What Are The Symptoms Of Osteoarthritis
The main symptoms of osteoarthritis are:
- joint pain and stiffness
- grating sensations when moving a joint
- less joint flexibility than before
You may only notice symptoms in your joints after doing an activity such as walking, climbing stairs or opening a jar. Some people have mild symptoms, while others may experience more severe, ongoing symptoms.
Who Gets Osteoarthritis Of The Knee
Osteoarthritis is the most common type of arthritis. While it can occur even in young people, the chance of developing osteoarthritis rises after age 45. According to the Arthritis Foundation, more than 27 million people in the U.S. have osteoarthritis, with the knee being one of the most commonly affected areas. Women are more likely to have osteoarthritis than men.
What Should I Expect From A Knee Osteotomy
Youll have knee osteotomy under anesthesia. Your doctor will recommend the best anesthesia option for you, including:
- General anesthesia: Your doctor gives you medicine that puts you to sleep during the surgery.
- Spinal anesthesia: You receive an injection in your back that numbs your body from the waist down.
Your doctor has several options to hold the osteotomy in place during healing. This includes metal screws and a plate or a biocomposite material to hold the realigned bone in place while it heals. Knee osteotomy surgery usually takes one to two hours.
After a knee osteotomy, your doctor will closely monitor you while you recover from the anesthesia. Most people who have a knee osteotomy leave the hospital one to two days after surgery. Some patients leave the same day of surgery. While healing from the surgery, you will likely need to use crutches or a walker for several weeks to avoid putting too much weight on the knee while it heals.
Don’t Miss: What Is Infusion Therapy For Rheumatoid Arthritis
Preparing For Your Appointment
Communicating openly with your doctor and collaborating on your care is important. Your appointment is an opportunity to share your symptoms, ask your questions, and discuss your treatment plan. Doctors are offering patients the option to schedule in-office or virtual visits. These tips may be helpful on your next appointmentwhether youll be at the doctors office or on your device.
Recommended Reading: Whats The Difference Between Osteoarthritis And Rheumatoid Arthritis
What Are The Risks Of Platelet

