What Is Reactive Arthritis
Reactive Arthritis is a form of autoimmune arthritis or joint inflammation, that occurs as a reaction to an infection elsewhere in the body. Inflammation is a characteristic reaction of tissues to injury or disease and is marked by swelling, redness, heat, and pain. Besides this joint inflammation, reactive arthritis is associated with two other symptoms: redness and inflammation of the eyes and inflammation of the urinary tract . These symptoms may occur alone, together, or not at all.
Reactive arthritis is a type of spondyloarthritis a group of disorders that can cause inflammation throughout the body, especially in the spine.
The symptoms of reactive arthritis usually last several months, although symptoms can return or develop into a long-term disease in a small percentage of people.
This information is provided by the National Institutes of Health Genetic and Rare Diseases Information Center .
Digestive Disorders And Psoriatic Arthritis
Did you know having psoriatic arthritis might also affect your gut?
A study published in Clinical Rheumatology found people with psoriatic arthritis are at risk for having the following conditions:
- Crohns disease, a chronic inflammatory bowel disease that affects the lining of the digestive tract
- Ulcerative colitis, a chronic inflammatory bowel disease that causes inflammation in the digestive tract
- Reflux esophagitis, a condition where inflammation damages the esophagus
- Peptic ulcer disease, a condition that causes painful sores or ulcers in the lining of the stomach or small intestine
Another study, published in JAMA Dermatology, revealed people with psoriasis were around 2 times more likely to develop Crohns and ulcerative colitis compared with the general population.
The authors concluded: These findings suggest that psoriasis is significantly associated with IBD. Gastroenterology consultation may be indicated when patients with psoriasis present with bowel symptoms.
Scientists believe that the same gene mutations that are associated with psoriasis may also be related to the gut disorders.
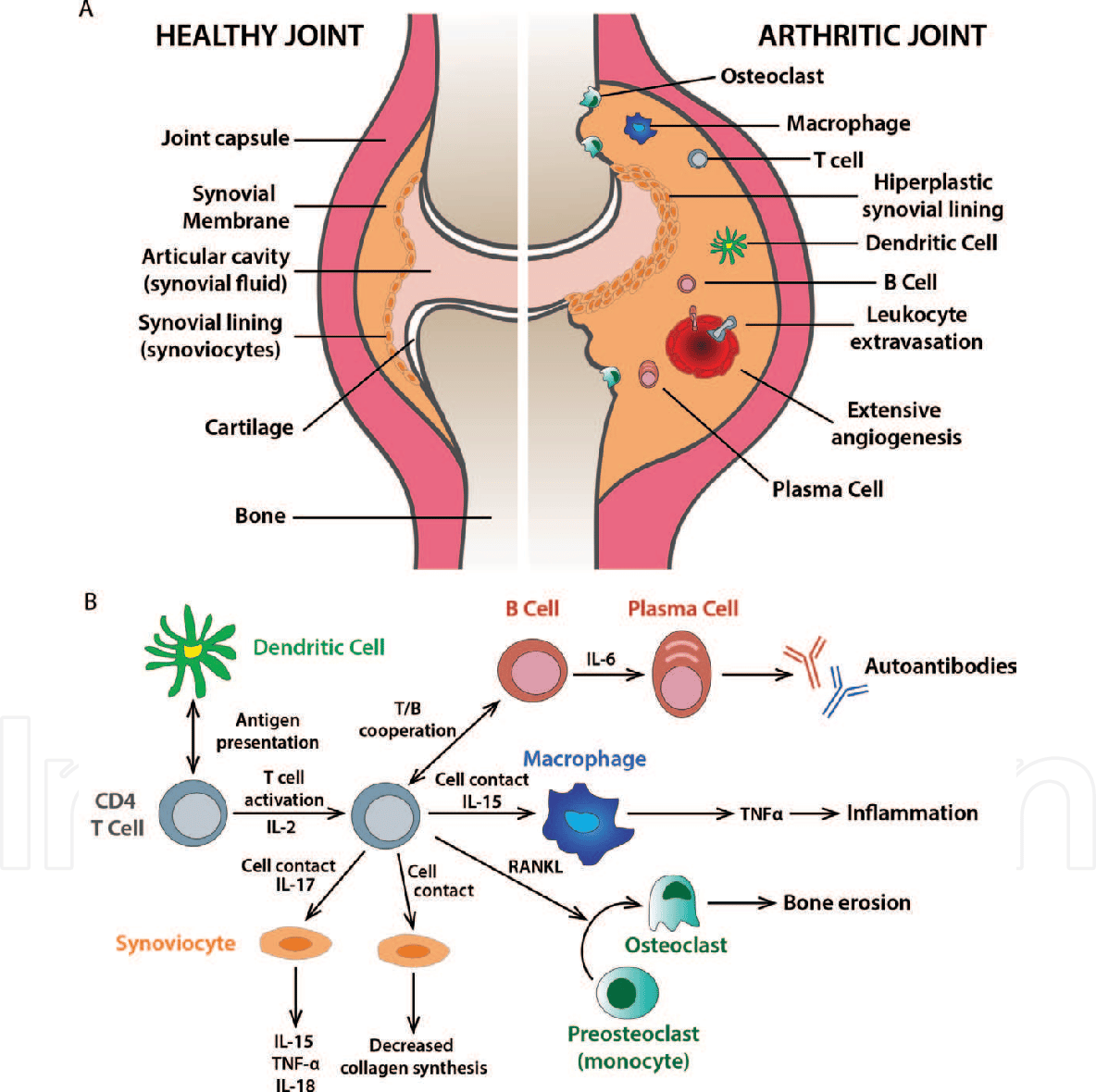
Causes Of Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disease. This means your immune system attacks the cells that line your joints by mistake, making the joints swollen, stiff and painful.
Over time, this can damage the joints, cartilage and nearby bone.
It’s not clear what triggers this problem with the immune system, although you’re at an increased risk if:
- you are a woman
- you have a family history of rheumatoid arthritis
Find out more about the causes of rheumatoid arthritis.
