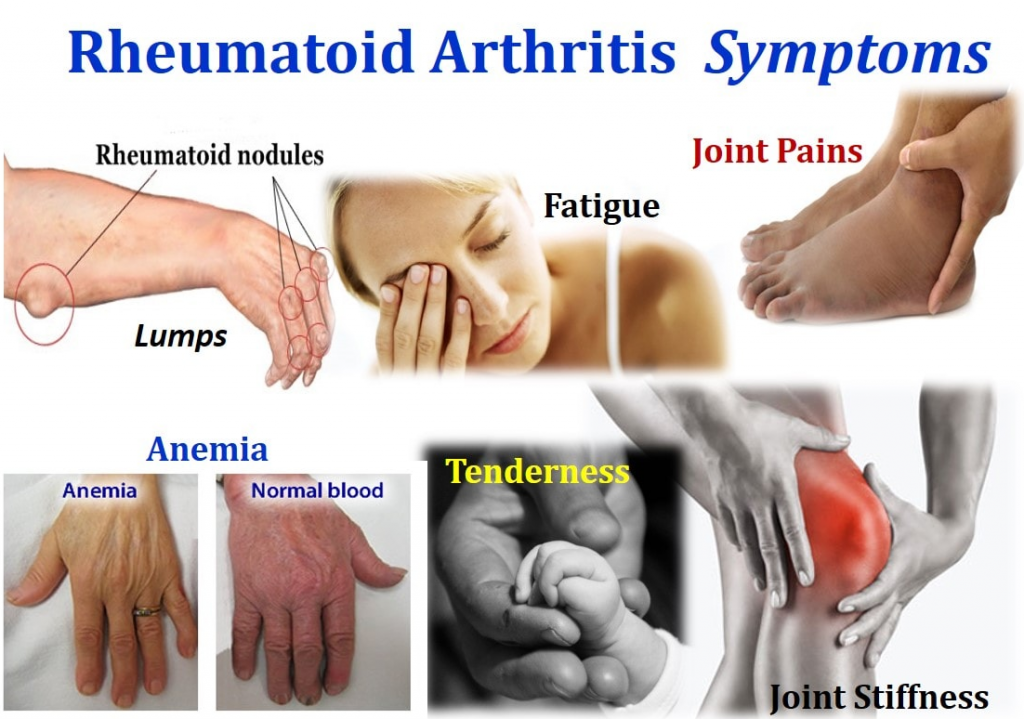
Symptoms Affecting The Joints
The main Rheumatoid Arthritis symptoms are affecting the joints are outlined below.
Pain
The joint pain linked with rheumatoid arthritis is normally a throbbing and aching pain. It is usually worse in the mornings and following a period of inactivity.
Stiffness
Joints swayed by rheumatoid arthritis can feel stiff. For instance, if your hands are affected, you may not be capable.Similar to joint pain, the stiffness is often more hard in the morning or after a time of inactivity. Morning stiffness linked with another type of arthritis called osteoarthritis normally wears off within 30 minutes of getting up, but rheumatoid arthritis morning stiffness usually lasts longer than this.
Swelling, warmth, and redness
The lining of joints affected by rheumatoid arthritis display inflamed, which can induce the joints to swell, and become hot and tender to touch. In some bodies, firm swellings called rheumatoid nodules can further develop under the skin around affected joints.As well as difficulties affecting the joints, some people with rheumatoid arthritis undergoing a range of more general symptoms, such as:
- Tiredness and a lack of energy
- Sweating
- Weight loss
What Should Be Done If Rheumatoid Arthritis Is Suspected
Any person who is suspected of having RA should be referred to a specialist rheumatologist. Early referral is important so that disease modifying anti-rheumatic drugs may be prescribed as soon as possible so as to slow or halt the disease process. Delay in referral or receiving a definitive diagnosis and treatment can result in significant costs to the individual, particularly those who are employed. This is because joint damage occurs most rapidly in the early stages of the disease, and often the treatment drugs can take several months to work.
Many areas now offer Early Arthritis Clinics where a rapid assessment is performed by specialists/specialist nurses in order to limit any delays. An ultrasound of the affected joints may be performed during this assessment.
