Sleep Easy With Rheumatoid Arthritis
Are achy joints, stiffness, and night sweats interrupting your sleep? Try these tips for managing insomnia and other sleep problems related to RA.
People with chronic pain, a hallmark of rheumatoid arthritis, need quality sleep. In fact, a survey of 971 adults revealed that those who got fewer than six hours of sleep a night were more likely to report troublesome pain the next day. And the poor sleep-daytime pain connection may be a vicious cycle other studies have shown that people who report high levels of daytime pain have a harder time sleeping well that night.
If you have rheumatoid arthritis, chances are you contend with chronic or periodic pain, stiffness, and achiness that can wake you up at night, interfering with good quality sleep and leading to insomnia. Both your sleepless nights and painful days need to be addressed in order to improve quality of life. Fortunately, addressing one could also improve the other.
When Rheumatoid Arthritis Pain Disrupts Sleep
When Debbi Hirshfield, of Springfield, Mass., was diagnosed with rheumatoid arthritis, getting a good nights sleep became a problem so she decided to buy a new bed.
The store she went to provided a computer-based diagnosis of her bodys pressure points when lying on a mattress and then recommended an appropriate product. I was more comfortable the moment I got into bed, recalls Hirshfield.
Here are a few other tricks that have been helpful:
Ruthberg offer these tips as well:
Morphologic Examination Of The Lymph Node
The diagnostic test consisted of an excisional biopsy of a cervical lymph node. Examination of the node revealed patchy, irregular paracortical lesions composed of mononuclear cells associated with remarkable karyorrhectic debris . The mononuclear cells included phagocytic macrophages , histiocytes, lymphocytes, and so-called plasmacytoid monocytes, now known to represent a population of immature dendritic cells. Neither neutrophils nor eosinophils were present in significant quantities. The cortical portion of the lymph node was markedly attenuated without reactive lymphoid follicles.
Figure 3
How Should I Take Venlafaxine Extended
You should take venlafaxine extended-release with food.
You should take venlafaxine extended-release exactly as prescribed, and continue to take venlafaxine extended-release as prescribed even after your symptoms improve. You should not change your dosing regimen or stop taking venlafaxine extended-release without discussing with your provider first. A gradual reduction in dosage rather than abruptly stopping is recommended whenever possible.