Read Also: Is Salt Bad For Arthritis
E How Do We Document And Evaluate Immune Deficiency Disorders Excluding Hiv Infection
1. General.
a. Immune deficiency disorders can be classified as:
Primary for example, X-linked agammaglobulinemia, thymic hypoplasia , severe combined immunodeficiency , chronic granulomatous disease , C1 esterase inhibitor deficiency.
Acquired for example, medication-related.
b. Primary immune deficiency disorders are seen mainly in children. However, recent advances in the treatment of these disorders have allowed many affected children to survive well into adulthood. Occasionally, these disorders are first diagnosed in adolescence or adulthood.
2. Documentation of immune deficiency disorders. The medical evidence must include documentation of the specific type of immune deficiency. Documentation may be by laboratory evidence or by other generally acceptable methods consistent with the prevailing state of medical knowledge and clinical practice.
3. Immune deficiency disorders treated by stem cell transplantation.
a. Evaluation in the first 12 months. If you undergo stem cell transplantation for your immune deficiency disorder, we will consider you disabled until at least 12 months from the date of the transplant.
b. Evaluation after the 12-month period has elapsed. After the 12-month period has elapsed, we will consider any residuals of your immune deficiency disorder as well as any residual impairment resulting from the treatment, such as complications arising from:
Graft-versus-host disease.
You May Like: Is Osteo Bi Flex Good For Rheumatoid Arthritis
Treatments For Inflammatory Arthritis
Although presently there is no cure for Inflammatory Arthritis, doctors and other healthcare providers can make lifestyle recommendations and prescribe medication that aim to control the inflammatory process and hence reduce its symptoms and signs. In patients in whom the process is well controlled, the progress and potential damage resulting from the disease can be slowed and often halted. Treatment is most effective when it begins early in the course of the disease. Over the past two decades, research in this field has resulted in dramatic improvements in care. Recent developments in treatment strategies have also significantly improved the long term outcomes of inflammatory arthritis.
Medications for Inflammatory Arthritis fall into one of the following categories:
Because the medications used to treat inflammatory arthritis affect the immune system and can have side effects, rheumatologists monitor their patients carefully throughout treatment. This can involve regular doctors visits and blood tests.
