A Final Word From Creakyjoints
If youre diagnosed with rheumatoid arthritis, youll likely have many questions about next steps and starting treatment. Our downloadable guidelines,A Patients Guide to Living with Rheumatoid Arthritis, provide key info you need to know.
You can also , to start tracking your RA symptoms and have the opportunity to participate in voluntary research studies.
How Does Treatment Improve Life Expectancy
Early treatment greatly improves the prognosis of RA patients. If treatment begins before symptoms cause too much damage, patients can generally go on to live a better quality of life.
Ongoing treatment and monitoring can help rheumatologists provide the most appropriate and personalized care for their patients. Each patient will experience a different set of symptoms over their lifetime. Doctors look for warning signs of other complications associated with RA and work to either prevent them or treat them as they develop.
The main goal of treatment is to reduce pain and improve quality of life. Many patients experience very effective treatment plans and continue to live their lives making appropriate lifestyle adjustments along the way.
Other Diagnostic Methods Used To Confirm Rheumatoid Arthritis
Blood tests arent the only method that can be used to diagnose rheumatoid arthritis. You might also have a variety of other tests done to help confirm rheumatoid arthritis. These include:
- Physical assessment. A physical assessment can help determine how much your symptoms are impacting your daily life. You might be asked how well you can do daily tasks such as showering, eating, and dressing. A physical therapist might also assess your grip, walk, and balance.
- Joint scan. A joint scan looks for inflammation and damage in your joints. It can help confirm a rheumatoid arthritis diagnosis.
- Imaging tests. X-rays and MRIs create detailed pictures of your bones, muscles, and joints that can help diagnose rheumatoid arthritis.
Read Also: Can Someone With Rheumatoid Arthritis Donate Blood
Serologic Testing For Ra
RF and/or anti-CCP antibodies may be positive in people with RA, leading to what’s referred to as “seropositive RA.” However, approximately 20% of people with RA will not have either a positive RF or CCP antibody, thus having “seronegative RA.” Seropositive RA is associated with more aggressive disease.
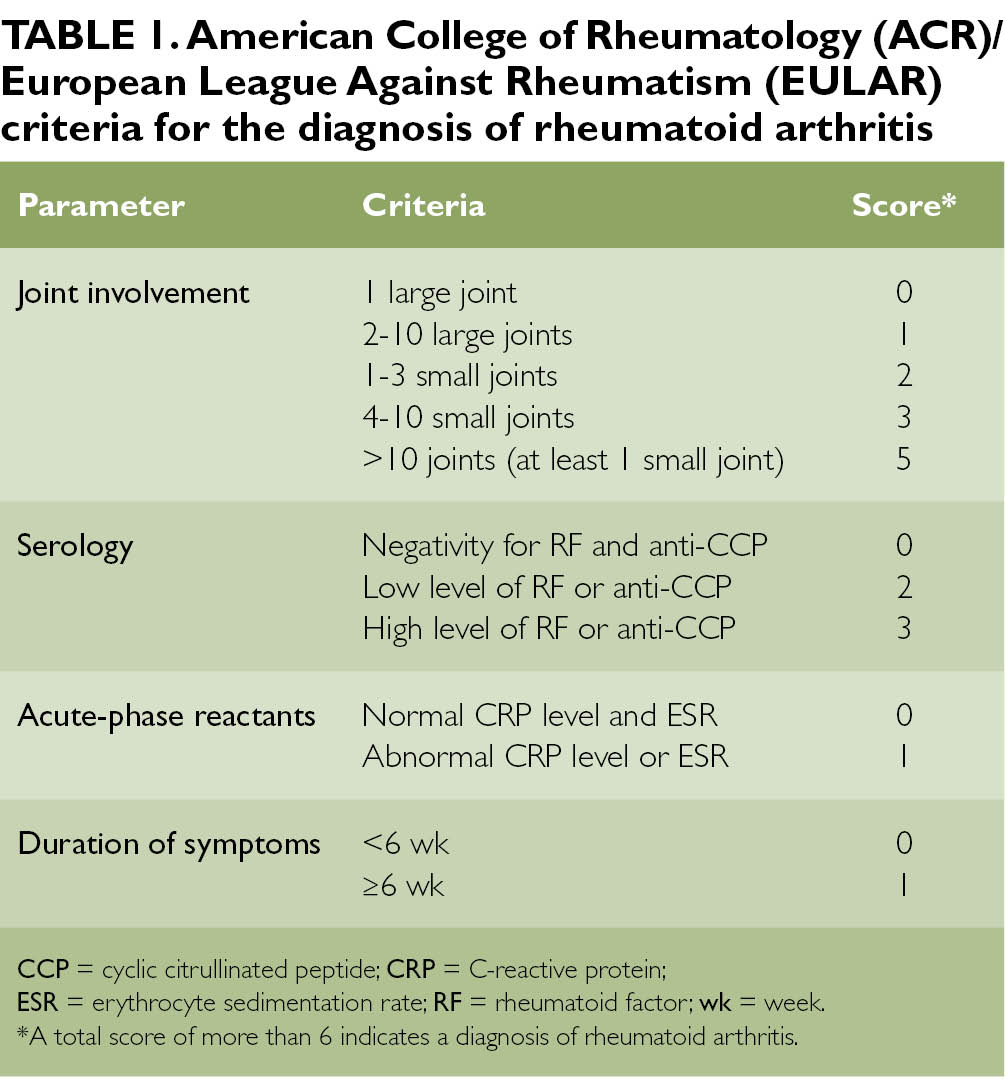
Finally, since RA is a systemic inflammatory condition, it is only natural that inflammatory markers such as the erythrocyte sedimentation rate and C-reactive protein , may be elevated at various times throughout the disease. Elevation in either the ESR or CRP is included in the 2010 EULAR/ACR diagnostic criteria for RA and can be used to monitor and gauge disease activity.
Once adequate and appropriate management is achieved, these markers should return to normal.
A Healthy Lifestyle With Ra
Living a healthy life is an integral part of managing RA. The daily lifestyle strategies you implement help you maintain your physical and mental health, prevent disease complications, and protect and strengthen your joints.