If your symptoms are not improving or you have any questions about changing or stopping medication, reach out to your Ro-affiliated provider for guidance.
Don’t Miss: Coping With Rheumatoid Arthritis
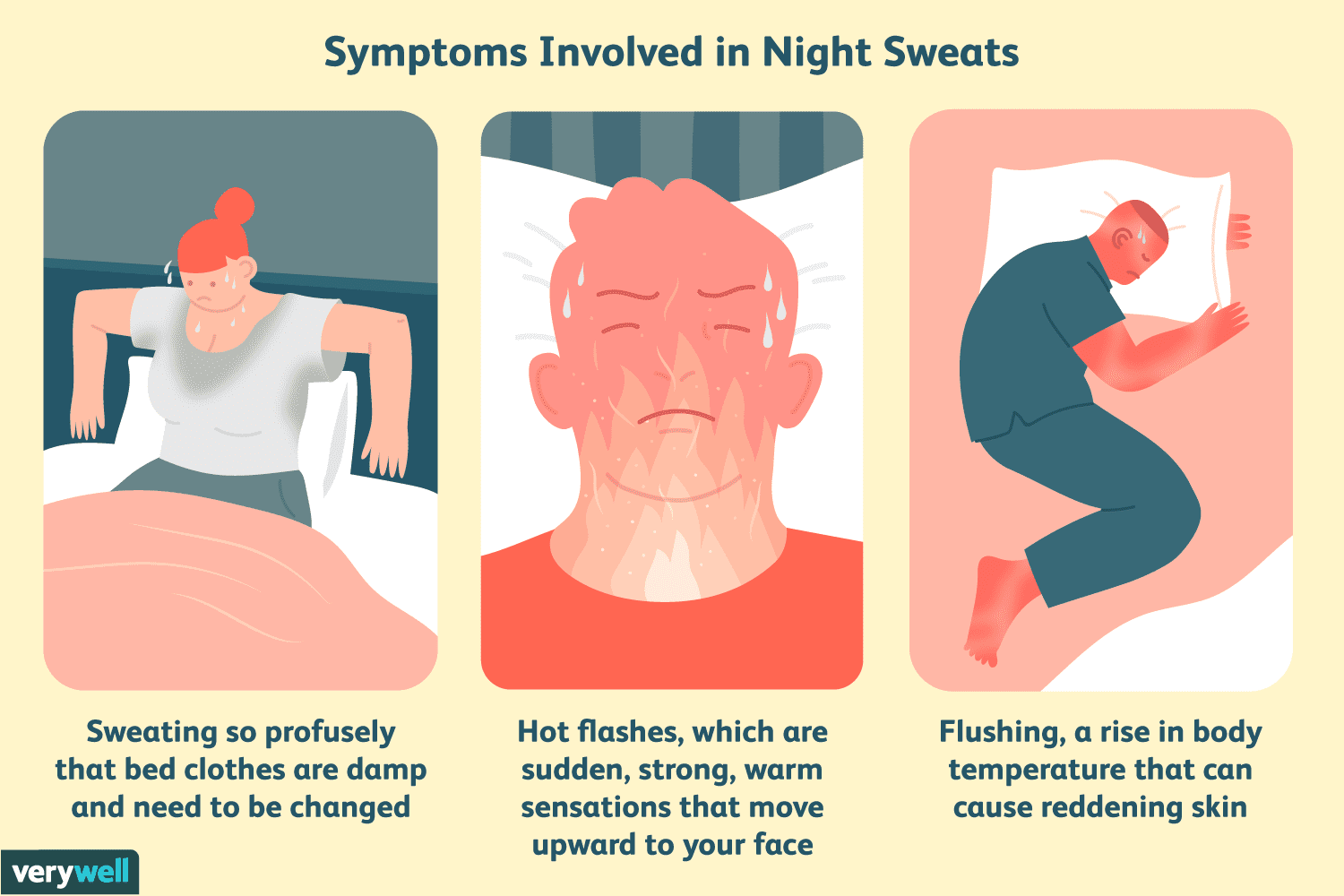
How To Diagnose The Cause Of Night Sweats
Diagnosis of night sweats begins with a discussion with your healthcare provider about the severity, frequency, and any associated symptoms you may have with your night sweats. A physical exam may further narrow down potential causes to allow for a more focused work-up. As mentioned above, night sweats can be a symptom of an underlying medical condition, and your provider will look for other symptoms like hot flashes, abnormal periods, fevers, cough, unexplained weight loss, heartburn, and snoring. Tell your provider if you have a history of medical conditions like diabetes, HIV, substance abuse, obstructive sleep apnea, hyperthyroidism, or anxiety disorders. In some cases, additional testing like bloodwork or chest x-rays may be indicated.
Who Should Not Use Venlafaxine Extended

Do not use venlafaxine extended-release if:
- You are taking a class of medications called monoamine oxidase inhibitors . Examples of MAOIs include isocarboxazid , phenelzine , selegiline , and tranylcypromine , linezolid, or intravenous methylene blue. MAOIs may increase the risk of serotonin syndrome.
- You have a known allergic reaction to venlafaxine hydrochloride or desvenlafaxine succinate.
You May Like: How To Relieve Arthritis Pain In Your Hands
Parkinsons Disease And Drenching Night Sweats Solutions
PatientsLikeMe members with Parkinsons disease have talked a lot about excessive sweating and heat intolerance with Parkinsons disease. It can be a stinker, as one blogger who has PD recently shared in Parkinsons News Today.
Can you relate? Read on for more information and some possible adjustments or life hacks that others have tried.
One study found that over 60% of patients with PD experience sweating disturbances like hyperhidrosis or hypohydrosis .
The Parkinsons Foundation and Parkinsons Victoria cover these issues in their guides to skin, scalp and sweat changes related to PD. In addition to hyperhidrosis, many people with PD experience an extra-oily scalp , drenching night sweats and general difficulty with temperature control.
