How Rheumatologists Diagnose Ra
Findings from a physical exam and medical history are important factors in diagnosing RA, say experts. Common RA symptoms include:
- Joints that feel tender, warm, or swollen for six weeks or more
- Multiple joints can be affected
- Joint pain that is commonly symmetrical
- Joint stiffness, especially first thing in the morning that lasts for an hour or more
- Fatigue
- Low-grade fever
- Loss of appetite
While many of these symptoms can occur with other diseases, infections, or injuries, there are subtle traits unique to RA that can help doctors make the diagnosis.
Pain, swelling, and stiffness in smaller joints in the hands, toes, and elbow, for example as opposed to one or two bigger joints, like the knee and hip, usually indicates a pattern more likely to be RA, says Dr. Husni. Pain from RA is usually more symmetric in nature, occurring on both sides of the body. When you injure yourself or have an overuse injury, however, pain usually occurs in just one joint. Joint stiffness can occur with injuries or other conditions, but stiffness with RA typically occurs in the morning and can be overwhelming, explains Dr. Husni. Its not a joint stiffness that passes after a few minutes, but more like you cant even move the covers to get out of bed.
Is There A Link Between Osteoarthritis And Osteoporosis
Q) Is there a link between osteoarthritis and osteoporosis? If you have one of these conditions, is there more chance that you may get the other? My mother had both. I had a hysterectomy at the age of 47, and was on HRT for five years. I recently had a DEXA scan and found that I have a condition called osteopenia.
Angela, Swindon, Wiltshire – 2008
A) For a long time rheumatologists have believed that there’s an inverse relationship between osteoarthritis and osteoporosis that people are unlikely to have both conditions at the same time. In fact, it was thought that having osteoporosis is protective against developing osteoarthritis. Now the facts don’t quite fit with this theory, although some of the evidence is still compelling. We see people in everyday practice who present with a new hip joint and now have a fracture in another bone and osteoporosis, just like your mother. Osteopenia is used to describe bones that have lost calcium, but not severely enough to call it osteoporosis. Usually both these conditions are diagnosed after a DEXA scan, which gives a more precise estimate of the amount of calcium in the bones.
This answer was provided by Dr Philip Helliwell in 2008, and was correct at the time of publication.
What Are The Signs And Symptoms Of Ra
With RA, there are times when symptoms get worse, known as flares, and times when symptoms get better, known as remission.
Signs and symptoms of RA include:
- Pain or aching in more than one joint
- Stiffness in more than one joint
- Tenderness and swelling in more than one joint
- The same symptoms on both sides of the body
- Weight loss
Don’t Miss: What Can You Do To Help Arthritis In Your Hands
Drug Treatments And Challenges
Your treatment goal is remission, the lowest possible level of disease activity. This can prevent joint damage and can keep your joints working like they should.
Your doctor will probably give you the same drugs used to treat early-onset RA. These include:
- Disease-modifying antirheumatic drugs
- Nonsteroidal anti-inflammatory drugs
- Corticosteroids
You might have more challenges with your medication, especially if you take drugs for other health conditions. This boosts your chances of a bad reaction to the medicine.
You may also have a harder time with drug side effects. NSAIDs increase your chances of heart, brain, gut, and kidney problems. Corticosteroids up the odds of glaucoma, osteoporosis, and other health problems.
Does Rheumatoid Arthritis Contribute To Dry Eyes
Q) I’ve suffered from dry eyes for a long time. I suffer from rheumatoid arthritis and had a hip replacement in 2000. I’ve tried all the remedies the NHS has to offer and have been on sulfasalazine and methotrexate for three years. Does rheumatoid arthritis contribute to dry eyes? Can you suggest a cure or anything to relieve the symptoms?
Gordon, Shetland – 2010
A) Dry eyes are a recognised feature of rheumatoid arthritis. The rheumatoid process can cause damage to the cells that produce the moisture for the eyes and mouth. This is called Sjögrens syndrome . At its most severe, this condition can lead to damage of the surface of the eye and visual impairment, so it’s important to seek help. Mostly, lubricant eye drops are used, but sometimes surgical solutions are necessary. These include putting a plug in the duct that drains the tears away. Lubricants can also be used for the mouth and a tablet called pilocarpine may help both eyes and mouth.
This answer was provided by Dr Philip Helliwell in 2010, and was correct at the time of publication.
