From The Lab To The Cardio
Translating research into clinical practice is paramount at Mayo Clinic. To that end, the divisions of cardiovascular diseases and rheumatology have joined forces to change the clinical approach to rheumatic conditions.
The Cardio-Rheumatology Clinic at Mayo Clinic opened in Rochester in the summer of 2013. The clinic provides specialized care focused on early detection, prevention and treatment of cardiovascular disease in patients with rheumatic conditions.
âWe saw the need for a team of specialists that understand the unique risks and circumstances of people with rheumatoid arthritis, so we created this special clinic just for those patients,â explains Mayo Clinic cardiologist Rekha Mankad, M.D., who directs the Cardio-Rheumatology Clinic in Rochester.
Dr. Gabriel concurs. âBecause they donât necessarily show cardiovascular symptoms the same way as other people, and because they take medication that other people arenât on and have poorer outcomes when they develop heart disease, they need more specialized care,â she says.
The Cardio-Rheumatology Clinic enables early referral of patients with rheumatic diseases to cardiology. Patients have both a traditional cardiovascular risk assessment and a vascular health assessment. The results help create an individualized plan to manage risks and symptoms.
Scarring Within The Lungs
In medical speak, its called interstitial lung disease a broad category of lung disorders, most of which lead to scarring in the tissue between the air sacs of the lungs . Chronic inflammation from rheumatoid arthritis can lead to this scarring over time, the buildup of scar tissue makes the lung tissue stiff, which interferes with breathing and can be difficult to treat.
ILD is the most common and most serious lung complication for people with RA: Research shows lung disease alone accounts for up to 20 percent of deaths in rheumatoid arthritis patients, and most are attributed to ILD. Though its rare, this scarring may also occur in a small number of people with ankylosing spondylitis.
Symptoms include shortness of breath and dry cough, as well as fatigue and weight loss. But by the time these signs appear, irreversible lung damage has often already occurred. Some estimates suggest about 30 percent of patients with rheumatoid arthritis have ILD, without obvious symptoms.
Congestive Heart Failure Ischaemic Heart Disease And Risk Factors
Several reports showed that the increased incidence of cardiovascular disease, including ischaemic heart diseases, or the presence of carotid atherosclerosis is not explained by traditional cardiovascular risk factors , suggesting that RA-related factors might influence the risk of cardiovascular disease .
The increased prevalence of congestive heart failure found in RA patients is underlined by recent echocardiographic studies. Left ventricular systolic dysfunction has been found to be three times more common than in the general population and was associated with abnormal electrocardiography, suggesting that screening of RA patients with abnormal electrocardiography may be worthwhile . Also, right and left ventricular diastolic dysfunction are found more frequently in RA patients without evident cardiovascular disease .
As the use of several drugs in RA, including corticosteroids and biological therapy, have such an important positive effect in the reduction of arthritis activity and improvement of functional capacity, it is important to have more knowledge on possible deleterious effects on the function of the heart due to these drugs.
You May Like: How Turmeric Is Linked To Arthritis
How Do I Know If My Ra Is Progressing
Signs Your RA Is Progressing
How Can Rheumatoid Arthritis Affect Lungs
Rheumatoid arthritis is a kind of joint disease. But although it primarily affects the joint, it can affect other parts of the body such as heart, eyes, and even lungs. Thats why it is also often called as a systemic inflammatory condition.
Understanding the complications of RA in general
Since RA can be systematic, there is a chance for the inflammation to spread and target other organs. RA itself is often considered as unusual arthritis because it is rheumatoid condition. In other words, it is linked to the abnormality of the patients immune system.
Lung is not the only one of distinct organ that can be affected by RA. It also can affect the eyes, heart, mouth, kidneys, liver, blood cells , blood vessels, and even nervous system.
The most common complication of poorly-controlled RA may be joint damage. Each flare poses the risk of damage to the joint. Therefore, the goal of the treatment is to reduce the number of the flares.
