Do You Need To Modify Rheumatoid Arthritis Medications Before Or After Getting The Vaccine
Temporarily stopping certain immunosuppressant medications after receiving the vaccine, or timing when you get the vaccine in the course of your treatment, might help increase the effectiveness of the COVID-19 vaccine if you have RA.
But whether this is right for you depends on a number of factors, including which medications you take and your overall health. For example, if your RA is not well-controlled and skipping medications is likely to cause you to flare, your doctor may suggest that you keep taking them. You and your doctor should decide together about making any medication changes. You should not stop taking any of your rheumatoid arthritis medications on your own.
Most disease-modifying antirheumatic drugs, including biologics, should not be stopped for those with rheumatoid arthritis. Here are the RA drugs for which the ACR guidance suggests changes may be recommended:
- Methotrexate: Skip for 1 week after each vaccine dose
- JAK inhibitors : Skip for 1 week after each vaccine dose
- Abatacept , injectable form: Skip one week before and after the first vaccine dose only
- Abatacept , IV form: Get COVID-19 vaccine 4 weeks after your last infusion, then skip a week and get next infusion
- Rituximab : Get COVID-19 vaccine approximately 4 weeks before next infusion, then delay next infusion by 2-4 weeks after second vaccine dose if possible
- Cyclophosphamide infusion: Time administration so its one week after each COVID-19 vaccine dose
Question 1 Of : Background
Question 5 Of : Prognosis
Don’t Miss: Is Marijuana Good For Arthritis Pain
Rheumatoid Arthritis: Causes Symptoms Treatments And More
Rheumatoid arthritis is an inflammatory type of arthritis that can causes joint pain, swelling and damage. Learn what causes RA and how to treat it.
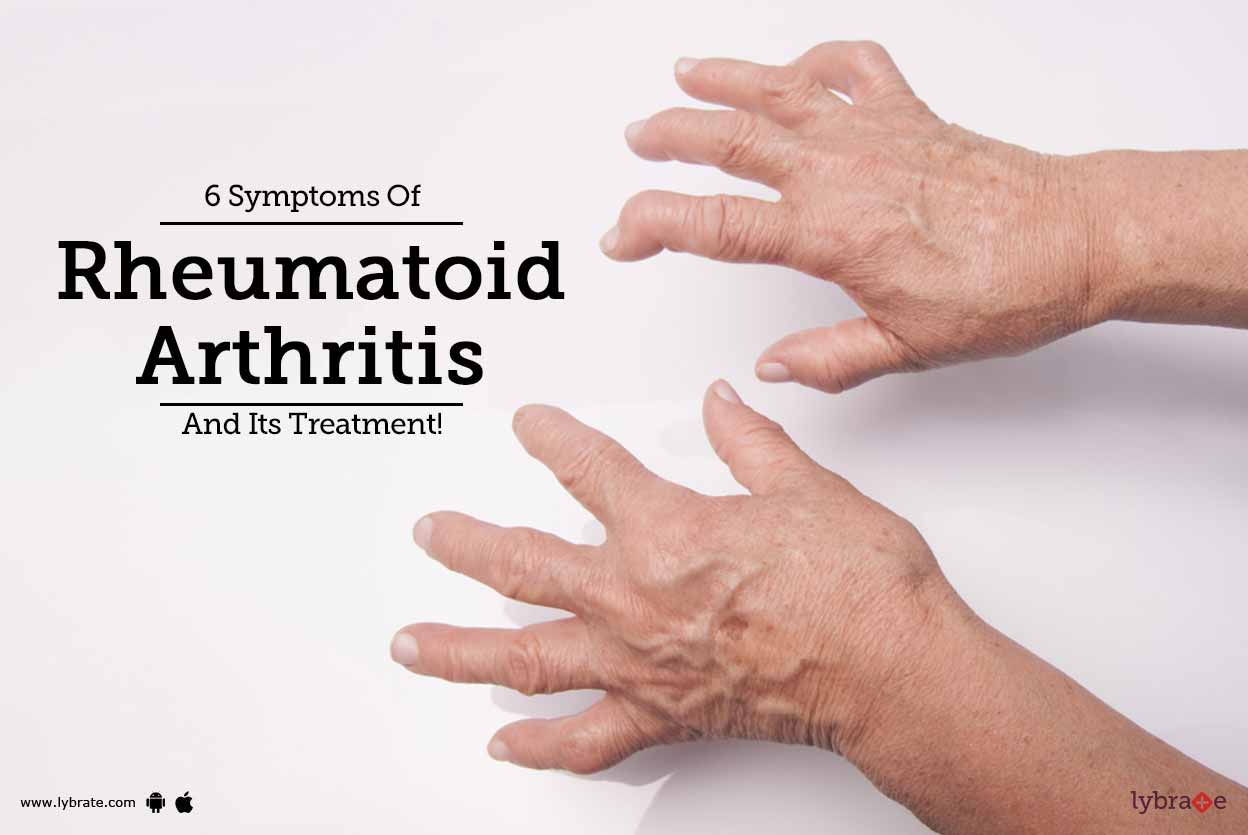
Rheumatoid arthritis causes joint inflammation and pain. It happens when the immune system doesnt work properly and attacks the lining of the joints . The disease commonly affects the hands, knees or ankles, and usually the same joint on both sides of the body. But sometimes, RA causes problems in other parts of the body as well, such as the eyes, heart and circulatory system and/or lungs. For unknown reasons, more women than men get RA, and it usually develops in middle age. Having a family member with RA increases the odds of developing RA.
