Rheumatoid Factor And Anti
One blood test measures levels of rheumatoid factors in the blood. Rheumatoid factors are proteins that the immune system produces when it attacks health tissue.
About half of all people with rheumatoid arthritis have high levels of rheumatoid factors in their blood when the disease starts, but about 1 in 20 people without rheumatoid arthritis also test positive.
A related blood test known as anti-cyclic citrullinated peptide test is also available. Anti-CCPs are antibodies also produced by the immune system.
People who test positive for anti-CCP are very likely to develop rheumatoid arthritis, but not everybody with rheumatoid arthritis has this antibody.
Those who test positive for both rheumatoid factor and anti-CCP may be more likely to have severe rheumatoid arthritis requiring higher levels of treatment.
Learning When You’re Stiff
RA-related stiffness is usually worst in the morning and lasts about an hour, Dr. Khan says: The fingers are tight. They have a hard time movingthey feel like the Tin Manand then as they get moving, in half an hour to an hour, symptoms get better. Any extended period of sitting or just not moving can cause RA joints to stiffen up, too. Osteoarthritis stiffness typically happens for less time later in the day, after physical activity.
How Common Is Ra Back Pain
When back pain is RA related, inflammation in the cervical spine is usually the cause.
RA primarily affects peripheral jointssuch as in the hands, feet, and kneesbut the cervical spine is the second most common region thatâs affected.
The spine is affected when RA progresses. In other words, inflammation in the back and spine may indicate a more advanced disease. However, the damage can be seen on X-rays as early as two years after diagnosis.
A 2015 report suggests that more than 80% of people with RA have some cervical spine involvement.
Although pain in the lumbar spine, or low back, is not commonly a part of RA, itâs associated with RA. This means that if you have RA, itâs common to also have low back pain.
A 2013 study reported that up to 65.5% of people with RA may experience low back pain. The researchers also noted that people with RA who had low back pain reported lower quality of life and had an increased risk for depression.
A 2017 report in the German medical journal Zeitschrift für Rheumatologie also found that low back pain in those with RA led to a higher degree of disability.
Recommended Reading: Can You Have Ra And Psoriatic Arthritis
How Does Rheumatoid Arthritis Affect How People See Themselves
Rheumatoid arthritis is relatively common in young women. The limitations it can cause come right at a time when most of their peers are in good health, and that can be hard to deal with.
Some women worry that they cant be a good mother or partner. Young women who have rheumatoid arthritis often wonder whether they should even have children. Having this disease doesnt mean that getting pregnant isnt an option. But its important to keep in mind that not all of the rheumatoid arthritis medication can be taken before and during pregnancy or while breastfeeding. You can talk to a rheumatologist or gynecologist about this early on. Men who are trying for a baby with their partner also need to stop taking certain rheumatoid arthritis medications for a while.
Some people are concerned about loss of status if they have to give up their job or take on a different position. The pain and loss of strength can also affect how you see yourself. It can be hard to show weakness or accept help, especially for men. Quite a few people even try ignoring the condition as much as possible because it doesnt fit in with how they view themselves. Theyd like to stay in control and continue living the life theyre used to as much as possible. This can be physically and emotionally draining, though. It can sometimes lead to depressive thoughts, frustration and aggression.
Also Check: Does Arthritis Make Your Hands Shake
Living With Rheumatoid Arthritis
Research shows that people who take part in their own care report less pain and make fewer doctor visits. They also enjoy a better quality of life.
Self-care can help you play a role in managing your RA and improving your health. You can:
- Learn about rheumatoid arthritis and its treatments.
- Use exercises and relaxation techniques to reduce your pain and help you stay active.
- Communicate well with your health care team so you can have more control over your disease.
- Reach out for support to help cope with the physical emotional, and mental effects of rheumatoid arthritis.
Participating in your care can help build confidence in your ability to perform day-to-day activities, allowing you to lead a full, active, and independent life.
