The Importance Of Early Diagnosis Of Ra
In a study of Frech cohort, only 50.9% of RA satisfied 1987 ACR revised criteria for diagnosis of RA in 1 year . However, in the absence of treatment inflammation will lead to articular damages and bone erosion particularly within the first two years of disease onset . Regarding the current concept of “window of opportunity”, early diagnosis of RA is essential for initiation of treatment, otherwise, disease will progress to more severe forms requiring more aggressive therapy .
Application of recently developed diagnostic criteria provided an opportunity to identify and treat those patients with early inflammatory arthritis who progress to future RA. Using this criteria can discriminate inflammatory arthritis who fulfil the 1987 ACR criteria in the future from those who do not develop RA. The new 2010 criteria is a diagnostic tool with higher sensitivity and specificity compared to previous ACR-criteria. The new criteria classify greater number of patients at earlier phase with reasonable discriminative ability .
What Does Early Rheumatoid Arthritis Treatment Look Like
The first-line treatment for RA is usually a DMARD called methotrexate . You may also get steroids or corticosteroids as an anti-inflammatory. That’s enough for most people, though some may need to increase the dose. That brings us to the next decision point: Is the methotrexate enough? If its not enough, you might need to add in another medication, such as TNF-blocking drugs, which are also anti-inflammatories, says Niewold.
The Significance Of Inflammation
The cytokine milieu in rheumatoid arthritis influences a multitude of physiological processes. These include promoting the influx of immune effector cells into the joint synovium, and activation of osteoclasts, chondrocytes and fibroblasts.3 There is a positive feedback loop that reinforces the inflammatory process. Unabated, this process results in joint pain and destruction, ultimately causing deformity and disability.
Chronic inflammation also contributes to an increased risk of myocardial infarction, stroke and death. A Canadian population-based prospective cohort study reported an absolute increase in cardiovascular events of 5.7 per 1000 person-years in patients with rheumatoid arthritis compared to those without.4 The use of disease-modifying antirheumatic drugs to attenuate the inflammatory process has been shown to prevent joint erosions and reduce pain, cardiovascular morbidity and mortality.3,5
You May Like: What’s Good For Arthritis In Fingers
Biologic Agents Side Effects
A variety of infections have been described associated with the use of anti-TNF agents. Most common has been tuberculosis. For this reason, before any anti-TNF agent is used, the patient should have a PPD skin test or Quantiferon Gold skin test. If positive, and if the patient is previously untreated, treatment of latent tuberculosis is begun before the patient is given an anti-TNF agent. Anakinra seems less likely to activate tuberculosis than the anti-TNF agents.
Due to described worsening of multiple sclerosis in patients treated with biologic agents, and rare cases of new multiple sclerosis-like lesions developing in patients not symptomatic prior to starting a biologic agent, it is advised to use great caution in using anti-TNF agents in patients with multiple sclerosis. Other side effects of biologic agents include:
- Opportunistic infections in addition to tuberculosis: e.g., atypical mycobacteria, pneumocystis infection, histoplasmosis…
- Rare reports: pancytopenia and aplastic anemia
- Rare elevations liver function tests
- Lymphoma so far increased risk not shown data to date suggests that the rheumatoid arthritis disease severity is associated with risk of lymphoma and that adding TNF blockade does not increase lymphoma risk in adults
- Skin cancers : it appears that TNF blockers increase the risk of squamous cell and basal cell carcinomas of the skin. Patients on TNF blockers should get yearly total body skin checks.
Current Treatment Practice: Biologic Response Modifiers
Following the introduction of the first TNF inhibitors, biologic response modifiers targeting other components of the immune response involved in the pathogenesis of RA have been approved for clinical use. Anakinra, a recombinant human soluble IL-1 receptor antagonist, can be administered subcutaneously daily to treat patients with RA. Abatacept, a recombinant fusion protein that combines the T-cell co-stimulation inhibitory molecule CTLA-4 with the Fc region of human IgG, may be given subcutaneously weekly or intravenously monthly. Rituximab, a chimeric mAb directed against the surface molecule CD20 on B cells, is administered in two i.v. doses given 2 weeks apart, usually every 6 months. Most recently, tocilizumab, a humanized mAb directed against the IL-6 receptor, has been approved for monthly i.v. administration to patients with RA. Specifics regarding the biologic response modifiers approved for the treatment of RA are summarized in .