As with any type of injection, there are small risks of bleeding, pain and infection. When the platelets are from the patient who will be using them, the product is not expected to create allergies or have risks of cross infection. One of the main limitations with PRP products is that every preparation in every patient can be different. No two preparations are the same. Understanding the composition of these therapies required measuring numerous complex and different factors. This variation limits our understanding of when and how these therapies may succeed and fail, and the matter of current research endeavors.
Recommended Reading: What’s The Difference Between Rheumatoid And Psoriatic Arthritis
Treating Arthritis Of The Knee
What Is A Joint And How Does It Work
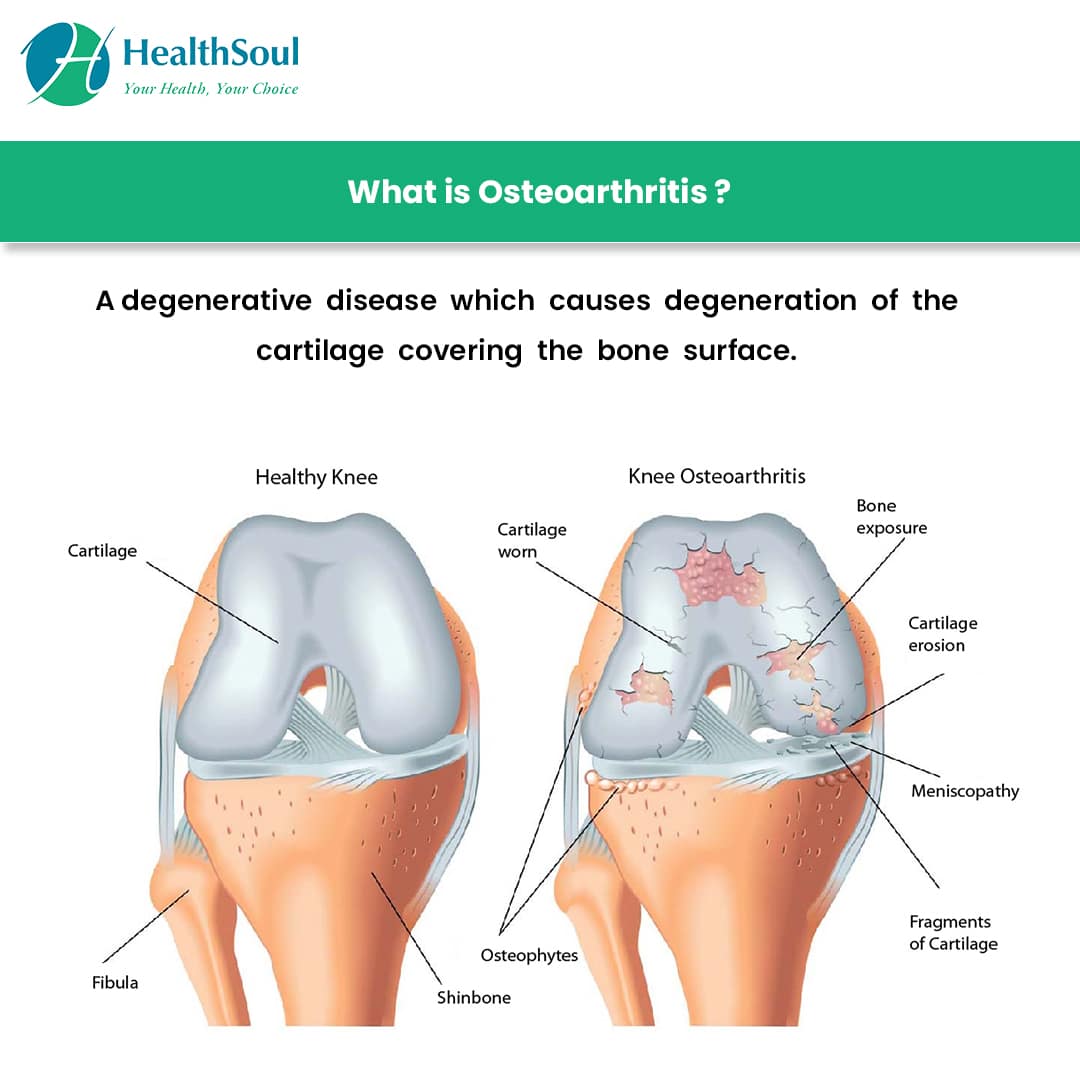
A joint is where two or more bones meet, such as in the fingers, knees, and shoulders. Joints hold bones in place and allow them to move freely within limits.
Most of the joints in our body are surrounded by a strong capsule. The capsule is filled with a thick fluid that helps to lubricate the joint. These capsules hold our bones in place. They do this with the help of ligaments. These are a bit like very strong elastic bands.
The ends of the bones within a joint are lined with cartilage. This is a smooth but tough layer of tissue that allows bones to glide over one another as you move.
If we want to move a bone, our brain gives a signal to the muscle, which then pulls a tendon, and this is attached to the bone. Muscles therefore have an important role in supporting a joint.
Also Check: Can Ms Be Misdiagnosed As Psoriatic Arthritis
How Can I Reduce My Risk For Post
Follow these general safety tips to reduce your risk of an injury:
- Always wear your seatbelt.
- Wear the right protective equipment for all activities and sports.
- Make sure your home and workspace are free from clutter that could trip you or others.
- Always use the proper tools or equipment at home to reach things. Never stand on chairs, tables or countertops.
What Happens During Knee Arthroscopy
During the procedure, your healthcare provider:
You May Like: Can Psoriatic Arthritis Affect The Lungs
What Are The Early Signs Of Arthritis In The Knees
Back to News
Arthritis is a disease characterized by pain, swelling, and joint stiffness. Notably, arthritis can affect various joints in your body although the knees are the most common culprit. Although there is no cure for knee arthritis, its essential to see an orthopedic knee surgeon to help slow the progression of this condition.