Also Check: Can Psoriatic Arthritis Cause Hip Pain
What Are The Risk Factors For Developing Rheumatoid Arthritis
There are several risk factors for developing rheumatoid arthritis. These include:
- Family history: Youre more likely to develop RA if you have a close relative who also has it.
- Sex: Women and people designated female at birth are two to three times more likely to develop rheumatoid arthritis.
- Smoking:Smoking increases a persons risk of rheumatoid arthritis and makes the disease worse.
- Obesity: Your chances of developing RA are higher if you have obesity.
Why You Have Arthritis
There are over 100 different types ofarthritis that can develop as you get older or following an injury. The many types of arthritis target your joints, causing pain, inflammation, and stiffness and limiting your joints flexibility.
The two most common types of arthritis that affect many adults in the United States include osteoarthritis and rheumatoid arthritis.
Read Also: Whats Good For Arthritis In The Legs
Also Check: Can I Take Tylenol Arthritis With Xarelto
Making A Diagnosis Of Rheumatoid Arthritis
Diagnosis of RA is not straight forward as there is no individual test for RA. A diagnosis tends to be made by a consultant rheumatologist on the basis of tests, examination and ruling out other possible causes for symptoms.
Sometimes it is clear from symptoms and initial blood tests that someone has rheumatoid arthritis, but not always. Specialist criteria have been developed jointly by American and European experts to try to help make a diagnosis of rheumatoid arthritis in people presenting with new-onset swollen, painful joints with no obvious cause . These