Chronic Reactive Arthritis And Lifestyle Modification Approaches
In as many as 30 percent of cases, the patient can develop chronic symptoms and this poses many challenges therapeutically for doctors and specialist physicians. In these cases, the condition is usually treated with disease-modifying anti-thematic drugs , which are administered in the form of an injection and help to remove fluid build-up in the joints. If the joints are particularly inflamed, steroid injections are sometimes also recommended in the joints and muscles, and these work by blocking the effects of the chemicals in the body that triggered the inflammation.
Key Points To Remember
- Symptoms of reactive arthritis generally occur four to six weeks after a child has recovered from an infection.
- Your childs doctor will need to rule out other conditions that can mimic the symptoms of reactive arthritis before making a correct diagnosis of this condition.
- Reactive arthritis is a fairly common form of arthritis in children and usually goes away in about six weeks with proper treatment.
What Is Reactive Arthritis
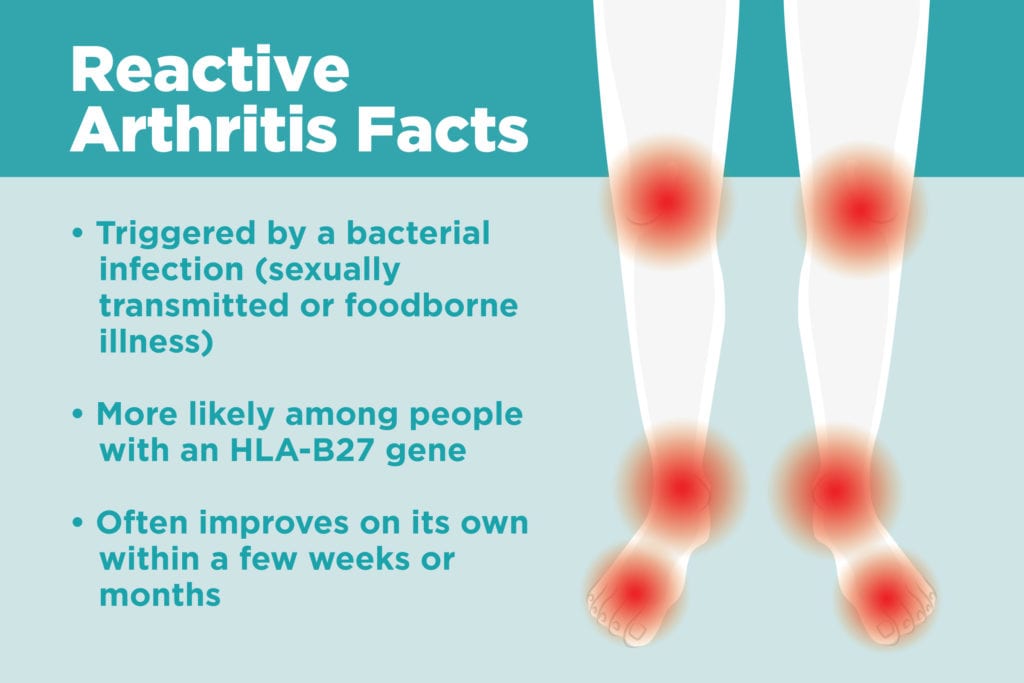
Reactive arthritis causes inflammation, swelling and pain in the joints. Knees, ankles and the feet are the joints most often affected.
Caused by an infection, reactive arthritis is not contagious, but if the underlying infection is still active, the infection itself may be contagious.
Once referred to as Reiters disease or Reiters syndrome, this inflammatory form of arthritis now belongs to a particular arthritis group called spondyloarthritis. Arthritis in this group causes inflammation, pain, stiffness and sometimes deformities of the spine. Under this classification, axial spondyloarthritis, peripheral spondyloarthritis, psoriatic arthritis and enteropathic arthritis are included along with reactive arthritis.