You May Like: Is Tiger Balm Good For Arthritis
Treatment In Early Ra
The armamentarium of available antirheumatic treatments has increased tremendously during the last years and includes today three major groups of DMARDs: conventional synthetic DMARDs , with methotrexate being the anchor drug in this category biologic DMARDs , targeting cytokines and cells of the immune system that are important players in the immunopathogenesis of RA , rituximab, tocilizumab, abatacept, sarilumab) and targeted synthetic DMARDs . The last category includes tofacitinib and baricitinib, two Janus Kinase inhibitors that have received approval for the treatment of RA.
Percentage of methotrexate-naïve patients with RA achieving remission with methotrexate monotherapy or methotrexate in combination with biologic DMARD or targeted synthetic DMARD. DMARD, disease-modifying antirheumatic drug MTX, methotrexate RA, rheumatoid arthritis.
What Drugs Are Used To Treat Rheumatoid Arthritis
The youll wind up on will depend on your symptoms and disease severity. To help lessen your pain and inflammation, your rheumatologist may initially suggest over-the-counter or prescription non-steroidal anti-inflammatories or a short course of corticosteroids. But the ultimate goal is to stop or slow the progression of the disease, preventing potentially debilitating cartilage and bone damage. For that, your physician will likely start with disease-modifying anti-rheumatic drugs . These medications slow down your overactive immune system, so it doesn’t attack the tissue lining your joints.
Which medication specifically your doc chooses depends on your disease severity. In RA, the goal is to match the strength of medication to the degree of inflammation in the patient’s body. If someone has low disease activity, we may offer hydroxychloroquine, which is the least immunosuppressive of the bunch, says Saika Sharmeen, M.D., assistant professor in the division of rheumatology at Stony Brook Medicine in Stony Brook, NY.
Also Check: Is Turkey Bad For Arthritis
Whats The Rush For Treating Rheumatoid Arthritis Asap
This push to begin treatment immediately may seem hasty, but there are important reasons to start early. “There is a progression of damage to joints that is irreversible. Your body tries to heal it, but its really never the same. A number of studies have shown that sometimes even when someone is first diagnosed with RA, you can already see some of these changes on X-rays and MRIs. That tells us that we have to think of treatment right away, says Timothy Niewold, MD, director of the Colton Center for Autoimmunity and a professor of medicine at the New York University Grossman School of Medicine in New York City.
Treatment Of Stage 4 Ra
After trying all medical options, surgery may be the next option for patients with stage 4 RA. Surgery may be required to repair joint damage, repair tendons, remove the synovium or nodules, separate fused joint, or replace a damaged joint.
Patients usually rely on assistive mobility devices to perform their daily tasks.
Read Also: Can You Have Arthritis In Your Back
Can I Cut Back On My Ra Medications If I Feel Ok
If pain and stiffness start to fade, you may wonder if you can change your medications.
RA is a long-term condition, and medicine keeps your symptoms under control. But with guidance from their doctor, some people may be able to lower the amount of medication they take.
When was your last flare?
Studies show that people who stop their RA medicine are likely to have a flare of symptoms 4 to 8 weeks later. If your disease stays active, you’re more likely to get permanent joint damage.
Your doctor will want to know how long it’s been since you had any problems. They’ll also do some tests. If everything looks good, your doctor may slowly lower the dose of your medications, usually starting with NSAIDs.
You want to keep a constant and effective level of your RA drugs in your system, so if you are able to cut back on your medicine, it would be a slow change. It helps if you take your medicine at the same time every day.
Do you have any trouble with side effects from your meds?
If so, tell your doctor about them. They may be able to adjust your medicine. For example, many drugs used to treat RA can cause an upset stomach. To help, your doctor may suggest that take it at a different time or with food. They may also recommend medication to ease nausea and help with stomach acid.
Do you use reminders to help you take medicine on time?
Lifestyle Changes Are Also Key To Early Ra Treatment
Niewold recommends taking the following steps to improve your health with RA:
- Stop smoking.There is some risk of getting RA from smoking, and if you continue to smoke while taking RA meds, they dont work as well you tend to have more disease activity and more damage.
- Engage in low-impact exercise.If you are able to get active and push back against stiffness, it goes away faster. Yoga is good because in involves both moving and stretching.
- Lose weight.Shedding extra pounds will mean less strain on your joints in general.