Some of these problems may stem from PD itself, which affects some of the bodys automatic functions, such as blood pressure and temperature regulation.
Research has shown that hyperhidrosis also seems to occur along with off times in levodopa treatment and with dyskinesia .
Possible solutions and hacks
Maria De Leon, M.D., a neurologist with young onset PD, writes on her blog that she understands firsthand the impact that sweating issues can have on peoples lives. A few things you can try? Dr. De Leon suggests:
Join PatientsLikeMe to see what the community says about excessive sweating and heat intolerance with PD, or add a comment below based on your own experiences.
Stomach Pain Or Indigestion
RA and medicines used to treat it are linked to mouth and stomach ulcers, stomach bleeding, acid reflux, diarrhea, and constipation. Painful diverticulitis and colitis are also possible if you have RA.
RA drugs like NSAIDs often cause ulcers or an upset stomach.
Belly pain is sometimes a sign of a rare RA complication called rheumatoid vasculitis — when inflammation spreads to your blood vessels. Weight loss and lack of appetite are other symptoms. Vasculitis is serious, so see a doctor right away. Learn more about vasculitis symptoms and types.
Recommended Reading: Rheumatoid Arthritis Pain Worse At Night
Highlights Of Pharmacologic Therapy
Monitoring for therapeutic benefit and toxicity is required for the duration of treatment.2TABLE 1 outlines the specific agents in the pharmacologic categories discussed below. While beyond the scope of this article, a comprehensive discussion about the pharmacologic management of RA may be found in References 1 , 2, 10, and individual manufacturer’s guidelines for each agent.1,2,10
Disease-modifying antirheumatic drugs are indicated in almost all RA patients since they appear to slow the progression of the disease.1 DMARDs vary chemically and pharmacologically from one another and no one agent is safe and efficacious in every patient.1,11 The ultimate goal is the prevention of erosions and progressive deformity, so DMARDs should be initiated within 3 months of diagnosis.2 Use in combination with one another may be more effective than monotherapy in some cases, a DMARD plus a biologic agent may be used to achieve a therapeutic outcome.1,2 MTX is the most commonly prescribed DMARD in the U.S. many rheumatologists consider it the drug of choice for managing RA.2,8 Toxicity to MTX, or any immunosuppressive agent, is increased in the elderly.10 Penicillamine, gold compounds, and the cytotoxic, immunosuppressive, or immunomodulatory agentsare used less frequently today due to toxicity and/or lack of long-term benefit, especially in the elderly, although they may have clinical value.8
Osteoarthritis And Rheumatoid Arthritis: Whats The Difference
OA and RA do bear some symptomatic similarities. Both conditions result in severe joint pain, swelling and stiffness. However the causes of these conditions are very different.
RA is an inflammatory autoimmune disease that affects the joints. Ailsa explains. The immune system goes wrong and attacks you instead of protecting you. It is very different to osteoarthritis. Its a systemic disease, and can affect other organs such as the eyes, lungs and heart. Having another autoimmune condition is relatively common and RA can occur with anemia, IBS, Crohns and colitis, Sjögrens syndrome, secondary Sjögrens syndrome or uveitis.
So who is more likely to be diagnosed with rheumatoid arthritis?
Whereas osteoarthritis is a wear and tear condition and generally affects many older people rheumatoid arthritis can affect anyone over the age of 16 at any point in their lives. RA is most commonly diagnosed between the ages of 40 and 60 years. Females are at a higher risk of being diagnosed. It is not fully understood why, but the disease affects about three times as many women as it does men.
Recommended Reading: How To Deal With Arthritis
Other Causes Of Joint Pain
Neurologic causes of pain may be determined by characterization apart from numbness and burning pain, the pain is unlikely to worsen with joint movement and is likely to worsen at night. Combinations of causes might make characterization of pain difficult. For example, a neurologic cause of pain might be combined with a rheumatologic cause, leading to mixed characteristics.