When arthritis, urethritis and conjunctivitis occur concurrently, it is referred to as the Reiters syndrome triad. In addition to the joint pain, infection in the eye and infection in the urethra , the disease may manifest on the skin. Lesions, pus-filled sores and rashes are possible.
Reiters syndrome in women is less common, accounting for approximately one-fifth of the cases. In addition to adults, children have been diagnosed, but this is considered rare.
Don’t Miss: How Can You Stop Arthritis In Your Hands
Risk Factors For Sara
There are several predisposing factors for SARA.
-
Gender: SARA appears to occur over ten times more frequently in men compared to women but under-recognition or milder disease in women may be a factor.
-
HLA-B27: The gene is 10 times more common in those with SARA and is associated with more severe disease.
-
HIV infection: A rising incidence of spondyloarthritis, including ReA, has been seen in sub-Saharan Africa in association with HIV. Similar observations have not been seen in Caucasian populations.
Medications For Pain Relief
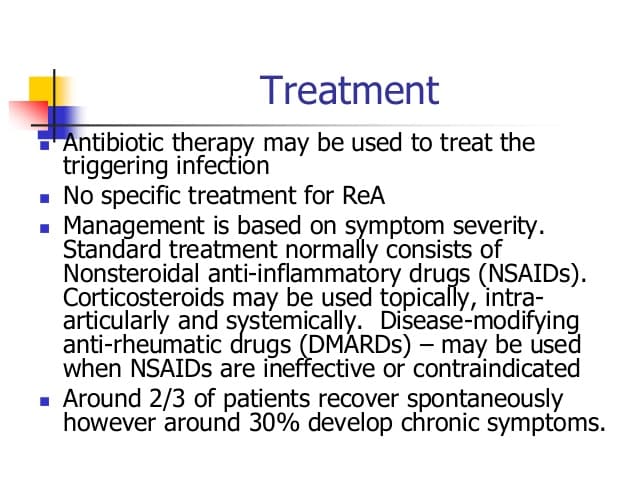
In mild cases that last less than 6 months, patience and over-the-counter medications called NSAIDs may be all that is needed. If the person has moderate to severe joint pain, a doctor may recommend prescription NSAIDs and/or steroid treatment. For more severe or protracted cases, prescription medications called DMARDs and biologics may be recommended.
NSAIDs. Non-steroidal anti-inflammatories, such as ibuprofen and aspirin, may be taken to reduce inflammation and pain. These drugs are available over-the-counter or by prescription in higher strengths. Long-term daily use of NSAIDs can have side effects, including stomach, kidney, and liver damage, so patients and doctors should discuss other options if symptoms are prolonged.
Recommended Reading: Mayo Clinic On Arthritis
How Is Reactive Arthritis Diagnosed
Diagnosis of reactive arthritis can be complicated by the fact that symptoms often occur several weeks apart. A doctor may diagnose reactive arthritis when the patient’s arthritis occurs together with or shortly following inflammation of the eye and the urinary tract and lasts a month or longer.
There is no specific test for diagnosing reactive arthritis, but the doctor may check the urethral discharge for sexually transmitted diseases. Stool samples may also be tested for signs of infection. Blood tests of reactive arthritis patients are typically positive for the HLA-B27 genetic marker, with an elevated white blood cell count and an increased erythrocyte sedimentation rate — both signs of inflammation. The patient may also be mildly anemic .
X-rays of the joints outside the back do not usually reveal any abnormalities unless the patient has had recurrent episodes of the disease. On an X-ray, joints that have been repeatedly inflamed may show areas of bone loss, signs of osteoporosis, or bony spurs. Joints in the back and pelvis may show abnormalities and damage from reactive arthritis.
Can Reactive Arthritis Be Prevented
This depends on the underlying infection that triggered the reactive arthritis. If itâs a urinary tract infection or STD caused by chlamydia, antibiotic treatment of the acute infection can prevent ReA from developing.There is no evidence suggesting that ReA resulting from gastroenteritis or chronic ReA can be prevented by antibiotic treatment.