In addition to treatment with medication, people with inflammatory arthritis benefit from eating a healthy, balanced diet and maintaining an optimal weight to minimize stress on the joints.
Recommended Reading: How Can You Stop Arthritis In Your Hands
Recommended Reading: What’s The Best Pain Reliever For Arthritis
Do You Need To Modify Psoriatic Arthritis Medications Before Or After Getting The Vaccine
Temporarily stopping certain immunosuppressant medications after receiving the vaccine, or timing when you get the vaccine in the course of your treatment, might help increase the effectiveness of the COVID-19 vaccine if you have PsA.
But this only applies to a select few psoriatic arthritis medications. It is recommended, in most cases, that PsA patients who are to receive a COVID-19 vaccine continue their biologic or oral therapies for psoriatic arthritis, says Dr. Gupta.
The American College of Rheumatology and National Psoriasis Foundation guidance differs on this matter, which is why its important to discuss this with your doctor and make a decision thats right for your situation.
Here are the psoriatic arthritis drugs for which the ACR guidance suggests changes may be recommended:
- Methotrexate: Skip for 1 week after each vaccine dose
- JAK inhibitor : Skip for 1 week after each vaccine dose
- Abatacept , injectable form: Skip one week before and after the first vaccine dose only
- Abatacept , IV form: Get COVID-19 vaccine 4 weeks after your last infusion, then skip a week and get next infusion
The NPF guidance recommends that patients continue their biologic or oral therapies for psoriatic arthritis in most cases. For the Johnson & Johnson COVID-19 vaccine, which is only one dose, the guidance says that certain patients can consider holding methotrexate for two weeks after getting the vaccine:
Also Check: How Do You Fix Arthritis In The Knee
What Can Go Wrong With Your Immune System
When your immune system doesn’t work the way it should, it is called an immune system disorder. You may:
-
Be born with a weak immune system. This is called primary immune deficiency.
-
Get a disease that weakens your immune system. This is called acquired immune deficiency.
-
Have an immune system that is too active. This may happen with an allergic reaction.
-
Have an immune system that turns against you. This is called autoimmune disease.
Recommended Reading: How Do Doctors Know If You Have Rheumatoid Arthritis
What Are Newer Rheumatoid Arthritis Medications And Side Effects
Newer second-line drugs for the treatment of rheumatoid arthritis include the following:
Each of these medicines can increase the risk for infections, and the development of any infections should be reported to the doctor when taking these newer second-line drugs.
While biologic drugs are often combined with DMARDs in the treatment of RA, they are generally not used with other biologics due to the risk of serious infections. Similarly, JAK inhibitor medication is not used with traditional biologic medicines.
Does Rheumatoid Arthritis Cause Fatigue
Everyones experience of rheumatoid arthritis is a little different. But many people with RA say that fatigue is among the worst symptoms of the disease.
Living with chronic pain can be exhausting. And fatigue can make it more difficult to manage your pain. Its important to pay attention to your body and take breaks before you get too tired.
What are rheumatoid arthritis flare symptoms?
The symptoms of a rheumatoid arthritis flare arent much different from the symptoms of rheumatoid arthritis. But people with RA have ups and downs. A flare is a time when you have significant symptoms after feeling better for a while. With treatment, youll likely have periods of time when you feel better. Then, stress, changes in weather, certain foods or infections trigger a period of increased disease activity.
Although you cant prevent flares altogether, there are steps you can take to help you manage them. It might help to write your symptoms down every day in a journal, along with whats going on in your life. Share this journal with your rheumatologist, who may help you identify triggers. Then you can work to manage those triggers.
Read Also: Does Exercise Help Rheumatoid Arthritis
Disorders Of The Immune System
Your immune system is your bodys defense against infections and other harmful invaders. Without it, you would constantly get sick from bacteria or viruses.
Your immune system is made up of special cells, tissues, and organs that work together to protect you.
The lymph, or lymphatic, system is a major part of the immune system. It’s a network of lymph nodes and vessels. Lymphatic vessels are thin tubes that branch, like blood vessels, throughout the body. They carry a clear fluid called lymph. Lymph contains tissue fluid, waste products, and immune system cells. Lymph nodes are small, bean-shaped clumps of immune system cells that are connected by lymphatic vessels. They contain white blood cells that trap viruses, bacteria, and other invaders, including cancer cells.