Also Check: What Does Arthritic Changes Mean
Is The Risk Of Rheumatoid Arthritis High In Women
Several inquests reveal that when compared with men, women are three times more prone to be diagnosed with rheumatoid arthritis, and the rheumatology symptoms in women may be more severe. Women are more likely to be affected at a younger age by this autoimmune condition, and men appear to have more cases of remission.
How To Diagnose The Cause Of Night Sweats
Diagnosis of night sweats begins with a discussion with your healthcare provider about the severity, frequency, and any associated symptoms you may have with your night sweats. A physical exam may further narrow down potential causes to allow for a more focused work-up. As mentioned above, night sweats can be a symptom of an underlying medical condition, and your provider will look for other symptoms like hot flashes, abnormal periods, fevers, cough, unexplained weight loss, heartburn, and snoring. Tell your provider if you have a history of medical conditions like diabetes, HIV, substance abuse, obstructive sleep apnea, hyperthyroidism, or anxiety disorders. In some cases, additional testing like bloodwork or chest x-rays may be indicated.
Don’t Miss: Rheumatoid Arthritis Knee Pain Relief
What Are The Risk Factors For Ra
Researchers have studied a number of genetic and environmental factors to determine if they change persons risk of developing RA.
Characteristics that increase risk
- Age. RA can begin at any age, but the likelihood increases with age. The onset of RA is highest among adults in their sixties.
- Sex. New cases of RA are typically two-to-three times higher in women than men.
- Genetics/inherited traits. People born with specific genes are more likely to develop RA. These genes, called HLA class II genotypes, can also make your arthritis worse. The risk of RA may be highest when people with these genes are exposed to environmental factors like smoking or when a person is obese.
- Smoking. Multiple studies show that cigarette smoking increases a persons risk of developing RA and can make the disease worse.
- History of live births. Women who have never given birth may be at greater risk of developing RA.
- Early Life Exposures. Some early life exposures may increase risk of developing RA in adulthood. For example, one study found that children whose mothers smoked had double the risk of developing RA as adults. Children of lower income parents are at increased risk of developing RA as adults.
- Obesity. Being obese can increase the risk of developing RA. Studies examining the role of obesity also found that the more overweight a person was, the higher his or her risk of developing RA became.
Characteristics that can decrease risk
What Drugs Should I Be Taking For Rheumatoid Arthritis
Q) I’m 61 and I’ve had rheumatoid arthritis in both my hands for about five years.
At first I was in complete denial and refused to go onto any sort of medication, which, looking back on it, was extremely foolish. Since then I’ve been on several types of medication, including methotrexate. I lasted precisely 11 weeks on it before developing nausea and shortness of breath. I consequently got very frightened and came off it immediately.
For the past 18 months, I’ve been on sulfasalazine, which, although is keeping it at bay, isn’t preventing the damage to my joints. I’ve had several flare-ups, which have rendered me almost immobile at times.
My rheumatologist is now trying to persuade me to try methotrexate again, this time by injection, or biological medication, which will also be by injection.
I’ve got to the stage where I feel like coming off all drugs, as I feel that I keep taking all this awful, toxic medication yet nothing is working. My left hand is constantly swollen and my right hand is extremely disfigured. I dont have much pain, which is a good thing, but my main concern is that nothing is stopping the damage to my joints.
I know I’m lucky that it’s only in my hands but it really can render me useless at times. I’m afraid to pick up my grandson for fear of dropping him.
I’m at a loss as to what to do for the best. I just want something that works.
Rhona, via email – 2015
I wish you all the best in whatever decision you make.
Don’t Miss: Is Rheumatoid Arthritis Curable
Not All Patients With ‘early Polyarthritis’ Develop Persistent Disease
When a patient with inflammatory arthritis cannot definitely be labelled as having RA, it becomes important to decide whether the arthritis is likely to remit or to persist. Clearly, if spontaneous remission seems likely, the patient should be spared potentially toxic DMARD therapy. On the other hand, a patient with persistent inflammation should be started promptly on DMARDs since the condition may represent RA in evolution. From the Norfolk Arthritis Register there is evidence that an overwhelming majority of patients with persistent polyarthritis in due course come to satisfy diagnostic criteria for RA . Thus, since joint damage and functional loss occur early, most patients develop these irreversible changes before a definite diagnosis of RA can be made.