If your symptoms are particularly severe when you first see your GP, then they may refer you urgently but also ring to speak to one of the local rheumatologists to ask for assistance in how to best help you in the meantime. Sometimes people are started on treatments other than those mentioned above, e.g. steroid tablets or a steroid injection, prior to being seen, in order to improve their condition. This though can affect what the specialists see and find at the first appointment, which can potentially delay their making a diagnosis or there may be increased uncertainty of the diagnosis.
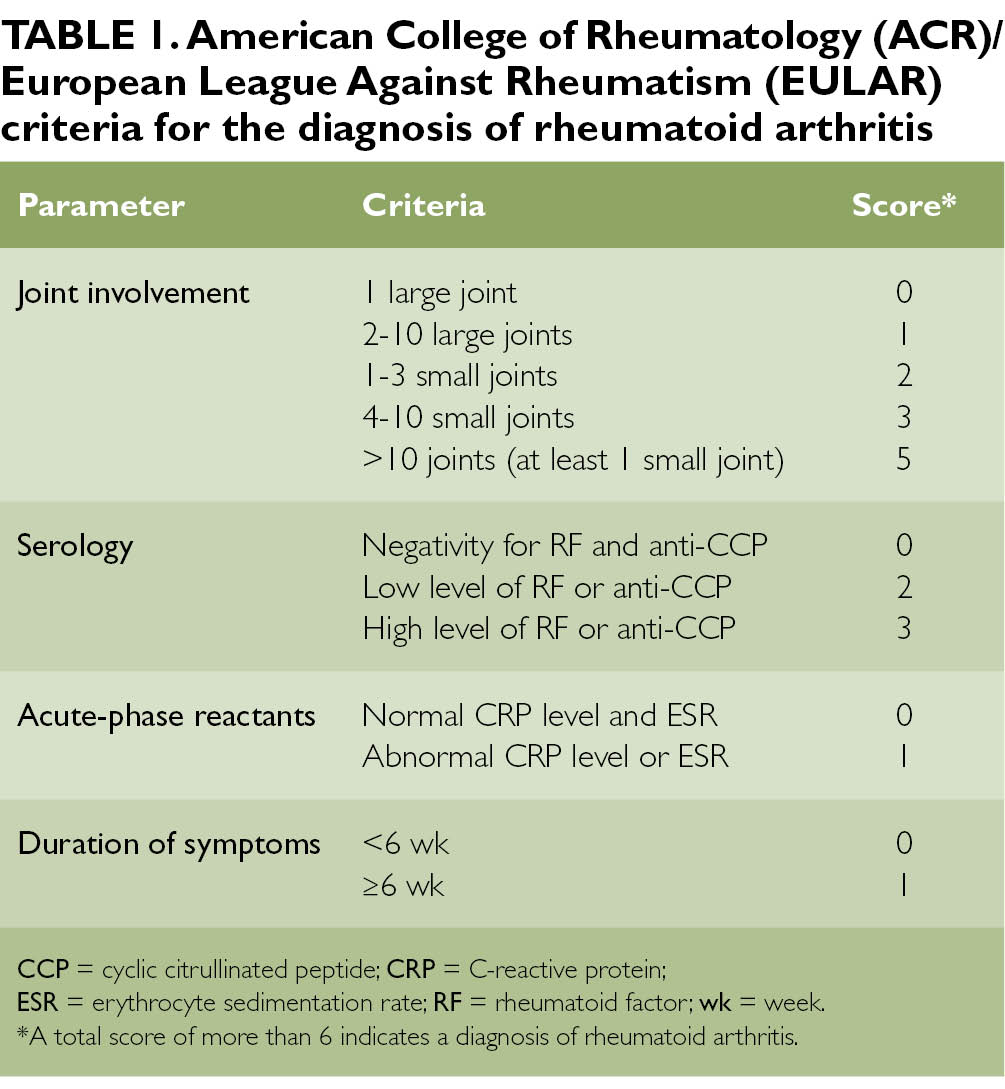
Reaching A Ra Diagnosis
Once all of these steps have been conducted, doctors will look at all of the test results and reach a conclusion based on the overall picture. Some doctors take a more symptom based approach to diagnosing RA while others rely on blood tests and medical history to confirm a RA diagnosis.
This is why its possible to be diagnosed with RA but not test positive for antibodies or have a medical history of RA in your family. If the symptoms themselves are consistent with RA, then it can still be diagnosed.
That being said, the main criteria for diagnosing RA do not change. The patient must exhibit symptoms for greater than six weeks, symmetrical symptoms, as well as multiple joints being affected including fingers and hands.