More flares of RA, the greater risk to develop the complications from the disease. It seems that poorly-controlled the disease is the key for the complications to occur.
Furthermore, the complications are more likely to occur in patients who have had moderate-to-severe rheumatoid arthritis for a long time.
How can RA affect the lungs?
Don’t Miss: What Is Arthritis Made Of
Other Bdmards And Tsdmards And Heart Disease
In addition to TNF-, IL-6 represents another proinflammatory cytokine targeted in RA. In the context of the development of major adverse cardiovascular events, the IL-6 receptor inhibitor tocilizumab was shown to be a safe alternative for the TNF- antagonist etanercept.
Abatacept and rituximab represent another class of bDMARDs, which target antigens on the surface of dendritic cells and B cells , respectively. T cell costimulation inhibitor abatacept is prescribed to patients with RA with a worse cardiovascular profile however, it does not affect the risk of developing heart failure compared with etanercept. Rituximab is a humanised chimeric anti-CD20 monoclonal antibody preventing B cell activation. Rituximab was shown to improve vascular pathophysiology in RA. In clinical trials, rituximab showed a cardiovascular safety profile comparable to anti-TNF- treatments.
Some patients with RA receive tsDMARDs JAK inhibitors tofacitinib or baricitinib. Both JAK inhibitors have been shown to worsen the plasma lipid profile however, data from clinical studies and databases do not suggest an increased cardiovascular risk in patients with RA treated with these drugs. It should be mentioned that statins can effectively reverse dyslipidaemia in patients with RA treated with tofacitinib.
Recommended Reading: How To Relieve Arthritis Pain In Thumb Joint
Peripheral Vascular Disease And Peripheral Artery Disease
The arteries and veins that carry blood throughout your body are collectively your vascular system. Any disease of the vascular system outside of the heart is known as peripheral vascular disease .12
Peripheral artery disease is a type of PVD. Veins carry oxygen-rich blood from the rest of the body to the heart, while your arteries bring this blood from the heart to the rest of the body. PAD occurs only in the arteries, slowing blood flow return. This causes the arms and legs to suffer from the decreased blood supply. PAD is caused by a build-up of plaque in the arteries.12
Along with the traditional risk factors for PAD, those with RA who take steroids are at an increased risk for this type of heart disease.11
Recommended Reading: What Are The Early Warning Signs Of Arthritis
Get Early Treatment For Ra
We are still working to understand the natural history of lung involvement in RA and how exactly medication may be involved. At this point, I would encourage early screening for lung involvement for patients with signs and symptoms, says Sparks. If you have RA and are experiencing shortness of breath, coughing, or other respiratory symptoms, talk to your doctor. These are potentially serious symptoms that warrant prompt attention.
RELATED: Early Rheumatoid Arthritis Treatment: Why Is It So Important?
How Heart Disease Affects People With Ra
Dr. Navarro-Millán is an advocate for coordinated care, in which people with RA get primary care along with seeing a rheumatologist. She emphasized that primary care doctors and rheumatologists need to stay in close communication when risk factors are identified. As rheumatologists, we are really focused on controlling pain, decreasing inflammation, and decreasing and monitoring side effects of medication, Dr. Navarro-Millán said.
But people with RA need to have regular screenings by primary care providers for cardiovascular disease risk factors like hyperlipidemia high cholesterol and high blood pressure. Many of my patients with rheumatoid arthritis say, Well, I dont have anything else but rheumatoid arthritis. Why should I see a primary care provider? And that is where things start to fall through the cracks, she noted.
One myRAteam member described her experience discovering heart problems unexpectedly. I am in the hospital with high blood pressure and a high heart rate, she said. I went to see my rheumatologist and she sent me straight to the emergency room. I dont have a history of heart problems or high blood pressure.
Also Check: How To Get Rid Of Arthritis Knee Pain
Don’t Miss: What To Do For Arthritis In Back
What Is The Difference
Rheumatoid arthritis vs. osteoarthritis
Rheumatoid arthritis and osteoarthritis are both common causes of pain and stiffness in joints. But they have different causes. In osteoarthritis, inflammation and injury break down your cartilage over time. In rheumatoid arthritis, your immune system attacks the lining of your joints.