There are two common types of knee arthritis: rheumatoid arthritis and osteoarthritis .
OA is a progressive condition and usually occurs after midlife. This is due to the gradual wearing of the cartilage in the knee joint. You can also get post-traumatic arthritis which develops after a knee injury. Rheumatoid arthritis is an inflammatory autoimmune disease that can appear at any age.
Keep reading to learn about some early signs of knee-related arthritis:
Gradual Increase in Pain
Arthritis pain typically starts slow though it can appear suddenly in rare cases. During the early stages, you might experience pain in the morning or after long periods of inactivity. For instance, your knee might hurt when you suddenly stand up from a sitting position.
In the case of RA, you might experience pain in the smaller joints usually on both sides of the body. These symptoms might worsen during cold weather or after excessive activity.
Cracking Sounds
Another early sign of arthritis is hearing a popping sound when you bend or straighten your knee. Your orthopedic knee surgeon may refer to the phenomenon as crepitus.
- Physical activity
Cracking Or Popping Sounds
When you bend or straighten your knee, you may feel a grinding sensation or hear cracking or popping sounds. Doctors call this crepitus.
These symptoms can occur when youve lost some of the cartilage that helps with smooth range of motion. Both OA and RA can result in cartilage damage.
When cartilage is damaged, rough surfaces and bone spurs develop. As you move your joints, these irregular areas rub against each other.
Read Also: How To Test For Rheumatoid Arthritis Symptoms
What Can Knee Mri Diagnose
MRI is good at diagnosing sprains and tears of the tendons and ligaments.
We can see tears of the menisci of the knee.
MRI can show us sprains and tears of muscle around the knee.
We can see arthritis including the detailed location and extent of cartilage damage.
We can diagnose all types of abnormalities of the bone that X-rays sometimes do not show. These can include bone bruises, fractures, bone lesions and tumors.
MRI of the knee can show us collections of fluid around the knee. This can be joint fluid, fluid in a bursa, cysts, or swelling from various causes.
Will an MRI show knee inflammation?
Yes, knee inflammation can be seen on an MRI. This can be seen as edema or fluid accumulation around the knee. There are various causes of inflammation like arthritis, injuries, and infections.
Is Surgery Used To Treat Knee Osteoarthritis
If your doctor wants to treat the osteoarthritis in the knee with surgery, the options are arthroscopy, osteotomy, and arthroplasty.
- Arthroscopy uses a small telescope and other small instruments. The surgery is performed through small incisions. The surgeon uses the arthroscope to see into the joint space. Once there, the surgeon can remove damaged cartilage or loose particles, clean the bone surface, and repair other types of tissue if those damages are discovered. The procedure is often used on younger patients in order to delay more serious surgery.
- An osteotomy is a procedure that aims to make the knee alignment better by changing the shape of the bones. This type of surgery may be recommended if you have damage primarily in one area of the knee. It might also be recommended if you have broken your knee and it has not healed well. An osteotomy is not permanent, and further surgery may be necessary later on.
- Joint replacement surgery, or arthroplasty, is a surgical procedure in which joints are replaced with artificial parts made from metals or plastic. The replacement could involve one side of the knee or the entire knee. Joint replacement surgery is usually reserved for people over age 50 with severe osteoarthritis. The surgery may need to be repeated later if the prosthetic joint wears out after several years. But with today’s modern advancements, most new joints will last over 20 years. The surgery has risks, but the results are generally very good.