Causes
In a healthy person, the immune system fights invaders, such as bacteria and viruses. With an autoimmune disease like RA, the immune system mistakes the bodys cells for foreign invaders and releases inflammatory chemicals that attack, in the case of RA, the synovium. Thats the tissue lining around a joint that produces a fluid to help the joint move smoothly. The inflamed synovium gets thicker and makes the joint area feel painful and tender, look red and swollen and moving the joint may be difficult.
Researchers arent sure why some people develop RA. They think that these individuals have certain genes that are activated by a trigger in the environment, like a virus or bacteria, or physical or emotional stress or some other external factor.
Symptoms
What Imaging Techniques May Be Used To Diagnose Arthritis
Imaging techniques may give your healthcare provider a clearer picture of what is happening to your joint. Imaging techniques may include the following:
-
X-ray. X-rays may show joint changes and bone damage found in some types of arthritis. Other imaging tests may also be done.
-
Ultrasound. Ultrasound uses sound waves to see the quality of synovial tissue, tendons, ligaments, and bones.
-
Magnetic resonance imaging . MRI images are more detailed than X-rays. They may show damage to joints, including muscles, ligaments, and cartilage.
-
Arthroscopy. This procedure uses a thin tube containing a light and camera to look inside the joint. The arthroscope is inserted into the joint through a small incision. Images of the inside of the joint are projected onto a screen. It is used to evaluate any degenerative and/or arthritic changes in the joint to detect bone diseases and tumors to determine the cause of bone pain and inflammation, and to treat certain conditions.
Read Also: Is Banana Good For Rheumatoid Arthritis
What Are The Signs And Symptoms Of Ra
With RA, there are times when symptoms get worse, known as flares, and times when symptoms get better, known as remission.
Signs and symptoms of RA include:
- Pain or aching in more than one joint
- Stiffness in more than one joint
- Tenderness and swelling in more than one joint
- The same symptoms on both sides of the body
- Weight loss
Talk With Others Who Understand
On myRAteam, the social network for people with rheumatoid arthritis and their loved ones, more than 147,000 members come together to ask questions, give advice, and share their stories with others who understand life with rheumatoid arthritis.
Are you living with rheumatoid arthritis and considering biologic treatment? Share your experience in the comments below, or start a conversation by posting on your Activities page.
Recommended Reading: Is Coffee Good For Rheumatoid Arthritis
Referral To A Rheumatologist Tests & Diagnosis Of Rheumatoid Arthritis
A diagnosis is usually made by one of three routes. Some GPs carry out tests, make the diagnosis and then refer the person to a specialist – a rheumatologist, at their local hospital or a specialist hospital. For many people, after having discussed the initial symptoms with their GP, the GP will suspect that it is some form of arthritis but will refer the person to the rheumatologist to make a specific diagnosis of RA. A few people, who have quite severe symptoms at the start, go into hospital for care and tests to establish the cause.Some people we interviewed were referred to the rheumatologist straight away, but this can vary and there can be delays in diagnosis. One woman then aged 30, was a bit worried at being given an ‘urgent referral’, but was relieved when she saw the consultant and got a diagnosis.