How can the clinician predict persistence of disease? Several research groups have tried to identify pointers in patients with early arthritis but their results are not easily combined because of heterogeneity in populations, predictive factors used and duration of follow-up. Among the predictive factors suggested, the most useful seems to be disease duration exceeding 12 weeks: a patient who has had inflammatory joint symptoms for this long is very unlikely to experience a spontaneous remission. Other features suggesting the unlikelihood of remission are positive tests for rheumatoid factor or cyclic citrullinated peptide antibodies and the presence of erosions on radiographs.
How Is Early Rheumatoid Arthritis Diagnosed
It can be difficult to diagnose rheumatoid arthritis early on in the disease. In the first few weeks and months, the symptoms are often mild and not always typical. But it’s important to diagnose the disease as soon as possible: The treatment is more likely to stop rheumatoid arthritis from getting worse if it is started early enough.
Some of the non-specific symptoms of early rheumatoid arthritis include general weakness, exhaustion, tiredness and weight loss. Other early signs include a slight fever, as well as achy bones and muscles. But people might also experience more typical rheumatoid arthritis symptoms such as swollen joints.
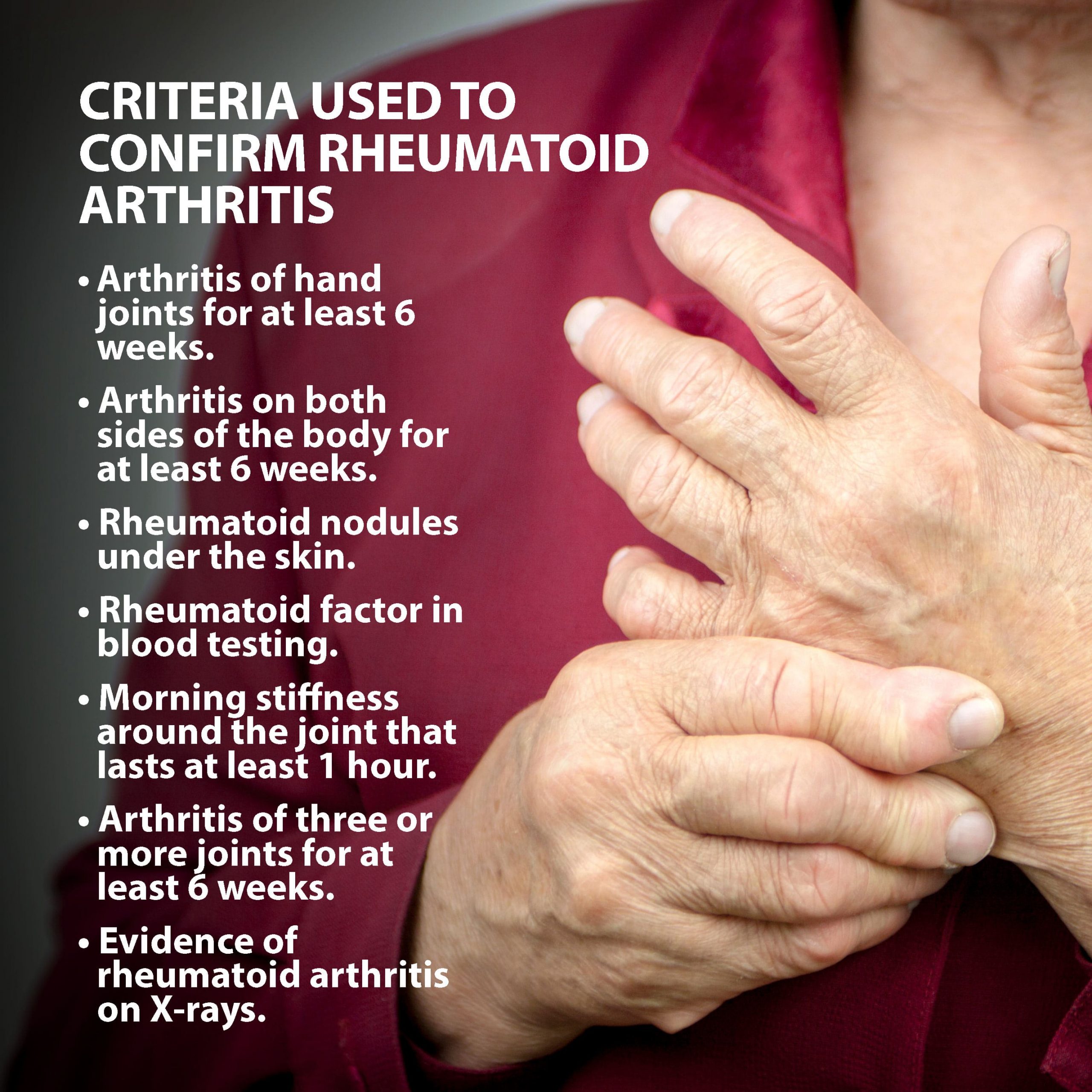
Tests specifically for rheumatoid arthritis will be recommended at the latest if
- three or more joints have been swollen for at least six weeks,
- the same joints are swollen on both sides of the body, and/or
- your joints feel stiff for at least one hour after getting out of bed in the morning.