Read Also: Is Epsom Salt Good For Arthritis
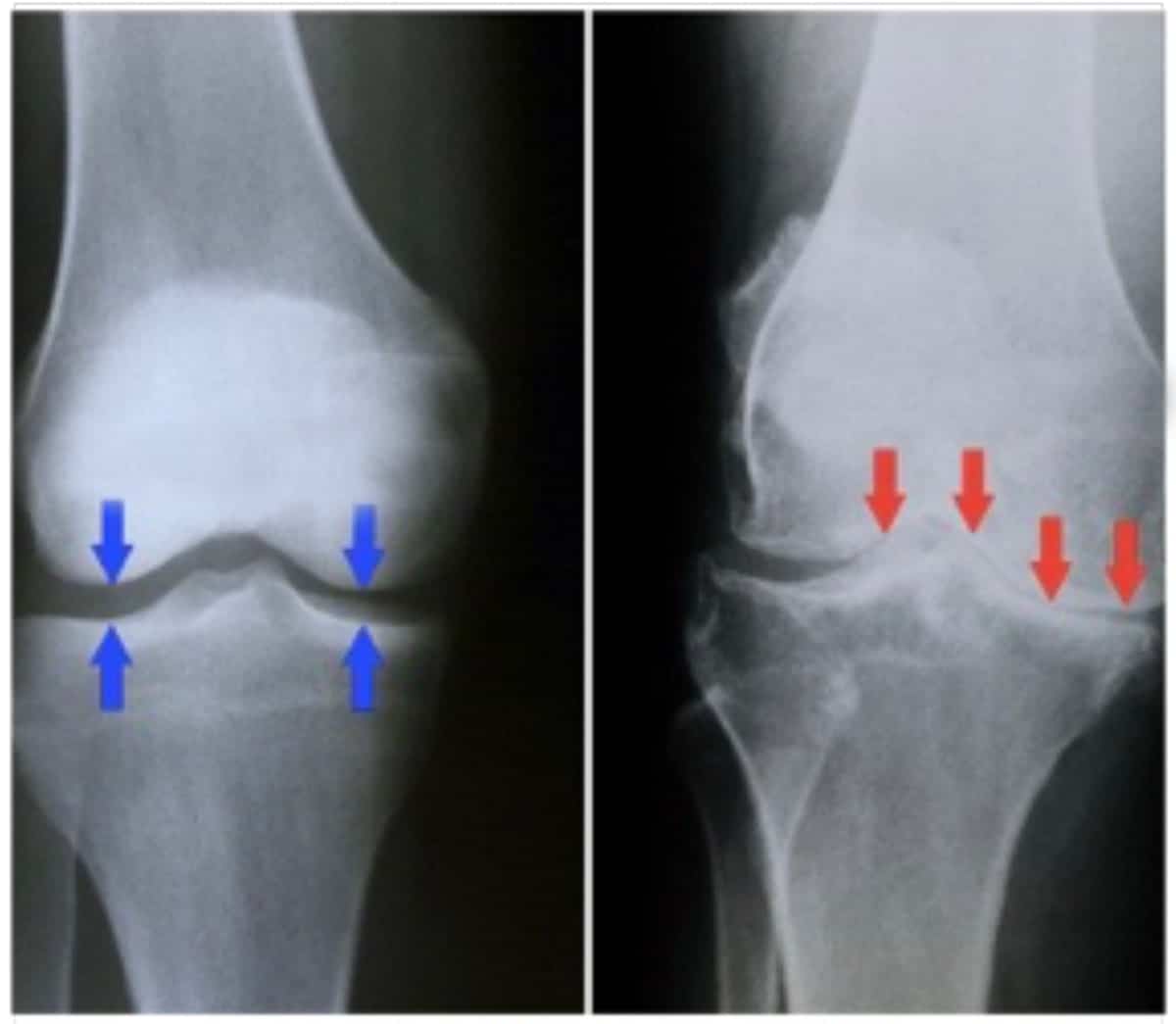
The Course Of Knee Oa And Factors Of Progression
A proportion of patients with knee OA have a progressive course. The rate of progression varies across the life stages based on the presence or absence of some associated factors. In the elderly persons, the rate of progression is low . In Framingham study, over a mean follow up period of 8.1 years, a progressive rate of 4% per year was observed among patients with knee OA. In another study of 32 patients with knee OA who were followed up for 2 years, about 6.1% of cartilage volume had lost over the study period. In this study, progression of knee OA was evident as early as six months after the start of the study .
Progression of OA may be attributed to the effects of biomechanical forces derived in response to pathological reactions. These factors can lead to progressive deterioration of joint structures and exacerbation of knee symptoms and subsequent reduction of knee joint functions.