Recommended Reading: How To Deal With Arthritis
Deterrence And Patient Education
The social taboo associated with genitourinary symptoms often becomes a challenge in obtaining a complete and accurate history from patients. Some studies have suggested that appropriate treatment of acute Genitourinary infection with a 3-month course of antibiotics can prevent ReA. However, this is highly controversial.
Similarly, from a physician’s perspective, identifying the triad of visual, genitourinary, and arthritis symptoms to a pattern of unifying diagnosis are time-sensitive. It is even more so when acute uveitis or iritis sets in, as they can rapidly progress to permanent loss of visual function if not intervened upon in due time.
Treating Any Triggering Infection
- If the trigger is an infection of the urethra, a short course of antibiotics will usually be advised.
- Gut infections have often cleared on their own by the time the reactive arthritis develops. But, if a stool sample shows that a germ is still present then treatment may be advised to clear it.
Note: clearing the triggering infection does not usually alter the course of the arthritis. Once the arthritis is triggered, it will usually run its course well after any infection has gone. However, some studies suggest that long-term treatment with antibiotics may help to reduce the length of the arthritis in some cases, particularly if chlamydia is the triggering infection. The use of long-term treatment with antibiotics in reactive arthritis is currently being investigated.
Recommended Reading: How To Deal With Arthritis
Does It Run In Families
You cant pass reactive arthritis on to your children. However, they can inherit the HLA-B27 gene, which could slightly increase their chance of getting the condition. This doesnt mean that by having this gene theyll definitely get reactive arthritis. However, the condition tends to be more common in people with HLA-B27.
Around 1 in every 10 people in the UK carry this gene.
The first signs of reactive arthritis are often:
- painful and swollen joints, usually in the ankles or knees
- sausage-like swelling of fingers or toes
- puffy, sore, red eyes, often with a mucus discharge known as conjunctivitis
- extreme, unexplained tiredness, known as fatigue
You may notice that your knees, ankles or toes suddenly become swollen, stiff and painful to move. Or the swelling may appear gradually over a few days.
Reactive arthritis can also affect other joints, such as your fingers, wrists, elbows and the joints at the base of your spine, known as the sacroiliac joints . It can also cause inflammation in the tendons around your joints, such as the Achilles tendon which runs down the back of your ankle.
You may find your whole finger or toe swells up if both the tendons and joints become affected at the same time. This is often called sausage digit or dactylitis .
Is There A Test For Reactive Arthritis
There is no single test that doctors can use to see if you have reactive arthritis. Doctors may suspect that you have it if you have joint pain, and have had an infection of the digestive or urinary tract or the genitals in the past few weeks.. To figure out if you have reactive arthritis, your doctor may:
- Take your medical history and do a physical exam.
- Order lab tests.
- Send you for x-rays or other imaging tests.
Don’t Miss: How To Deal With Arthritis
Tips To Reduce Your Risk Of Infection
- Try to avoid close contact with people you know have an infection.
- Wash your hands regularly and carry around a small bottle of antibacterial hand gel.
- Keep your mouth clean by brushing your teeth regularly.
- Stop smoking if youre a smoker.
- Make sure your food is stored and prepared properly.
- Try to keep your house clean and hygienic, especially the kitchen, bathrooms and toilets.
If you are prescribed a drug you may find more information about it here.
Self Care How Can I Look After Myself
In the early stages of reactive arthritis, it’s recommended that you get plenty of rest and avoid using affected joints. As your symptoms improve, you will slowly need to start exercises to strengthen affected muscles and improve the range of movement in your affected joints.
Your doctor or specialist may recommend a suitable exercise programme for your arthritis, or may refer you to a physiotherapist. You may also find ice packs and heat pads useful in reducing joint pain and swelling. Do not place these directly on your skin.