Rheumatoid arthritis vs. gout
Rheumatoid arthritis and gout are both painful types of arthritis. Gout symptoms include intense pain, redness, stiffness, swelling and warmth in your big toe or other joints. In gout, uric acid crystals cause inflammation. In rheumatoid arthritis, its your immune system that causes joint damage.
What Medications Treat Rheumatoid Arthritis
Early treatment with certain drugs can improve your long-term outcome. Combinations of drugs may be more effective than, and appear to be as safe as, single-drug therapy.
There are many medications to decrease joint pain, swelling and inflammation, and to prevent or slow down the disease. Medications that treat rheumatoid arthritis include:
Non-steroidal anti-inflammatory drugs
Biologics tend to work rapidly within two to six weeks. Your provider may prescribe them alone or in combination with a DMARD like methotrexate.
Also Check: Does Omega 3 Help Rheumatoid Arthritis
The Direct Effects Of Rheumatoid Disease On Lung Tissue And Pleura
People with RA can develop disease in their lungs, as a consequence of their immune system attacking their joints and other tissues. Different types of lung disease can occur, including interstitial lung disease , bronchiectasis and bronchiolitis obliterans. In each of these, inflammation and damage can occur to the lung tissue, reducing the ability to absorb oxygen from the air we breathe into the bloodstream and causing breathlessness in affected people. Often this is accompanied by a persistent cough, especially with exertion. Breathing tests and a CT scan of the lungs are used to confirm the diagnosis, and precise patterns of lung disease are described.
What Are The Treatments For Rheumatoid Arthritis
RA is usually treated with a combination of medications to relieve swelling and pain while regulating the immune system. Joint surgery to relieve pain and disability, including joint replacement, may also be considered when these nonsurgical methods have failed to provide lasting benefit.
With early detection and intervention, RA and other forms of inflammatory arthritis can be treated very effectively. The connects patients quickly and efficiently with a rheumatologist who can evaluate their joint pain and get each patient started on an appropriate course of treatment. HSS also offers specialized for people with RA.
Today, we are blessed with a deeper understanding of the pathogenesis and characteristics of RA and the availability of safe and effective medications that can alter the natural history of RA and improve function. We start with the premise that RA is eminently controllable, and the goal of our therapies is âno evidence of disease.â That means no signs of redness, warmth, swelling or tenderness and normal function. Since we would not accept uncontrolled illness in angina, chronic obstructive lung disease, hypertension or diabetes, we should similarly not accept it in RA. Luckily, today, we have the therapeutic tools to make this happen.
Don’t Miss: How To Cure Arthritis Naturally
Can Ra Be Fatal
RA alone is not fatal. Fatality occurs due to complications associated with the inflammation caused by RA. In severe cases, patients can develop other medical conditions. The other medical conditions that patients need to be aware when it comes to shortened RA life expectancy include:
- Respiratory conditions like Chronic Pulmonary Obstruction Disorder
Off course, these are conditions that everyone should be concerned about. Keeping your body healthy through diet, exercise, and positive habits will go a long way to reducing the risk of fatality from any of these conditions.
Also Check: How Can You Prevent Arthritis
How Is Rheumatoid Arthritis Treated
Your healthcare provider will figure out the best treatment for you based on:
- How old you are
- How well you handle certain medicines, treatments, or therapies
- If your condition is expected to get worse
- Your opinion or preference
There is no cure for RA. The goal of treatment is often to limit pain and inflammation, and help ensure function. You may have 1 or more types of treatments. Treatment may include:
- Medicines. Some medicines may be used for pain relief. Some are used to treat inflammation. Others can help to slow the disease from getting worse. Medicines should be managed by a rheumatologist. This is a doctor who specializes in arthritis and rheumatic diseases. You may need regular blood tests to check how the medicines affect your blood cells, liver, and kidneys.