Recommended Reading: What Does Arthritis Do To You
Getting Tested For Rheumatoid Arthritis
Testing for rheumatoid arthritis is ordered by a doctor or specialist if indicated by a patients symptoms. Blood and urine samples used for testing can be obtained in a doctors office or other medical setting.
Synovial fluid is a liquid that is located in spaces between a persons joints, helping to cushion ends of bones and reduce friction during movement. For a synovial fluid analysis, a sample of synovial fluid is obtained during a procedure called a joint aspiration or arthrocentesis. During a joint aspiration, a doctor uses a needle to withdraw a sample of synovial fluid from a joint.
How Is Seronegative Rheumatoid Arthritis Diagnosed
Some patients still have RA but do not test positive for either anti-CCPs or RF they have seronegative RA.
Annals of the Rheumatic Diseases
Your doctor may also conduct a synovial biopsy, which involves removing a small piece of the tissue lining one of your joints.
RELATED: Psoriatic vs Rheumatoid Arthritis: Whats The Difference?
You May Like: Medical Term Arthritis
What Are The Mortality Rates Among Canadians With Or Without Rheumatoid Arthritis
Between 20072008 and 20162017, age-standardized all-cause mortality rates decreased among females with diagnosed rheumatoid arthritis and among males with diagnosed rheumatoid arthritis . Mortality rates were consistently higher among males compared to females.
Over the surveillance period, the age-standardized all-cause mortality rate ratios were relatively stable ranging from 1.7 to 1.6 in females and from 1.5 to 1.7 in males. While rate ratios were similar among females and males, they showed an increase in mortality risk among those with diagnosed rheumatoid arthritis.
Figure 4: Age-standardizedFootnote e all-cause mortality rates and rate ratios among Canadians aged 16 years and older with and without diagnosed rheumatoid arthritis , Canada,Footnote f from 20072008 to 20162017
- Footnote e
| 1.7 |
Talk To Others Who Understand
Members of myRAteam know that having a team of others who understand life with rheumatoid arthritis can make all the difference. They regularly ask questions, give advice, and share stories about living with and managing RA.
Do you experience hot flashes, sweating, or overheating with RA? If youve found a way to manage it, let other members know in the comments below or by starting a new conversation thread.
Also Check: Rheumatoid Arthritis Arm Pain
Blood Tests For Rheumatoid Arthritis
RA is an autoimmune disease. Several blood tests can detect immune system changes or antibodies that may attack the joints and other organs. Other tests are used to measure the presence and degree of inflammation.
For blood tests, your doctor will draw a small sample from a vein. The sample is then sent to a lab for testing. Theres no single test to confirm RA, so your doctor may order multiple tests.
Can Climate And Environment Affect Osteoarthritis
Q) My son suffers from a serious back injury he sustained while serving in the army. He’s had several operations and was told that, in the future, he may well suffer from arthritis in his spine as a result.
Is there an area of the country that has a lower incidence of the condition, or does climate and the environment have no bearing?
Susan – 2018
A) Im sorry to hear about your sons injury. The risk of osteoarthritis in a joint is increased when you have a history of injury to that joint, including the spine. Moving to a different location with a different climate wont alter the risk of developing osteoarthritis or slow the progression of the condition.
The debate around whether warm climates improve symptoms of osteoarthritis, such as stiffness and pain, continues. Warm weather may have a small impact on improving symptoms, but unfortunately it doesnt stop you from getting the condition.
This answer was provided by Dr Tom Margham in 2018, and was correct at the time of publication.