Don’t Miss: What Does Arthritic Knee Pain Feel Like
What Tests Do Health Care Professionals Use To Make A Diagnosis Of Reactive Arthritis
There is no single lab test used to diagnose reactive arthritis. Reactive arthritis is diagnosed based upon recognition of the combination of arthritis with symptoms such as inflammation of the eyes, and the genital, urinary, and/or gastrointestinal systems. The health care professional obtains a medical history to note the time course of possible infection in the genital or urinary tracts, or the bowel. Stiffness and pain are monitored. Inflammatory types of joint problems typically cause more stiffness in the morning. Blood tests such as a sedimentation rate may be obtained to document the presence of inflammation in the body. The rheumatoid factor, which is typically present in rheumatoid arthritis, is usually negative in reactive arthritis. The HLA-B27 gene marker blood test can be helpful, especially in the diagnosis of patients with spine disease. Other tests may be ordered to eliminate other possible diseases with similar symptoms.
Sometimes the fluid of the inflamed joint needs to be examined. In this case, a health care professional will use a needle to withdraw fluid from the joint in sterile fashion. The joint fluid will be examined for white blood cells, bacteria , and crystals .
Antibiotics may be prescribed if one still has the infection that triggered reactive arthritis.
The inflammation around the penis can be helped by cortisone creams . When bacteria are discovered in the bowel or urine, antibiotics specific for those bacteria are given.
History Of The Condition’s Name
A doctor noticed that some people had a ‘triad’ of symptoms: joint inflammation , infection of the urethra and inflammation of the front of the eye , all at the same time. The condition was named after him but has subsequently become known as ‘reactive arthritis’. We know now that reactive arthritis often, but not always, has these three symptoms. In some cases there are additional symptoms and it may also follow a sexually transmitted infection.
Recommended Reading: Can Rheumatoid Arthritis Affect Your Back
Prognosis Of Reactive Arthritis
In most people, the initial symptoms of reactive arthritis disappear in 3 or 4 months, but up to 50% of people have recurring joint inflammation or other symptoms over several years.
Deformities of the joints, spine, and joint between the spine and the hip bone may develop if the symptoms persist or recur frequently. Some people who have reactive arthritis become permanently disabled.
Home Remedies And Pain Relief
Engaging in plenty of physical activity can be of benefit to a person with arthritis.
Exercise will not prevent reactive arthritis, but it may help people with arthritis experience less pain due to flare-ups and have better joint health.
Preventing repeat infections that can trigger reactive arthritis is also important for self-care. People can use barrier methods, such as condoms, to reduce the risk of acquiring an STI, and they can store and cook food at recommended temperatures to stop the spread of foodborne bacteria.
A person may also be able to alleviate the pain of reactive arthritis attacks when they occur. The careful use of heating pads or ice taking care to shield the skin from direct contact with either can provide relief from pain and swelling. Minimizing the pressure on an affected joint may also help reduce pain and discomfort.
Don’t Miss: What Does The Rash From Psoriatic Arthritis Look Like
What Are Reactive Arthritis Risk Factors
- Gender: Reactive arthritis is more frequent in men.
- Age: It is most frequent in people 20-40 years of age.
- Hereditary factors: There are inherited genes, such as HLA-B27, that increase the risk for developing reactive arthritis.
The symptoms of reactive arthritis can be divided into those that affect the joints and those that affect the non-joint areas.
The classic joints that can become inflamed in reactive arthritis are the knees, ankles, and feet. The particular joints involved are usually asymmetric, that is, one side of the body or the other is affected with signs and symptoms, rather than both sides simultaneously. The inflammation leads to joint pain, stiffness, swelling, warmth, and redness. Patients may develop inflammation of entire fingers or toes which can give the appearance of a “sausage digit.” This feature is also seen in patients with another type of arthritis called psoriatic arthritis that is associated with skin inflammation of psoriasis. The arthritis of reactive arthritis can be associated with fever and inflammation of the spine, leading to stiffness and joint pain in the back or neck .