- Splints. Splints may be used to help protect the joints and strengthen weak joints.
- Physical therapy. Physical therapy may be used to help increase the strength and movement of the affected areas.
In some cases, surgery may be an option if other treatments dont work. Surgery does not cure RA. It helps correct the deformities caused by the disease. After surgery, RA can still cause problems. You may even need more surgery. Joint repair or reconstruction can be done in many ways, including:
You May Like: What Can Be Done For Severe Arthritis In Lower Back
Whats The Age Of Onset For Rheumatoid Arthritis
RA usually starts to develop between the ages of 30 and 60. But anyone can develop rheumatoid arthritis. In children and young adults usually between the ages of 16 and 40 its called young-onset rheumatoid arthritis . In people who develop symptoms after they turn 60, its called later-onset rheumatoid arthritis .
You May Like: How Do You Get Rheumatoid Arthritis
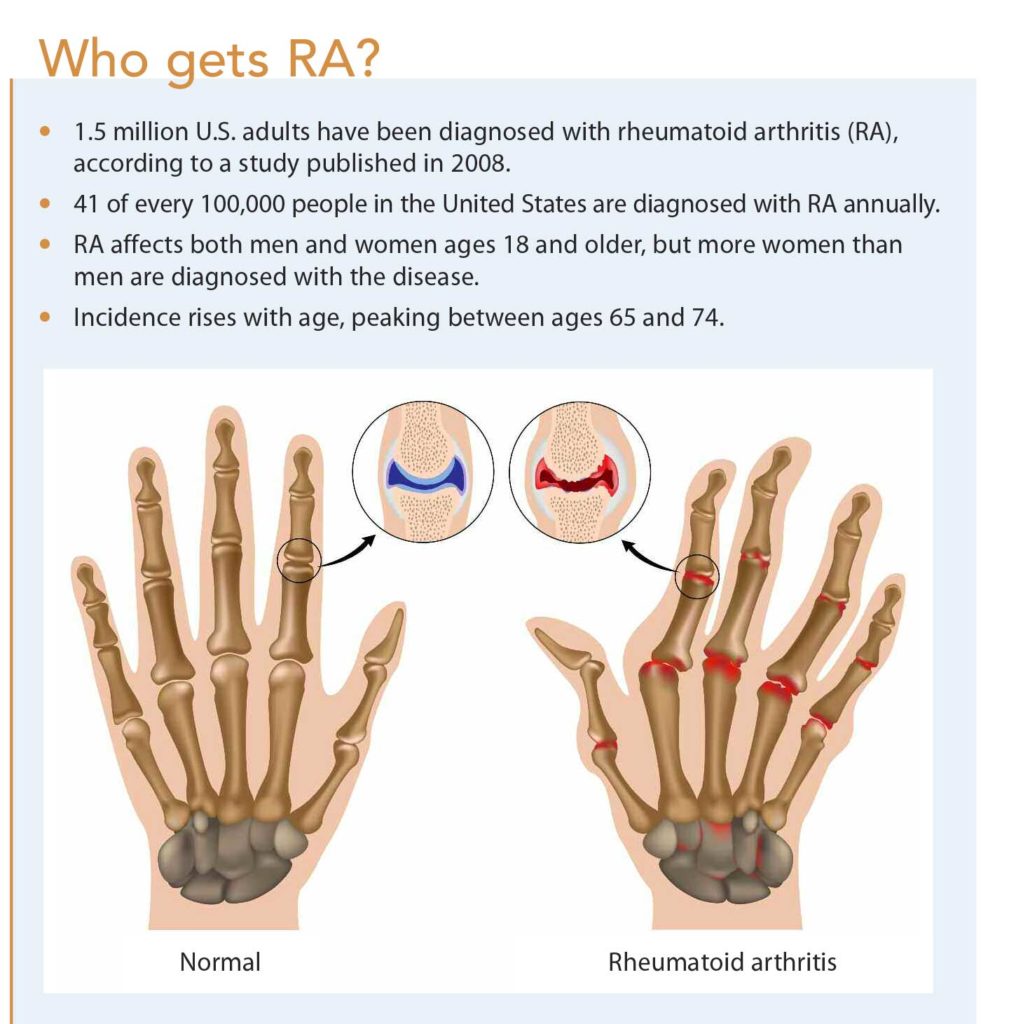
What Are The Risk Factors For Ra
Researchers have studied a number of genetic and environmental factors to determine if they change persons risk of developing RA.