Also Check: Aching Arms And Hands Rheumatoid Arthritis
How Can Rheumatoid Arthritis Be Managed
The specific causes of rheumatoid arthritis are unknown, but there are a number of factors associated with an increased risk of developing the disease including family history, smoking, increased age and occupational exposures.Footnote 4Footnote 5 While there is no cure for rheumatoid arthritis, there are treatment options which aim to alleviate joint symptoms and improve function. Individuals often work with a rheumatologist to develop a treatment plan to prevent further joint damage. Medication is often prescribed as a first line of therapy and is key to controlling disease and preventing damage. Other ways to manage include physical therapy, occupational therapy and education.Footnote 6 Individuals with rheumatoid arthritis who are diagnosed and treated early are less likely to experience long-term joint damage and functional impairments.
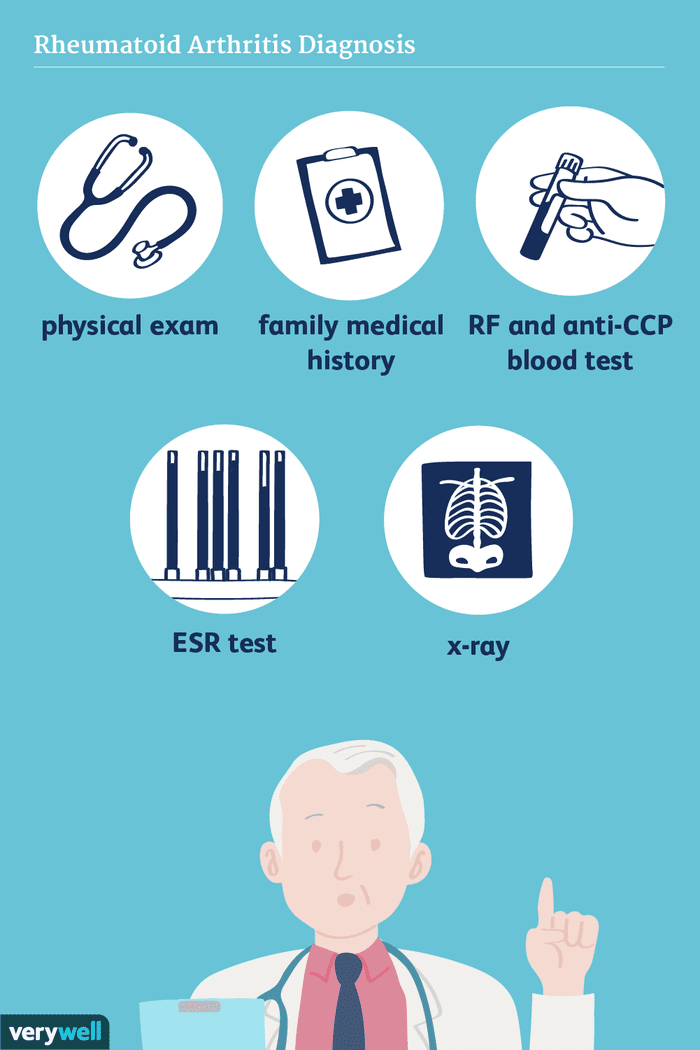
Physical Exam And Medical History
The appointment will likely begin with the physician taking a thorough medical history. This will include asking the patient several questions, such as:
- What joints are affected?
- How would you describe the pain?
- Do you have morning stiffness?
- Have you noticed increased fatigue or weight changes?
- Have you experienced other symptoms besides joint pain?
- When did symptoms begin?
- How have symptoms changed over time?
- What movements or activities make the patient feel better or worse?
The history will also include a review of the patients:
- Other medical problems
See Lifestyle Factors and Fatigue Associated with Rheumatoid Arthritis
During the physical exam, a doctor will evaluate the patients general health and then examine the joints, looking for signs of joint inflammation. For example, a doctor may measure a joints range of motion, press the skin over a joint to see if it causes pain, and test joint strength.
You May Like: How To Cope With Arthritis
Contact The Center For Arthritis And Joint Diseases
To learn more about our services or to make an appointment with a Brigham and Womens Hospital rheumatologist, contact one of our trained coordinators at 1-800-294-9999 to get connected with the best doctor for your needs.
Our expert rheumatologist, Daniel Solomon, MD, discusses the various treatment options for rheumatoid arthritis at Brigham and Women’s Hospital and how treatment modules are evolving through vigorous research.
Our expert rheumatologist, Michel Weinblatt, MD, has been involved in research for rheumatoid arthritis treatments for the past forty years. Find out how Brigham and Women’s is at the forefront of innovative treatment for rheumatoid arthritis.