should be used with care though as people with osteoarthritis or a crystal arthritis could meet the criteria and end up being incorrectly diagnosed with rheumatoid arthritis, which could have significant consequences for treatment. They have also been developed to classify, not diagnose, rheumatoid arthritis and so should not be used to decide who gets referred.
As already mentioned above, there are a number of other conditions that can cause very similar symptoms to rheumatoid arthritis and your GP will have to consider these when assessing each case.
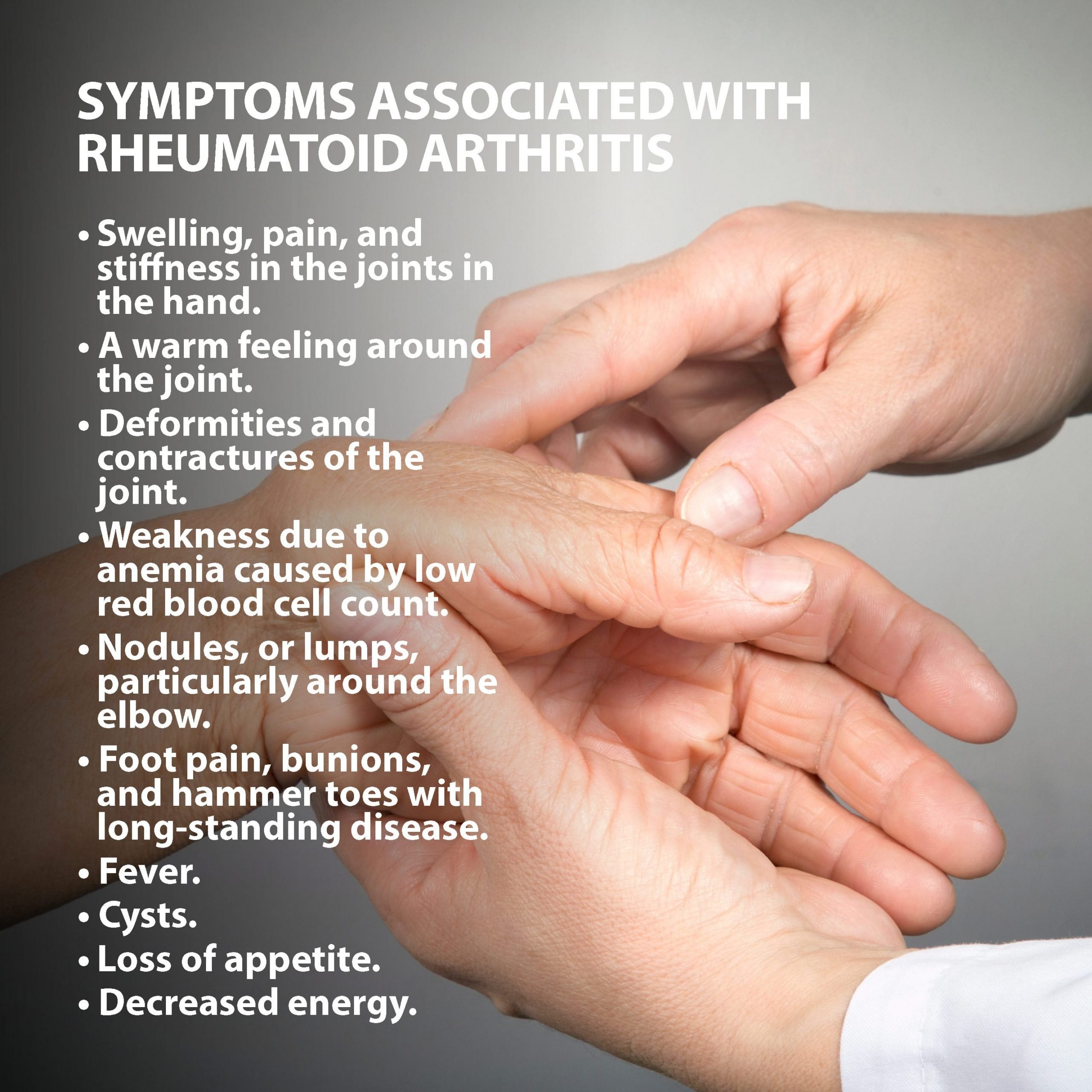
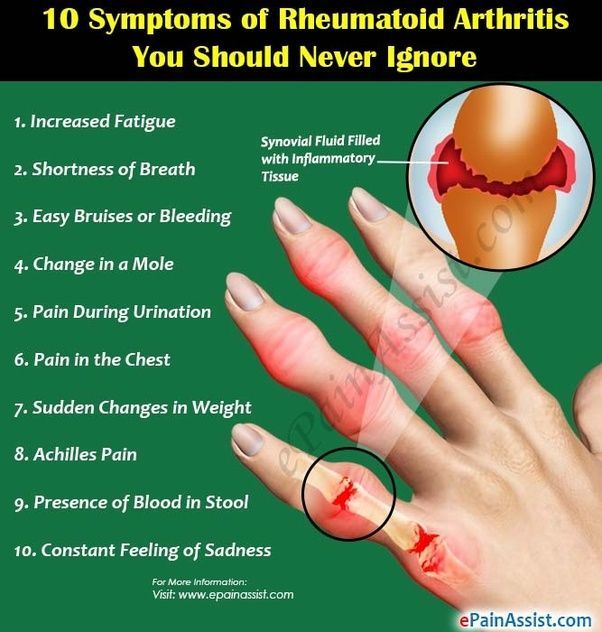
What Are The Signs And Symptoms Of Ra
With RA, there are times when symptoms get worse, known as flares, and times when symptoms get better, known as remission.
Signs and symptoms of RA include:
- Pain or aching in more than one joint
- Stiffness in more than one joint
- Tenderness and swelling in more than one joint
- The same symptoms on both sides of the body
Also Check: How Do You Cure Rheumatoid Arthritis
How To Prepare For An Initial Doctors Appointment
During your first appointment, your doctor will conduct a physical exam, collect details about your medical history, and discuss which symptoms you may be experiencing.
Generally, they will evaluate your joints for inflammation, swelling, and redness and may order imaging tests or blood work to determine if you have RA.
Be sure to keep track of all your symptoms and consider logging the time, duration, and severity of each symptom as it occurs. You should also provide your doctor with information about any medications that you are taking, including the frequency and dosage.