Cartilage can also become inflamed, especially around the breastbone where the ribs meet in the front of the chest this condition is called costochondritis. Muscles attach to the bones by tendons. In reactive arthritis, the tendon insertion points can become inflamed , tender, and painful when exercised. Achilles tendinitis is common with reactive arthritis.
Natural Remedies For Reactive Arthritis Symptoms
If you experience pain and swelling in your joints after an infection, you may have reactive arthritis. This form of arthritis causes inflammation and sometimes severe pain in the knees, ankles and feet, but it can also affect the heels, toes, back and fingers.
According to the American College of Rheumatology, reactive arthritis typically occurs as a short episode however, for some it can become a chronic condition. Generally, reactive arthritis symptoms come and go, with symptoms disappearing within a year.
Treatment isnt typically necessary except in severe or persistent cases. If the underlying infection that caused the reactive arthritis is still present or reoccurs, it will need to be treated.
Some research points to this disease being an autoimmune disorder. In the case of reactive arthritis, it may be caused by the immune system continuing to fight even after an infection is gone, according to Harvard Medical School.
While the bacteria that cause this disease are very common, reactive arthritis is fairly uncommon. Research continues to determine how genetics play a role.
Conventional reactive arthritis, or Reiters syndrome, treatment includes over-the-counter NSAIDs to relieve inflammation and reduce pain. More severe cases may require more aggressive treatment. Fortunately, there are natural remedies to help manage symptoms and improve the overall quality of life.
Don’t Miss: How Do I Know If I Have Knee Arthritis
Reactive Arthritis In Hiv Infection
Reactive arthritis may occur in HIVinfected patients and is sometimes the initial manifestation of the disease.17 The diagnosis of reactive arthritis should be considered in any patient with an asymmetric oligoarticular polyarthritis. Conversely, HIV infection should be considered in any new case of reactive arthritis where the etiology is at all unclear.
In these patients, arthritis may be severe and may progress rapidly. Azathioprine and methotrexate should not be used when HIV infection is suspected. It is not yet clear if antiretroviral therapy has any effect on the natural history of reactive arthritis in patients being treated for HIV infection.
Read the full article.
- Get immediate access, anytime, anywhere.
- Choose a single article, issue, or full-access subscription.
- Earn up to 6 CME credits per issue.
Who Develops Reactive Arthritis
Reactive arthritis is uncommon. It most commonly affects men aged between 20 and 40 years. This is because they are most at risk of urethral infection from sexually transmitted infections. However, it can occur at any age and in anyone. We are all at risk of getting a gut infection from food poisoning, which may trigger a reactive arthritis.
There is a genetic link too. About 1 in 14 people in the UK have a gene called HLA-B27. About 3 out of 4 people who have reactive arthritis have this gene. So, this gene seems to make you more likely to develop reactive arthritis if you have a triggering infection.
Don’t Miss: What Does Ra Pain Feel Like
Treatments For Reactive Arthritis
Symptoms stemming from reactive arthritis can be safely and effectively managed with oral medications. The type of medication used to treat reactive arthritis depends on the stage of the condition.
- Treatment for early stage reactive arthritis Acute, or early inflammation can often be effectively treated with non-steroidal anti-inflammatory drugs, or NSAIDs. NSAIDs work by suppressing swelling and reducing pain. These medications can be found over-the-counter such as naproxen or prescribed by your physician. The type of medication and dosage varies from patient to patient, so be sure to consult your rheumatologist about what will be most beneficial for you.
- Treatment for late stage reactive arthritis Chronic reactive arthritis typically requires the use of disease-modifying antirheumatic drugs, or DMARDs such as sulfasalazine or methotrexate.
In addition to the above medications, corticosteroid injections can help to decrease swelling and pain in individuals with chronic and severe reactive arthritis. If you are considering treatment for reactive arthritis, consult your physician about which course of treatment may be best suited for you.
To learn more about reactive arthritis treatment, visit medlineplus.gov