- Change your diet.Many people with RA say that following an anti-inflammatory diet has helped with their symptoms. Its hard to know if it really affects joint inflammation, but patients do report they have more energy and a little better mobility. Its a subtle effect its not a cure but its not a bad thing to try, says Niewold.
- Work with your rheumatologist to find the right treatment plan for you. And if at present you arent feeling relief from your course of disease management, dont give up, says Niewold. There are lots and lots of tools in the toolbox now.
Read Also: How To Help Arthritis In The Hip
Rheumatoid Arthritis Drugs With The Least Side Effects
First, lets get this out of the way: All drugs come with side effects. Your physician will balance your quality of life with the severity of the disease when choosing the right med for you. The RA drug with the least side effects is hydroxychloroquine . We dont consider it immunosuppressive, and it doesnt cause elevated liver markers or kidney issues like some of the other drugs, says Dr. Sharmeen. However, that doesnt mean its without side effects at all. We have patients monitored by an ophthalmologist for retinal toxicity, which can happen over 10 years, she says.
Methotrexate, considered a first-line drug for moderate RA, is also well tolerated. But it can cause elevated liver enzymes. When choosing between the two, your doctor will consider your lifestyle. For example, if you drink alcohol, methotrexate may not be your best option.
Data Abstraction And Data Management
To ensure accuracy, two reviewers will independently review all titles and abstracts. We will use Abstrackr, an online citation screening tool, to review title and abstract records and manage the results.24 We will then retrieve the full text for all citations deemed potentially appropriate for inclusion by at least one of the reviewers. Two team members will independently review each full-text article, including any articles that peer reviewers suggest or that may arise from the public posting process, for eligibility. Any disagreements will be resolved by a third team member or consensus. We will maintain a record of studies excluded at the full-text level with reasons for exclusion and will include this list in our final report.
After we select studies for inclusion, we will abstract data into categories that include the following: study design, eligibility criteria, intervention , additional medications allowed, methods of outcome assessment, population characteristics, sample size, attrition , results, and AE incidence. A second team member will verify abstracted study data for accuracy and completeness.
You May Like: What Can Rheumatoid Arthritis Lead To
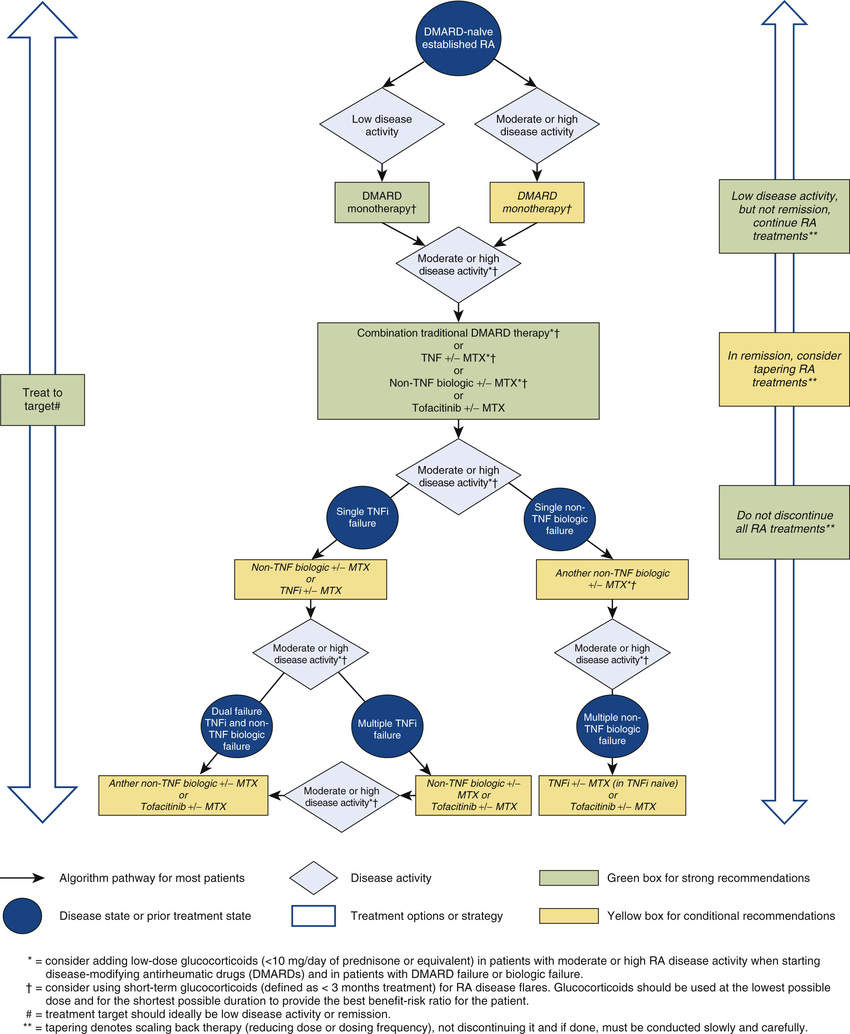