Keep in mind that you may not receive a definitive diagnosis on your first visit, as many autoimmune disorders develop slowly over time.
However, your doctor may discuss possible treatment options with you, which can include medications, physical therapy, pain management, exercise, and other modifications to your diet and lifestyle.
Its important to discuss any questions you have regarding your treatment plan with your doctor. Some questions you may want to consider asking:
- What treatment options are right for me?
- What are the potential side effects from my treatment?
- What types of exercise would be beneficial? How often should I work out?
- Are there other ways to treat symptoms at home, such as by using a hot or cold compress?
- What options available for mental health support, if needed?
- Would I benefit from physical therapy, nutrition counseling, or other complementary treatments?
What Conditions May Be Confused With Ra
Fibromyalgia
People with this condition often feel pain all over, in all their muscles and joints, and have multiple tender points when examined. They will also often have a degree of early morning stiffness. Poor unrestorative sleep is often present, with associated fatigue and low mood, and often there are associated symptoms of headaches and irritable bowels and bladder. Investigations tend to be normal. It is important to distinguish this condition from rheumatoid arthritis as their management is very different, although sometimes both conditions are present.
Polymyalgia Rheumatica
This condition causes pain and stiffness of the shoulders and thighs and tends to occur in people over 65 years of age. It is more common in females. Sometimes elderly people with RA present with similar symptoms. PMR is treated by a course of steroid tablets where the dosage is gradually reduced over months and can generally be stopped after about 18 months 2 years. In people with RA presenting with PMR type symptoms, the correct diagnosis of RA usually becomes apparent when the patient is unable to reduce the steroid dosage below 10mg.
Post-viral arthritis
Osteoarthritis
Crystal Arthritis
Other types of inflammatory arthritis
Recommended Reading: What To Take To Prevent Arthritis
How Else Can Your Gp Surgery Help
Your GP surgery can be involved in your RA care in many different ways. They continue to look after you in general and may want to keep a close eye on your blood pressure, cholesterol and blood glucose levels as there is a higher risk of heart disease in people affected by rheumatoid arthritis. This is often done as an annual review with one of the practice nurses. Many GP surgeries are involved in doing the blood monitoring for the specific drugs used in controlling and treating the joint inflammation , so you may get your regular blood tests performed by your surgery.
Rheumatoid arthritis, along with many of the treatments used affects the bodys immune response to infections. Your surgery may therefore contact you to offer you annual influenza jab and also a Pneumovax for pneumonia . With some of these treatments live vaccines should be avoided so please ensure you contact your Doctors surgery if you are planning to travel abroad.
What Else Could It Be
When a doctor thinks about how likely you are to have one disease over another, or over several others, this is called a differential diagnosis. There are many conditions your doctor may consider besides RA, and besides other forms of autoimmune arthritis:
Viral arthritis: Rubella, parvovirus, and hepatitis B and C can lead to short-term arthritis symptoms that resemble RA.
Palindromic rheumatism: Periodic joint inflammation that may lead to RA, lupus, and similar diseases
Polymyalgia rheumatica: This is more common over age 50, generally less painful than RA, and associated more with shoulders and hips.
Recommended Reading: How Do You Get Arthritis In The Knee
What Kind Of Information Will The Insurance Companies Ask Me Or Be Interested In
If youve been diagnosed with osteoarthritis or rheumatoid arthritis, the life insurance company may ask you a range of questions to better understand your health status and any potential risks.
Some of the information they may ask about includes:
- Date of diagnosis: The life insurance company may ask when you were diagnosed with osteoarthritis or rheumatoid arthritis and how severe your symptoms were at the time.
- Treatment: The life insurance company may ask about any treatments you have received for your arthritis, such as medication, physical therapy, or surgery. They may also ask about the effectiveness of these treatments and whether you have experienced any side effects or complications as a result of the condition.
- Current health status: The life insurance company may ask about your current health status, including any ongoing medical conditions, medications you are currently taking, and any other health issues you have experienced.