Extra-articular symptoms can help narrow the diagnostic options. For example, weakness may be a sign of neuromuscular disease, whereas dry mouth, dry eyes, Raynaud phenomenon, pleuritic chest pain, nasal ulcers, oral ulcers, alopecia, adenopathy, or rash might suggest systemic inflammatory rheumatologic conditions. Constitutional symptoms such as weight loss, night sweats, fever, and fatigue are also more common with systemic illnesses.
What The Hot Feeling Feels Like
We were first tuned into this symptom by CreakyJoints member Frances D., who has psoriatic arthritis. When she posted about it on , she got a ton of responses from fellow patients. I feel hotter than most people constantly, she told us when we asked her more about it. Sometimes at night I wake up sweaty with damp sheets. Often at night and sometimes during the day, my feet feel like they are on fire and are burning. My hands are usually warm when everyone else has cold hands. Ive mentioned it to three rheumatologists, and they didnt offer any explanation or remedy.
When we asked about this symptom on Facebook, we got an overwhelming response from the CreakyJoints community. I will go from fine to feeling like Im on fire in a matter of seconds. This has been happening for several years, since being diagnosed, Rene Marie B. told us. My face and scalp sweat the most and I can be around people who say its not hot while Im dripping sweat. At night I have blankets on and off a million times. I hate it.
Nearly all the responses echoed similar situations. Yes, this happens to me every day. My face feels like its going to catch fire its so hot, Diana M. shared. Its embarrassing when you are out around people and they ask if you are all right. I just feel like I want to sit on a block of ice and everyone else has their coats on. Very frustrating!
Recommended Reading: How To Help Arthritis In Your Hands
Does Hypothyroidism Cause Night Sweats
â
People who live with hypothyroidism struggle with heat regulation. Cold intolerance is the most common thermal symptom of hypothyroidism. However, some people may also experience night sweats. When the thyroid gland is compromised, and hormone levels are off-balance, you can experience uncomfortable temperature-related symptoms.
Vasculitis Skin Lesions And Other Conditions
Small-vessel vasculitis may cause infarcts near the ends of the fingers or toes, especially around the nail beds, that are typically of little consequence other vasculitis-related complications can be more serious.2 While a senior with RA may be vulnerable to the common causes of lower extremity ulcers , a skin breakdown secondary to vasculitis can also be the cause of ulcers and may not be distinguished from stasis ulcers.5,7 Vasculitis ulcers do not respond to regular stasis ulcer therapy and require aggressive treatment of the inflammatory process.2 Vasculitis usually occurs in patients with long-standing RA when larger vessels are involved, infarcts may cause irreversible motor deficits and visceral involvement.2 Other dermatologic conditions in seniors have been associated with RA, including autoimmune bullous dermatosis Raynaud’s phenomenon palmar hyperhidrosis and pyoderma gangrenosum.5
You May Like: How To Deal With Arthritis
Simple Guide For A Healthy Sleep
Doctor-approved tips to help you relieve insomnia and get a good night’s rest, starting tonight.
Adopt a healthy lifestyle
Exercising during the day can improve sleep quality and decrease stress. Similarly, controlling your weight may help reduce night sweats and difficulty resting.
Some foods and supplements like omega-3s may help relieve night sweats. However, most supplements that aim to treat night sweats gear toward treating menopausal vasomotor symptoms in women like night sweats and hot flashes.â
There are plenty of strategies you may try to get rid of pesky night sweats. The best tactic is to find the right thyroid medication and dosage to control your hypothyroidism. Once you find the correct medicine for your body, your thermostat has a strong chance to reset. If you have tried the above strategies without relief, consult your thyroid doctor to stay comfortable all night.
So What Causes The Overheated Feeling
The short answer: no one knows for sure. To our knowledge, there are no studies that have researched this specifically. One study that looked into patient perceptions of flares noted one participant who reported, when I have a flare and theres a lot of pain I have a feeling that Im burning upmy whole body is hot I feel as though Ive got a very high temperature.
We dont know yet if theres any kind of connection between my body temperature dysregulation and autoimmune disease, Dr. Domingues says. Because it is a subjective feeling, he explains, it can be hard for doctors to observe and for researchers to quantify in studies.