White blood cells are the cells of the immune system. They are made in one of your lymph organs, the bone marrow. Other lymph organs include the spleen and thymus.
What Is The Difference Between Rheumatoid Arthritis And Osteoarthritis
Rheumatoid arthritis and osteoarthritis both cause joint pain, stiffness, and limited range of motion, but the two diseases are distinct in their root cause and treatment.
Rheumatoid arthritis is an autoimmune condition where a persons own immune system attacks their joints, causing inflammation. Rheumatoid arthritis typically affects many joints simultaneously, especially in the hands, wrists, and feet, and is treated with medications to suppress the immune response.
Osteoarthritis is not an autoimmune disease, and although the exact causes are not known, multiple risk factors have been identified. In a healthy joint, cartilage provides cushioning and a smooth joint surface for motion. In an osteoarthritic joint, as cartilage is irreversibly destroyed and bone abnormalities develop, movement becomes painful and more difficult.
Recommended Reading: Is Egg Bad For Arthritis
Common Autoimmune Disease Symptoms
Despite the varying types of autoimmune disease, many of them share similar symptoms. Common symptoms of autoimmune disease include:
- Abdominal pain or digestive issues
- Recurring fever
Many women say its hard to get diagnosed, something that Orbai agrees with. Its not black or white, she says. Theres usually no single test to diagnose autoimmune disease. You have to have certain symptoms combined with specific blood markers and in some cases, even a tissue biopsy. Its not just one factor.
Diagnosis can also be difficult because these symptoms can come from other common conditions. Orbai says women should seek treatment when they notice new symptoms.
If youve been healthy and suddenly you feel fatigue or joint stiffness, dont downplay that, she says. Telling your doctor helps him or her to look closer at your symptoms and run tests to either identify or rule out autoimmune disease.
Risk Factors And Prevalence

Psoriasis, a family history of PsA, being between 30 and 50 years of age, cigarette smoking, obesity, having the HLA-B gene and other genetic markers, being male, and environmental triggers .
Dykes, L. . Females at Greater Risk of Developing Psoriatic Arthritis in Recent Years. Rheumatology Network. .
Feintuch, S. . 11 Psoriatic Arthritis Complications You Need to Know About. CreakyJoints. .
Feintuch, S. . Psoriatic Arthritis Risk Factors and Causes You Need to Know About. CreakyJoints. .
Haddad, A., & Zisman, D. . Comorbidities in Patients with Psoriatic Arthritis. Rambam Maimonides medical journal, 8, e0004. .
You May Like: Why Do You Get Arthritis In Your Back
F How Do We Document And Evaluate Hiv Infection
Any individual with HIV infection, including one with a diagnosis of acquired immune deficiency syndrome , may be found disabled under 14.11 if his or her impairment meets the criteria in that listing or is medically equivalent to the criteria in that listing.
1. Documentation of HIV infection.
a. Definitive documentation of HIV infection. We may document a diagnosis of HIV infection by positive findings on one or more of the following definitive laboratory tests:
HIV antibody screening test , confirmed by a supplemental HIV antibody test such as the Western blot , an immunofluorescence assay, or an HIV-1/HIV-2 antibody differentiation immunoassay.
HIV nucleic acid detection test .
HIV p24 antigen test.
Isolation of HIV in viral culture.
Other tests that are highly specific for detection of HIV and that are consistent with the prevailing state of medical knowledge.
b. We will make every reasonable effort to obtain the results of your laboratory testing. Pursuant to §§ 404.1519f and 416.919f, we will purchase examinations or tests necessary to make a determination in your claim if no other acceptable documentation exists.
c. Other acceptable documentation of HIV infection. We may also document HIV infection without definitive laboratory evidence.
2. Documentation of the manifestations of HIV infection.
c. Other acceptable documentation of manifestations of HIV infection. We may also document manifestations of HIV infection without definitive laboratory evidence.