Then Theyll Run More Tests
Doctors will also likely measure your overall level of inflammation using two common tests: C-reactive protein and the erythrocyte sedimentation rate . Not everyone with rheumatoid arthritis has elevated levels, but when the numbers are high, the findings can help confirm the diagnosis. If a patient has elevated ESR and/or CRP levels, it would imply they have an inflammatory kind of arthritis, versus osteoarthritis, Dr. Cohen says. Your doctor may continue to use these tests to monitor your disease and inflammation levels over time.
Recommended Reading: Does Rheumatoid Arthritis Affect Your Toes
How To Get Tested
Rheumatoid factor testing is ordered by a doctor. A patients doctor may suggest a rheumatoid factor test alone, but usually this test is used along with other tests to evaluate a patient for an autoimmune disorder. RF testing requires a blood sample that is normally drawn in a doctors office, hospital, or laboratory.
Tests For Rheumatoid Arthritis
If your doctor suspects that your joint pain and tenderness could be signs of rheumatoid arthritis, hell most likely refer to you a rheumatologist for testing to confirm the diagnosis. Naturally, youll feel a little nervous as you wait to see this new doctor, and youll probably have a lot of questions, too including wondering what tests are done to diagnose rheumatoid arthritis.
The good news is that rheumatoid arthritis tests are mostly non-invasive and not painful. However, you should prepare for a relatively long appointment. Diagnosing rheumatoid arthritis requires a very comprehensive exam because there is no one specific test that tells us a patient has RA, says John Davis III, MD, a rheumatologist and internist at the Mayo Clinic in Rochester, Minnesota. I set aside an hour to evaluate a new patient.
Is there a test for rheumatoid arthritis? Yes but its not just one test that can confirm the diagnosis. Here are the key components of tests for diagnosing rheumatoid arthritis:
Recommended Reading: What Is The Best Biologic For Rheumatoid Arthritis
Can My Doctor Use Imaware Results
Yes. All of our tests are performed by CLIA-certified labs, the gold standard in lab testing quality regulation. Within your results report you will also find detailed information intended for your healthcare professional. They can use this information to interpret your test results clearly. To see an example of this, you can request a sample report at the top of this page.
Rheumatoid Factor And Anti
One blood test measures levels of rheumatoid factors in the blood. Rheumatoid factors are proteins that the immune system produces when it attacks health tissue.
About half of all people with rheumatoid arthritis have high levels of rheumatoid factors in their blood when the disease starts, but about 1 in 20 people without rheumatoid arthritis also test positive.
A related blood test known as anti-cyclic citrullinated peptide test is also available. Anti-CCPs are antibodies also produced by the immune system.
People who test positive for anti-CCP are very likely to develop rheumatoid arthritis, but not everybody with rheumatoid arthritis has this antibody.
Those who test positive for both rheumatoid factor and anti-CCP may be more likely to have severe rheumatoid arthritis requiring higher levels of treatment.
You May Like: Does Vicks Vapor Rub Help With Arthritis
Are People With Rheumatoid Arthritis At Greater Risk For Covid
Yes, but this is an ongoing area of research. Its believed that autoimmune and inflammatory rheumatic disease patients are at higher risk for being hospitalized due to COVID-19 and having worse outcomes compared to the general population, according to the ACR.
However, this is likely affected by factors such as age, other comorbidities such as heart or lung disease, which is common in RA, and taking steroid medications, rather than simply having RA alone.
The medical community does consider patients living with rheumatoid arthritis to be at a greater risk for COVID-19, based on their inflammatory response from their condition, says Dr. Cadet. The medications used to treat the disease can also suppress the immune system.
In other words, when your body is preoccupied by fighting its own cells, it doesnt attack invaders as well as it should. Medications that affect immune system function can also affect the bodys ability to fight off viruses like the coronavirus.
For more information, check out this summary of research on inflammatory arthritis and rheumatic disease patients and their risk for COVID-19 complications.
Are Test Results Accurate
Rheumatoid factor testing is an important aspect of diagnosing certain health conditions and is generally regarded as accurate. Like any medical test though, RF testing is not perfect. Issues may arise in the processing or analysis of test samples and laboratories take special precautions to reduce the incidence of errors.
In order to reduce the likelihood of false positive results, in which a person tests positive for RF but doesnt have an underlying health condition, doctors may restrict RF testing to those with a high probability of having rheumatoid arthritis. In patients who arent likely to have rheumatoid arthritis based on their history and physical exam, the value of RF is poor, and false positives are more likely to occur.