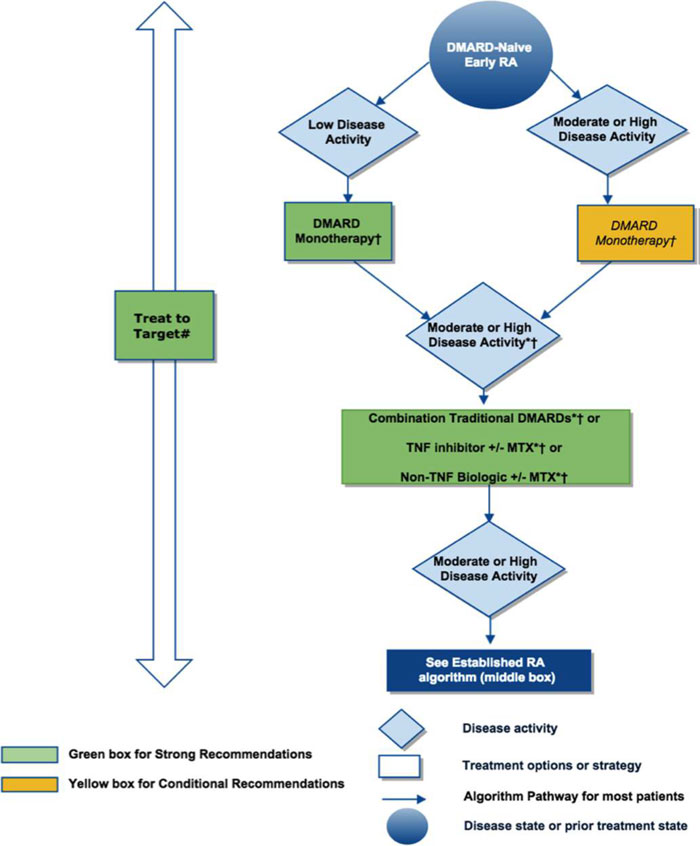
The American College Of Rheumatologys Updated Rheumatoid Arthritis Treatment Guidelines Emphasize Treating Newly Diagnosed Patients With Methotrexate First And Managing Using A Treat
Treatment options for rheumatoid arthritis , a chronic inflammatory disease that causes pain, stiffness, swelling, and loss of function in joints, have expanded dramatically over the past few decades. At the same time, doctors and researchers continue to gain new knowledge about the safety and efficacy of these available treatment options.
How can health care providers stay up to date and ensure that patients are getting the best available care? Thats where the American College of Rheumatology treatment guidelines, which are updated every five years, can provide some direction.
The latest version of the guidelines, which was released this month and published in the journal Arthritis Care & Research, is based on a comprehensive literature review of high-quality research as well as the opinions of a voting panel comprised of 13 leading rheumatologists and two patient representatives. The goal of the guidelines is to provide current, science-backed advice on how to best manage this inflammatory disease.
Although these guidelines are primarily aimed at helping doctors make informed decisions about patient treatment, they are also beneficial for people with RA to know about.
Keep in mind that the recommendations in these guidelines are a tool and not the final word on what will work best for you. Individual treatment decisions should always include input from patients and providers and take a variety of factors into account.
Medications For Rheumatoid Arthritis
In the present era, all patients with rheumatoid arthritis benefit from medications of some type, and often require a combination of medications. Analgesics such as acetaminophen are very commonly used by patients with RA. The vast majority of patients with RA end up requiring DMARDs and many benefit from having such agents started quite early in their course.
Spectrum of pharmacotherapy for rheumatoid arthritis:
- Steroids: e.g., prednisone and methylprednisolone
- Disease-modifying agents : hydroxychloroquine, sulfasalazine, methotrexate, leflunomide
- Biologic agents
- JAK inhibitors: e.g., tofacitinib
Recommended Reading: Is Spicy Food Good For Arthritis
Side Effects Are Par For The Course For All Medications But Which Ra Drugs Carry The Least Amount Find Out Here
by Health Writer
If you suspect you may have rheumatoid arthritis or your doctor has recently diagnosed youthen youre probably already experiencing the classic symptoms of painful, achy, and swollen joints, especially first thing in the morning or after a long day sitting at work.