What could be done, though, is study fluctuations in actual body temperature. One of the things we think about is if the inflammatory cytokines such as TNF alpha are upregulated , then that may drive a little bit more of the heat on the body, he says. This seems to be much more prominent in the joints but because inflammatory arthritis is a systemic illness, you can also see it in other soft tissues.
But, he adds, I dont think any study has been done to measure temperature in patients to see if theres a difference but still in the normality of range say, from 97 to 98.5 in rheumatoid arthritis patients. Maybe its that their temperature may be a little more elevated than normal but theyre still not febrile , Dr. Domingues says. We dont really have good studies on that.
Also Check: Test For Arthritis In Knees
What Causes Sweating With Ra
Health care providers, rheumatologists, and researchers dont know for sure what causes people diagnosed with RA to feel overheated and to sweat excessively. One study on RA symptoms during flares noted that a participant reported feeling that theyre burning up as though they have a very high temperature during flare-ups. However, there have not yet been studies dedicated to researching sweating, in particular. Self-reported symptoms like overheating and sweating can be hard for doctors to observe and for researchers to quantify in studies, experts say.
It may be the case that some autoimmune disorders like RA can affect the bodys ability to maintain a normal temperature. One study from Michigan Medicine suggested that RA inflammation may affect the brain, which plays a key role in regulating body temperature.
Some people with RA also have a condition known as autonomic dysfunction, according to the Cleveland Clinic. Autonomic dysfunction occurs when the body isnt properly managing the autonomic nervous system, which controls body temperature, among other automatic functions.
Some of the medications used to treat RA have also been known to cause hot flashes, night sweats, and excess sweating as potential side effects .
See what RA specialist Dr. Iris Navarro-Millán says about weight loss and night sweats in RA.
If You Have Night Sweats Theres No Need To Toss And Turn In Bed Like Youre On The Heavy Seas Relief May Be Out There
Night sweats a really common complaint, Dr. Weinstein says. If they are really bothersome and interfering with life, its time to see a doctor.
Your doctor will review your symptoms, do a physical exam, and probably do some bloodwork or other lab exams as they see fit, Dr. Okeke-Igbokwe says. From there, you and your physician can work together to identify potential causes of your night sweats, talk about treatments, and get you closer to sweat-free sleep.
Related:
Recommended Reading: Is Peanut Bad For Arthritis
Talk To Others Who Understand
Members of myRAteam know that having a team of others who understand life with rheumatoid arthritis can make all the difference. They regularly ask questions, give advice, and share stories about living with and managing RA.
Do you experience hot flashes, sweating, or overheating with RA? If youve found a way to manage it, let other members know in the comments below or by starting a new conversation thread.
Treatment Of Night Sweats
The best way to treat night sweats is to determine the underlying cause and address it. The following is a summary of potential treatment options depending on the cause of the night sweats.
Adjusting sleep habits may help, regardless of the cause. Lowering the temperature of your bedroom at night, wearing lighter sleepwear, using lightweight covers, etc. may help with the night sweats.
Don’t Miss: How To Deal With Arthritis
How The Thyroid Controls Body Temperature
The thyroid gland is the thermostat of the body. A healthy thyroid sends signals throughout the body to generate and stabilize heat. When you are low in thyroid hormone , your body does not have enough signals to create energy for heat production. Therefore, most people with hypothyroidism have cold intolerance that is, they are always cold even when temperatures outside of the body do not warrant feeling cold.
Rheumatoid Factor And Anticitrullinated Peptide Antibodies
Anticitrullinated peptide antibody levels are more specific for RA and correlate with erosive disease. Rheumatoid factor is a nonspecific immunoglobulin that is also detected in chronic infections, such as hepatitis C, tuberculosis, and infective endocarditis, and in autoimmune disorders such as paraproteinemias, vasculitis, or SLE and should prompt consideration for these entities in the absence of a typical RA joint pattern.11,12 The diagnostic value of rheumatoid factor testing may be limited by its specificity however, it should be used when signs and symptoms of inflammatory arthritis are present. In the clinical setting of symmetric polyarthritis, a high rheumatoid factor titer is associated with poor outcomes and high predictive value for diagnosing RA.13
Don’t Miss: Arthritis In Fingers And Toes Symptoms