You May Like: How Do You Treat Arthritis In The Hip
Inflammation And Other Forms Of Arthritis
Some infections can lead to joint destruction and this occurs much quicker than with other forms of arthritis. It is crucial to rule out an infection when arthritis affects a single joint.
Gout: A common and painful condition that affects the joints and tendons. Small crystals of uric acid form in and around the joint which causes inflammation, pain and swelling. An attack of gout usually comes on very quickly, often overnight. The joint becomes red, swollen and painful. It often affects one joint at a time, such as the big toe.
Inflammation: A localised physical condition in which part of the body becomes reddened, swollen, hot, and often painful. Inflammation is a common symptom of arthritis, and is the cause and the result of all forms of arthritis.
This info sheet was reviewed and updated by Prof. Susanna Proudman, Medical Director, Arthritis Australia and Dr Stephen Adelstein, Pathology Awareness Australia ambassador.
Medication For Rheumatoid Arthritis
Some of the medications you may take include:
- pain relievers , such as paracetamol, for temporary pain relief
- non-steroidal anti-inflammatory medications , such as ibuprofen, to control inflammation and provide pain relief
- corticosteroids, such as prednisolone, to quickly control or reduce inflammation
- disease-modifying anti-rheumatic drugs , such as methotrexate, to control your overactive immune system
- biological and biosimilar medicines , such as infliximab these are biological disease-modifying drugs that work to control your immune system, but in a much more targeted way.
Depending on your particular symptoms, and how much pain and inflammation you have, you may take one medication or a combination of different medications.
Recommended Reading: What Foods Are Good To Eat For Arthritis
How Is Ra Diagnosed
RA is diagnosed by reviewing symptoms, conducting a physical examination, and doing X-rays and lab tests. Its best to diagnose RA earlywithin 6 months of the onset of symptomsso that people with the disease can begin treatment to slow or stop disease progression . Diagnosis and effective treatments, particularly treatment to suppress or control inflammation, can help reduce the damaging effects of RA.
Getting Tested For Rheumatoid Arthritis
Testing for rheumatoid arthritis is ordered by a doctor or specialist if indicated by a patients symptoms. Blood and urine samples used for testing can be obtained in a doctors office or other medical setting.
Synovial fluid is a liquid that is located in spaces between a persons joints, helping to cushion ends of bones and reduce friction during movement. For a synovial fluid analysis, a sample of synovial fluid is obtained during a procedure called a joint aspiration or arthrocentesis. During a joint aspiration, a doctor uses a needle to withdraw a sample of synovial fluid from a joint.
Don’t Miss: How To Relieve Neck Pain From Arthritis
Who Should Get Testing
Patients who experience inflammation, pain, or loss of mobility in joints should discuss testing for rheumatoid arthritis with their doctor, especially if symptoms occur in multiple joints or in matching joints on both sides of the body, such as both wrists. Other symptoms of rheumatoid arthritis include:
- Stiffness in the morning for 30 minutes or longer
- Fatigue
- Dry eyes and mouth
- Firm lumps beneath the skin
These symptoms are often due to something other than RA when they last less than six weeks. The longer a patient experiences symptoms, the more likely the symptoms are to be due to RA.
Diagnosing rheumatoid arthritis in its early stages can be challenging, as patients may experience few symptoms, but early diagnosis is important because early treatment may prevent joints from worsening or at least slow the process. When symptoms are present, they often differ from person to person and mimic the symptoms of other diseases. Testing is an important part of the process of determining whether symptoms are due to RA or another condition.
After receiving a diagnosis of RA, its important for patients to continue rheumatoid arthritis testing. Testing can assist doctors in assessing the severity of RA, as well as monitoring the efficacy of treatment, tracking disease progression, and detecting potentially serious side effects of treatment drugs.
What Are The Signs And Symptoms Of Ra
With RA, there are times when symptoms get worse, known as flares, and times when symptoms get better, known as remission.
Signs and symptoms of RA include:
- Pain or aching in more than one joint
- Stiffness in more than one joint
- Tenderness and swelling in more than one joint
- The same symptoms on both sides of the body
- Weight loss
Don’t Miss: Does Heat Make Arthritis Worse
Question 5 Of : Prognosis
Joint Stiffness & Loss Of Range Of Motion
Stiffness in the joints occurs when this disease is in an active state of inflammation, or when your immune system is actively attacking healthy tissue. Oftentimes, the greatest amount of stiffness occurs in the mornings, but it can continue throughout the day as well.