Characteristics that increase risk
- Age. RA can begin at any age, but the likelihood increases with age. The onset of RA is highest among adults in their sixties.
- Sex. New cases of RA are typically two-to-three times higher in women than men.
- Genetics/inherited traits. People born with specific genes are more likely to develop RA. These genes, called HLA class II genotypes, can also make your arthritis worse. The risk of RA may be highest when people with these genes are exposed to environmental factors like smoking or when a person is obese.
- Smoking. Multiple studies show that cigarette smoking increases a persons risk of developing RA and can make the disease worse.
- History of live births. Women who have never given birth may be at greater risk of developing RA.
- Early Life Exposures. Some early life exposures may increase risk of developing RA in adulthood. For example, one study found that children whose mothers smoked had double the risk of developing RA as adults. Children of lower income parents are at increased risk of developing RA as adults.
- Obesity. Being obese can increase the risk of developing RA. Studies examining the role of obesity also found that the more overweight a person was, the higher his or her risk of developing RA became.
Characteristics that can decrease risk
Don’t Miss: How Can Arthritis Be Cured
People With Rheumatoid Arthritis Have A Higher Risk Of Developing Infections
People with RA are more susceptible to infections because of the disease itself and increased vulnerability from medications.
The drugs used for treating RA, including methotrexate, an injectable drug that suppresses inflammation in order to reduce joint pain, can cause a defect in white blood cells which helps fight infection and foreign invaders in our bodies.
As well as this, people who have had surgery on joints such as hip replacements or surgeries may need extended time off work due to their impaired ability to move around without causing further damage whilst recovering making them less likely to be able to keep themselves clean and healthy.
The risk is also higher if you smoke tobacco products also increases the likelihood of developing infections.
There are other treatments available including steroids that do not affect your immune system or even stopping some medication altogether.
It is important to visit the doctor if you are experiencing swollen joints, flu symptoms, or fever.
The most common infections that people with RA can develop include:
- Lung abscesses caused by bacteria and tuberculosis all of which can be fatal as your immune system becomes so weakened it cannot fight off these types of diseases.
- People with rheumatoid arthritis have an increased risk of developing infections because inflammation may damage white blood cells.
Fortunately, these types of infections also respond well to antibiotics.
What Health Conditions Can Affect Life Expectancy Among Ra Patients
RA patients appear to have a higher risk overall of developing serious lung or heart problems as well as infections, cancers and stomach problems. The reasons for RA patients being more susceptible to infections and cancers may be related to the altered function of the bodys defence system . However, as many of the drugs used for treatment of RA also have an impact on the immune system, these are also implicated. The following paragraphs look at each of these risk factors in more detail.
Infection risk:
Most infections in patients with RA are not serious, and in recent years studies have shown that the more commonly used drugs do not significantly increase the risk of serious infections. However, azathioprine, cyclophosphamide and corticosteroids do appear to increase the risk of infections.
The number of biological therapies has increased exponentially in recent years, and although the agents are effective, there is also a small, but important increased risk in serious infections. The risk of infection is largely determined by non-modifiable factors and modifiable factors . Anti-TNF drugs and some other biologics are linked with an increased risk for reactivation of tuberculosis , in people who had been exposed to TB in the past , so you are likely to be screened for TB before you are able to start on this type of treatment, and if positive will require treatment.
Lung problems:
Cancer:
Stomach problems:
Heart disease:
You May Like: Is Ankylosing Spondylitis Rheumatoid Arthritis