Because practitioners arent doing the full joint count, they may miss the TMJ.
Treatment options, such as biologics and disease-modifying anti-rheumatic drugs , can help prevent or slow TMJ damage. Additionally, you should try to avoid chewing hard foods to reduce pressure on your jaw.
Read Also: How To Get Rid Of Arthritis In Neck
Five Clinical Presentations Of Psoriatic Arthritis
Diagnosis of psoriatic arthritis may often be delayed since there are no identified biomarkers at this time. If left untreated psoriatic arthritis may lead to severe physical limitations and disability. Early diagnosis is critical to slow the progression of the disease with medications.
Coexisting Diseases And Conditions
Cardiovascular disease, obesity and metabolic syndrome, diabetes, osteoporosis, malignancy, fatty liver disease, depression, anxiety, vision problems, skin cancer, inflammatory bowel disease, arthritis mutilans, gout, HIV.
Recent research shows that inflammatory bowel disease may lead to the development of psoriatic arthritis.
Don’t Miss: Could I Have Arthritis In My Knee