Dealing with this type of stiffness, as well as overall joint swelling, can result in the loss of range of motion if rheumatoid arthritis treatment is not sought early or if the disease is too advanced. In more advanced RA, the range of motion can be permanently lost in certain joints.
Working with a qualified physical therapist may help preserve or extend the range of motion for RA patients. Other treatment methods, such as taking nonsteroidal anti-inflammatory drugs, can help as well.
Don’t Miss: Is Protein Good For Arthritis
Common Rheumatoid Arthritis Symptoms
Symptoms experienced by rheumatoid arthritis patients are a direct result of the inflammation of joint tissue and/or accumulation of synovial fluid caused by this autoimmune disorder.
An autoimmune disorder is a disease in which the bodys immune system attacks healthy tissue, mistaking it for foreign or damaged tissue. Though there are many types of autoimmune diseases, such as multiple sclerosis and systemic lupus erythematosus, rheumatoid arthritis is one that afflicts roughly 1.5 million Americans.
Symptoms of RA can range from mild to debilitating, and every level in between. However, there are some common overall symptoms to be aware of should you suspect that you or someone you know is suffering from rheumatoid arthritis.
Below are the most commonly reported rheumatoid arthritis symptoms:
What Else Could It Be
When a doctor thinks about how likely you are to have one disease over another, or over several others, this is called a differential diagnosis. There are many conditions your doctor may consider besides RA, and besides other forms of autoimmune arthritis:
Viral arthritis: Rubella, parvovirus, and hepatitis B and C can lead to short-term arthritis symptoms that resemble RA.
Palindromic rheumatism: Periodic joint inflammation that may lead to RA, lupus, and similar diseases
Polymyalgia rheumatica: This is more common over age 50, generally less painful than RA, and associated more with shoulders and hips.
Also Check: Are Bunions Caused By Arthritis
How To Prepare For An Initial Doctors Appointment
During your first appointment, your doctor will conduct a physical exam, collect details about your medical history, and discuss which symptoms you may be experiencing.
Generally, they will evaluate your joints for inflammation, swelling, and redness and may order imaging tests or blood work to determine if you have RA.
Be sure to keep track of all your symptoms and consider logging the time, duration, and severity of each symptom as it occurs. You should also provide your doctor with information about any medications that you are taking, including the frequency and dosage.
Keep in mind that you may not receive a definitive diagnosis on your first visit, as many autoimmune disorders develop slowly over time.
However, your doctor may discuss possible treatment options with you, which can include medications, physical therapy, pain management, exercise, and other modifications to your diet and lifestyle.
Its important to discuss any questions you have regarding your treatment plan with your doctor. Some questions you may want to consider asking:
- What treatment options are right for me?
- What are the potential side effects from my treatment?
- What types of exercise would be beneficial? How often should I work out?
- Are there other ways to treat symptoms at home, such as by using a hot or cold compress?
- What options available for mental health support, if needed?
- Would I benefit from physical therapy, nutrition counseling, or other complementary treatments?
Is Rheumatoid Arthritis Hereditary
Rheumatoid arthritis isnt considered a hereditary disease, yet it does appear to run in families. This may be due to environmental causes, genetic causes, or a combination of both.
If you have family members who have or have had RA, talk to your healthcare provider, especially if you have any symptoms of persistent joint pain, swelling, and stiffness unrelated to overuse or trauma.
Having a family history of RA increases your risk of getting the disease, and early diagnosis can make a big difference in how effective treatment will be.
Recommended Reading: What Foods Help Reduce Arthritis Pain
How Is Seronegative Rheumatoid Arthritis Diagnosed
Some patients still have RA but do not test positive for either anti-CCPs or RF they have seronegative RA.
Annals of the Rheumatic Diseases
Your doctor may also conduct a synovial biopsy, which involves removing a small piece of the tissue lining one of your joints.
RELATED: Psoriatic vs Rheumatoid Arthritis: Whats The Difference?
Human Leukocyte Antigen Tissue Typing
This test checks for a genetic marker called human leukocyte antigen .
Some studies suggest that around 60% of RA cases may be inherited. If a person has specific antigens, it could mean that they have a higher likelihood of developing RA. However, other factors, such as tobacco use, can also trigger the condition.