Obesity, generalized OA, malalignment and synovitis have consistently been reported as associated factors of progression in knee OA . Malalignment of the knee joint was found to be an independent risk factor for the progression of knee OA . Varus and valgus malalignment increase the risk of medial and lateral osteoarthritis progression, respectively. This was shown in a systematic review of 14 studies .
How Common Is Osteoarthritis
Women are more likely to develop osteoarthritis than men. Australian studies show that about 1 in 10 women report having the condition, compared with about 1 in 16 men.
Osteoarthritis can develop at any age, but it is more common in people aged over 40 years or in those who have previously injured a joint. One in 5 Australians over the age of 45, and one in 3 over 75 years have osteoarthritis.
Read Also: What’s The Best Thing For Arthritis
When Can I Go Back To My Usual Activities After Knee Arthroscopy
Everyone responds to surgery differently. Ask your healthcare provider when you can get back to your daily activities, including driving and walking without assistance. Your healthcare provider may recommend waiting several weeks before doing more physical or strenuous activities.
Sometimes, people need to make changes to their lifestyle and activity level. Some sports can damage your knee. Talk to your healthcare provider about choosing lower-impact sports and activities that are easier on your knee.
What Is Knee Arthroscopy
Healthcare providers use knee arthroscopy to diagnose and treat a wide range of knee injuries. During arthroscopic knee surgery, your healthcare provider inserts a tiny camera through an incision. The camera shows the inside of your knee. The images appear on a screen in the operating room. They help your healthcare provider diagnose problems inside of your knee.
Knee arthroscopy is a very common minimally invasive surgical procedure. Minimally invasive procedures require smaller incisions than traditional surgery. The incisions are about the size of a keyhole.
To treat injuries or structural problems, your healthcare provider inserts tiny tools through another incision. They use the tools to repair or remove damaged tissue.
Also Check: Can You Donate Blood If You Have Rheumatoid Arthritis
Dealing With Knee Arthritis At Home
What Is A Knee Osteotomy
A knee osteotomy is an operation that surgeons use to treat the pain and instability that can occur when there is damage or arthritis in part of the knee joint. Doctors may recommend an osteotomy instead of a knee replacement when only one area of the knee has damage.
During this knee surgery, a surgeon repositions the bones in the tibia or femur to realign the knee. This new positioning shifts your body weight from the damaged part of your knee to a healthy part.
A knee osteotomy can help slow deterioration of cartilage in the knee and may delay your need for knee replacement surgery for many years. Osteotomy of the knee has been used for decades to improve pain and function.
Read Also: How Do I Stop Arthritis
When To See A Doctor
Aches or pains that last a day or two generally arent cause for concern. But you should let your doctor know if youre experiencing persistent joint pain, stiffness, or swelling, or if youre experiencing joint symptoms that are getting in the way of your everyday activities. Rheumatoid arthritis needs to be treated early in order to stave off permanent joint damage. And regardless of your arthritis type, getting care sooner can help you feel better.
Related Story
Impaired Quality Of Life
People with symptomatic knee osteoarthritis may have problems performing their daily activities. This is often a direct consequence of intense knee pain and limited range of motion.
The daily life of a knee OA patient can get extremely difficult, sometimes to the point where no treatments can relieve pain.
This can trigger or exacerbate feelings of anxiety and depression in patients with this chronic disease, making their daily lives even more difficult.
Don’t Miss: Does Warm Weather Help Arthritis
Gradual Knee Joint Pain
The pain from knee osteoarthritis tends to have a gradual onset, rather than happening from one day to the next.
It often gets worse with movement like climbing stairs, squatting, or walking. Yet, it can also be present at rest, mostly while sitting or standing for long periods.
As the cartilage deterioration advances, you could have intense pain at night, too. However, the type of pain will vary from person to person.
It could feel like a dull, intermittent pain around your whole knee joint throughout the day. Or a sharp, severe pain that appears in specific movements.
Learn more:Reasons why knee osteoarthritis pain worsens at night.