Unlike other types of arthritis that can be brought on by too much activity, rheumatoid arthritis symptoms tend to happen when youve been at rest, not using your joints. Maybe you wake up in the morning and feel stiff. Or maybe you get out of the car after a long trip and find your body will barely move. The discomfort in your joints is the result of an overactive immune system that mistakenly attacks the tissue that lines your joints. The result is pain and inflammation and, over time, damage to the joints that can lead to deformity and disability. You may not know anyone else with the disease, but if you have rheumatoid arthritis, youre in good company: RA is the second most common type of arthritis, affecting 1.3 million Americans.
The good news about rheumatoid arthritis is that there are many different . When someone comes in with rheumatoid arthritis, I tell them that I can get them feeling better and halt the progression of their disease, says Rebecca Blank, M.D., Ph.D., a rheumatologist at NYU Langone Health in New York City. The question is, which treatments work best and which ones are safest? Start with these joint-saving options.
Pregnancy Contraception And Lactation
The management of rheumatoid arthritis before, during and after pregnancy can be challenging. Although many women will have an improvement in disease activity during pregnancy, remission is rare.17 Poor pregnancy outcomes occur more commonly with high disease activity and include miscarriage, prematurity and pre-eclampsia.17 With the exception of sulfasalazine and hydroxychloroquine, all DMARDs are considered either unsafe or of uncertain safety during pregnancy.18 Counselling on effective methods of contraception is essential to prevent unplanned pregnancy while taking teratogenic drugs.17 Planned pregnancy is preferable and allows time for appr opriate treatment changes to be made while optimising disease control. Certain DMARDs must be stopped at least 36 months before conception.18
During lactation the immunosuppressive effects of some DMARDs may affect the infant because of drug excretion into breast milk. Information on drugs and lactation can be found at United States National Institute of Health Lactmed or via local medicines information services.
Read Also: Can Hip Arthritis Cause Groin Pain
Rheumatoid Arthritis Treatment And The Wildfire Analogy
Zerbini explains that early treatment that stops disease activity also stops joint and bone destruction. “You may compare the inflammatory process in the beginning of the disease to a bonfire that may become a fire, destroying the joint and adjacent bone if not eliminated by treatment as soon as possible, he says. The bottom line: Do not delay treatment.
Zerbini adds, The active disease leads to a continuous loss of bone and consequently to osteoporosis, leaving the patient with a high probability of a low trauma fracture. The pain and deformity prevent the ability to exercise, which contributes to additional loss of bone.
Tocilizumab In The Treatment Of Rheumatoid Arthritis And Beyond
Accepted for publication 21 January 2014
28 March 2014Volume 2014:8 Pages 349364
Introduction
Tocilizumab , a new drug targeting the IL-6 pathway, was approved in 2010 for the treatment of moderate to severe RA in patients who have failed other DMARDs, including biologics. It is the first humanized IL-6 receptor-inhibiting monoclonal antibody.8 IL-6 is a 26 kDa glycopeptide. This cytokine plays a role in inflammation, bone metabolism, hematopoiesis, and immune regulation. IL-6 is produced by various cell types, predominantly macrophages and fibroblasts.9 IL-6 is known to be produced in high quantities in the synovial fluid of patients with RA and these elevations correlate with disease activity and joint destruction.10
The purpose of this paper is to review the role of TCZ in the treatment of RA, focusing on the pharmacology, efficacy, and safety of this drug as demonstrated by important clinical trials. Lastly, we will address the evolving role of TCZ in the future.
Pathogenesis of RA and the role of IL-6
Pharmacokinetics and metabolism
Drug interactions
Key studies of TCZ
SATORI: monotherapy DMARD failure
SAMURAI: monotherapy DMARD failure radiographic progression with TCZ
LITHE: combination therapy DMARD failure radiographic progression with TCZ
CHARISMA: combination therapy previous DMARD failure
OPTION: combination therapy previous DMARD failure
TOWARD: combination therapy previous DMARD failure
ROSE: combination therapy previous DMARD failure
Also Check: How To Get Rid Of Arthritis In Your Back