- Lifestyle: The life insurance company may ask about your lifestyle habits, such as your diet, exercise routine, and use of tobacco or alcohol, as these can all potentially impact your health.
Its important to be as honest and accurate as possible when answering these questions, as any discrepancies or omissions could affect the coverage provided by the policy.
Now at this point
We usually like to take a moment and remind folks that nobody here at IBUSA has any kind of medical training, and were certainly not doctors.
Reaching A Ra Diagnosis
Once all of these steps have been conducted, doctors will look at all of the test results and reach a conclusion based on the overall picture. Some doctors take a more symptom based approach to diagnosing RA while others rely on blood tests and medical history to confirm a RA diagnosis.
This is why its possible to be diagnosed with RA but not test positive for antibodies or have a medical history of RA in your family. If the symptoms themselves are consistent with RA, then it can still be diagnosed.
That being said, the main criteria for diagnosing RA do not change. The patient must exhibit symptoms for greater than six weeks, symmetrical symptoms, as well as multiple joints being affected including fingers and hands.
You May Like: How Bad Does Arthritis Have To Be To Get Disability
Can I Prevent Rheumatoid Arthritis
You cannot prevent rheumatoid arthritis because the cause of the disease is not known.
Quitting smoking, or never smoking, will reduce your risk of developing rheumatoid arthritis. You are more likely to develop rheumatoid arthritis if someone in your close family has it, but unfortunately there is no way to reduce this risk.
People who have rheumatoid arthritis often experience flare ups, which are times when their joints are particularly sore. Learning what triggers your flare ups can help reduce or prevent them.
For some people, stress can trigger a flare up, so can being run down or pushing yourself beyond your limits. Having an infection, missing a dose of your medicine or changing your treatment plan can also cause a flare up.
Keeping a food and activity diary may help work out your personal triggers but keep in mind that sometimes flare ups happen without any obvious cause.
Ra Onset In Older Adults
EORA occurs in individuals over the age of 65 years. Although early onset RA is more prominent in females, EORA has a more similar distribution between males and females.
Doctors often diagnose EORA earlier in the disease, and although it is frequently acute with symptoms coming on quickly, it is less erosive or damaging to the bones than early onset RA. Additionally, EORA often involves larger joints such as the shoulders rather than the small joints of the hands.
Among those with EORA, fewer individuals may test positive for rheumatoid factor , an immune system protein that may attack healthy tissues. Overall, 80% and 6070% of individuals with RA test positive for RF and cyclic citrullinated protein , respectively, according to the American College of Rheumatology.
The treatment for RA and EORA may differ. Treating young adults with RA typically involves disease-modifying antirheumatic drugs and biologics. In comparison, doctors commonly treat those with EORA with lower dosages or less potent DMARDs, biologic medications, or both. Generally, they avoid corticosteroids for these individuals due to the long-term side effects.
The various ways that EORA presents can make it challenging for doctors to diagnose, and it requires different clinical and treatment approaches.
Recommended Reading: How Do You Find Out If You Have Rheumatoid Arthritis
Physical Exam And Medical History
The appointment will likely begin with the physician taking a thorough medical history. This will include asking the patient several questions, such as:
- What joints are affected?
- How would you describe the pain?
- Do you have morning stiffness?
- Have you noticed increased fatigue or weight changes?
- Have you experienced other symptoms besides joint pain?
- When did symptoms begin?
- How have symptoms changed over time?
- What movements or activities make the patient feel better or worse?
The history will also include a review of the patientâs:
- Other medical problems
See Lifestyle Factors and Fatigue Associated with Rheumatoid Arthritis
During the physical exam, a doctor will evaluate the patientâs general health and then examine the joints, looking for signs of joint inflammation. For example, a doctor may measure a jointâs range of motion, press the skin over a joint to see if it causes pain, and test joint strength.
Question 3 Of : Symptoms
Read Also: What Can I Do If My Dog Has Arthritis