How Can Parents Help
JIA is a lifelong disease, but treatments can help ease pain, keep kids active, and prevent long-term joint damage. To help your child:
- Make sure your child takes all medicines exactly as directed.
- Work with your childs physical therapist to develop a regular exercise program. This will help keep your childs muscles strong and flexible.
- Learn about JIA with your child. Your care team is a great resource. You can also find information and support online at:
Read Also: What Foods Are Good For Arthritis Pain
What Causes Rheumatoid Arthritis
The exact cause of rheumatoid arthritis is unknown. Researchers think its caused by a combination of genetics, hormones and environmental factors.
Normally, your immune system protects your body from disease. With rheumatoid arthritis, something triggers your immune system to attack your joints. An infection, smoking or physical or emotional stress may be triggering.
Is rheumatoid arthritis genetic?
Scientists have studied many genes as potential risk factors for RA. Certain genetic variations and non-genetic factors contribute to your risk of developing rheumatoid arthritis. Non-genetic factors include sex and exposure to irritants and pollutants.
People born with variations in the human leukocyte antigen genes are more likely to develop rheumatoid arthritis. HLA genes help your immune system tell the difference between proteins your body makes and proteins from invaders like viruses and bacteria.
What Causes Autoimmune Diseases
No one is sure why autoimmune diseases happen. But you can’t catch them from other people.
Autoimmune diseases do tend to run in families, which means that certain genes may make some people more likely to develop a problem. Viruses, certain chemicals, and other things in the environment may trigger an autoimmune disease if you already have the genes for it.
Also Check: How Can I Relieve Arthritis Pain In My Hands
Is Osteoarthritis An Autoimmune Disease
Arthritis has several types, and osteoarthritis or OA is the most common type. According to a classic theory, OA is related to a condition of when the cartilage degenerates and breaks down as the age. In fact, it is more common to be found in people aged 45 or older. But is it also a kind of autoimmune disease?
Understanding autoimmune diseases in general!
Autoimmune disease is a condition of when the immune system of the body doesnt work as well as it should. And there are numerous different types of this disease.
Normally, the immune system is so essential to protect the body from harmful substances called antigens such as harmful virus and bacteria. But in autoimmune disorder, the immune system works abnormally .
There are some theories proposed, but currently nobody knows exactly the reason behind autoimmune disorder.
The abnormality of immune system may cause:
In other words, the abnormal function of immune system can affect other organs of the body. Skin, muscles, pancreas, thyroid, blood vessels, connective tissues, joints , and red blood cells are common organs affected in autoimmune disorder.
The symptoms that appear if you have this disease are dependent on the kind of the autoimmune disorder itself and the affected organ . But in general malaise , fever, and fatigue are usually the common symptoms.
Osteoarthritis is not an autoimmune disease!
Genetic And Epigenetic Findings Of Autoimmunity In Psa
2.1.1. Human leukocyte antigen associations
Given their strong risk association, explaining the functional role of the HLA risk alleles, particularly the HLA-C*06:02, is essential for elucidating the pathogenesis of PsA. A fascinating case study with a unique methodology identified ADAMTS-like 5 as an HLA-C*06:02-presented melanocytic autoantigen to the lesion-infiltrating autoreactive CD8+ T cells in psoriasis . More interestingly, peptide motifs of the HLA-C*07:01, -C*07:02, and -B*27, which are three of the other psoriasis risk-related leukocyte antigens, utilize the same anchor residues with the HLA-C*06:02, have overlapping peptide-binding properties, and belong to the same HLA supertype . Synovial/entheseal counterpart of this picture is yet to be studied but seems to be more complicated since different disease phenotypes in PsA exhibit different HLA associations and contribution of the HLA-C*06:02 polymorphism to PsA risk is lesser compared to psoriasis .
Read Also: What Helps Arthritis Pain In Ankle
You May Like: How To Reduce Rheumatoid Arthritis Pain
What Are The Goals Of Treating Rheumatoid Arthritis
The most important goal of treating rheumatoid arthritis is to reduce joint pain and swelling. Doing so should help maintain or improve joint function. The long-term goal of treatment is to slow or stop joint damage. Controlling joint inflammation reduces your pain and improves your quality of life.