Recommended Reading: How Do I Know If I Have Knee Arthritis
How To Prepare For An Initial Doctors Appointment
During your first appointment, your doctor will conduct a physical exam, collect details about your medical history, and discuss which symptoms you may be experiencing.
Generally, they will evaluate your joints for inflammation, swelling, and redness and may order imaging tests or blood work to determine if you have RA.
Be sure to keep track of all your symptoms and consider logging the time, duration, and severity of each symptom as it occurs. You should also provide your doctor with information about any medications that you are taking, including the frequency and dosage.
Keep in mind that you may not receive a definitive diagnosis on your first visit, as many autoimmune disorders develop slowly over time.
However, your doctor may discuss possible treatment options with you, which can include medications, physical therapy, pain management, exercise, and other modifications to your diet and lifestyle.
Its important to discuss any questions you have regarding your treatment plan with your doctor. Some questions you may want to consider asking:
- What treatment options are right for me?
- What are the potential side effects from my treatment?
- What types of exercise would be beneficial? How often should I work out?
- Are there other ways to treat symptoms at home, such as by using a hot or cold compress?
- What options available for mental health support, if needed?
- Would I benefit from physical therapy, nutrition counseling, or other complementary treatments?
Blood Test For Rheumatoid Arthritis
- As in the lupus test, there is no clear cut preparation for the rheumatoid arthritis blood test. Stay clear of alcohol or related products.
- It is good to inform the doctor of all the supplements, medication, or anything that helps in managing your condition. The doctor may tell you to avoid taking food before the test.
- There are several rheumatoid arthritis blood tests that the doctor can order. That will depend on the clinical symptoms and the doctors suspicion.
- The doctor will prepare you as in the lupus procedure. When the blood samples are back from the laboratory, the doctor will interpret the negative or positive results.
- The anti-CCP blood test looks for an antibody with the same name. If it is more than 20 units per milliliter, you are at risk. Antinuclear antibody test usually checks for other autoimmune diseases.
- Other blood tests include C-reactive protein, erythrocyte sedimentation rate, HLA tissue typing, and rheumatoid factor. Two further blood tests check on the uric concentration.
- If there is a higher concentration of uric acid, you may have gout rather than rheumatoid arthritis.
- Rheumatoid arthritis blood tests can sometimes fall short of giving a conclusive diagnosis. This will cause the doctor to use some imaging diagnosis to check the joint condition. It is the doctor to decide which other methods to take.
Also Check: Is Tens Good For Arthritis
Blood Fluid And Tissue Tests For Arthritis
Checking blood, tissues and various body fluids help doctors diagnose and monitor arthritis.
Blood and other lab tests play a critical role in diagnosing and monitoring arthritis. When your doctor needs to confirm an arthritis diagnosis, monitor disease progress, check medication effectiveness or determine if medications are causing potentially dangerous but not evident side effects, lab tests are ordered.
Most tests require drawing and testing the blood, but some may involve testing urine, joint fluid or even small pieces of skin or muscle.
Diagnosing and Monitoring Disease Activity
If your doctor suspects you have inflammatory arthritis, these are the most common tests used to diagnose as well as monitor the disease:
Blood Tests
Other Lab Tests
- Skin biopsy A small piece of skin is removed by a doctor. Its usually done under local anesthetic. The sample is tested in a lab and the results help determine the presence of lupus, vasculitis and psoriatic arthritis.
- Muscle biopsy A doctor takes the tissue sample from a muscle with a biopsy needle. The sample is reviewed for signs of damage to muscle fibers to help confirm a diagnosis of polymyositis or vasculitis.
- Joint fluid tests A doctor removes a small amount of fluid from a joint to determine the presence of uric acid and diagnose gout.
Monitoring Medication Response and Side Effects
Checking for Comorbidities
Quick Links
Other Tests For Seropositive Rheumatoid Arthritis
Blood tests are not only used to detect RF and anti-CCP antibodies. They’re also used to reveal if you have:
- Anemia, or low red blood cell count, which occurs in up to half of people with RA
- A high erythrocyte sedimentation rate, also known as a sed or ESR rate, a crude measure of inflammation in your body
- High C-reactive protein levels, another marker of inflammation
Aside from blood tests, an X-ray can help your doctor determine the degree of destruction in your joints, but may only be useful when RA has progressed to a later phase.
Recommended Reading: How To Treat Arthritis In Lumbar Spine