HLA markers in the blood can help indicate the likelihood of developing an immune-related condition such as RA. These markers may also be a sign of another condition, such as ankylosing spondylitis or reactive arthritis.
Also Check: Does Arthritis Qualify For Social Security Disability
Diagnosis Of Rheumatoid Arthritis
The usual symptoms of rheumatoid arthritis are more flu like, and include muscle aches, low grade fever, reduced appetite, and perspiration of feet and hands. But, these symptoms get misdiagnosed as flu signs.
In several cases, additionally, one may also observe swollen, painful and red joints that are warm to touch. This gives a clear identification of rheumatoid arthritis and rules out flu possibilities. In rheumatoid arthritis, the joint symptoms appear symmetrically.
If one of the hands gets affected, the other hand is bound to be affected at the same moment. There is no specific test to identify rheumatoid arthritis.
Doctors diagnose it based on various factors associated with this disease. Still, few tests are there that help to diagnose it.
Have Your Inflammation Levels Checked
In addition to the presence of antibodies that are hallmarks of an autoimmune condition like RA, your doctor may administer two other tests that rummage around for markers of inflammation within the bodyanother indicator for the disease. the primary test measures erythrocyte ESR while the opposite takes stock of your serum globulin levels within the blood. along with information from your antibody test, these are useful tools to see if questions about RA.
Recommended Reading: Is Arthritis And Autoimmune Disease
Tests That Help Diagnose Ra
To help confirm or disprove RA, your rheumatologist will also have lab tests done. The lab tests would point to likelihood of rheumatoid arthritis, as well as potentially rule out other possibilities on the differential diagnosis, says Dr. Neogi. These tests may include:
Erythrocyte sedimentation rate and C-reactive protein blood tests detect and measure inflammation in your body. If inflammation levels are elevated, it helps build the case for an RA diagnosis. If inflammation levels are normal, says Dr. Neogi, That might dissuade us from thinking about an inflammatory arthritis like rheumatoid arthritis, but would not rule it out. Since inflammation is present in many diseases, these tests do not confirm whether you have RA by themselves.
Rheumatoid factor and anti-cyclic citrullinated peptide antibody blood tests look for proteins associated with RA. Testing positive for one increases your chances of RA diagnosis, while testing positive for both raises your odds even more. However, up to 50 percent of RA patients dont have RF or anti-CCP antibodies. They are diagnosed based on other factors. In these cases, the RA is considered to be seronegative.
The possibility of some autoimmune disorders, such as lupus and Sjögrens syndrome, can be eliminated with the help of an antinuclear antibody blood test, while a synovial fluid analysis, which examines the fluid that lubricates your joints, can help count out gout by looking for crystals under the microscope.
Know Your Medical Record
GettyImages
Your rheumatologist will likely ask you questions about your family and their anamnesis. RA is a disease-related to certain genetic markers, so if a relative has it, that produces it more likely that you simply have it also. Your doctor will ask about your symptoms: once they developed, which joints are hurting, whether the swelling is symmetric if symptoms are consistent or on-and-off and whether youve experienced anything like this within the past.
You May Like: Is Cherry Juice Good For Rheumatoid Arthritis
Blood Tests For Rheumatoid Arthritis
RA is an autoimmune disease. Several blood tests can detect immune system changes or antibodies that may attack the joints and other organs. Other tests are used to measure the presence and degree of inflammation.
For blood tests, your doctor will draw a small sample from a vein. The sample is then sent to a lab for testing. Theres no single test to confirm RA, so your doctor may order multiple tests.
How Else Can Your Gp Surgery Help
Your GP surgery can be involved in your RA care in many different ways. They continue to look after you in general and may want to keep a close eye on your blood pressure, cholesterol and blood glucose levels as there is a higher risk of heart disease in people affected by rheumatoid arthritis. This is often done as an annual review with one of the practice nurses. Many GP surgeries are involved in doing the blood monitoring for the specific drugs used in controlling and treating the joint inflammation , so you may get your regular blood tests performed by your surgery.
Rheumatoid arthritis, along with many of the treatments used affects the bodys immune response to infections. Your surgery may therefore contact you to offer you annual influenza jab and also a Pneumovax for pneumonia . With some of these treatments live vaccines should be avoided so please ensure you contact your Doctors surgery if you are planning to travel abroad.
Don’t Miss: What Drugs Are Used To Treat Rheumatoid Arthritis