People who live with long-term conditions like RA benefit when they prioritize a healthy lifestyle. They can live longer, have a better quality of life, remain independent, and continue to be active even years and decades later after their diagnoses.
You May Like: Can Vitamin D Help Arthritis
Reaching A Ra Diagnosis
Once all of these steps have been conducted, doctors will look at all of the test results and reach a conclusion based on the overall picture. Some doctors take a more symptom based approach to diagnosing RA while others rely on blood tests and medical history to confirm a RA diagnosis.
This is why its possible to be diagnosed with RA but not test positive for antibodies or have a medical history of RA in your family. If the symptoms themselves are consistent with RA, then it can still be diagnosed.
That being said, the main criteria for diagnosing RA do not change. The patient must exhibit symptoms for greater than six weeks, symmetrical symptoms, as well as multiple joints being affected including fingers and hands.
Duration Of Rheumatoid Arthritis
But remission doesn’t happen for everyone, and because the pain and other symptoms of RA may change over time, pain management can be an ongoing concern. In addition to pain medications like nonsteroidal anti-inflammatory drugs and corticosteroids, there are many options for pain relief for people living with RA. These include, among others:
Read Also: What Foods Not To Eat If You Have Rheumatoid Arthritis
Rheumatoid Factor And Anti
One blood test measures levels of rheumatoid factors in the blood. Rheumatoid factors are proteins that the immune system produces when it attacks health tissue.
About half of all people with rheumatoid arthritis have high levels of rheumatoid factors in their blood when the disease starts, but about 1 in 20 people without rheumatoid arthritis also test positive.
A related blood test known as anti-cyclic citrullinated peptide test is also available. Anti-CCPs are antibodies also produced by the immune system.
People who test positive for anti-CCP are very likely to develop rheumatoid arthritis, but not everybody with rheumatoid arthritis has this antibody.
Those who test positive for both rheumatoid factor and anti-CCP may be more likely to have severe rheumatoid arthritis requiring higher levels of treatment.
What Happens In A Joint Affected By Rheumatoid Arthritis
If you have rheumatoid arthritis, your immune system can cause inflammation inside a joint or a number of joints. Inflammation is normally an important part of how your immune system works. It allows the body to send extra fluid and blood to a part of the body under attack from an infection. For example, if you have a cut that gets infected, the skin around it can become swollen and a different colour.
However, in the case of rheumatoid arthritis, this inflammation in the joint is unnecessary and causes problems.
When the inflammation goes down, the capsule around the synovium remains stretched and cant hold the joint in its proper position. This can cause the joint to become unstable and move into unusual positions.
The following can play a part in why someone has rheumatoid arthritis:
You May Like: How Do I Get Tested For Rheumatoid Arthritis
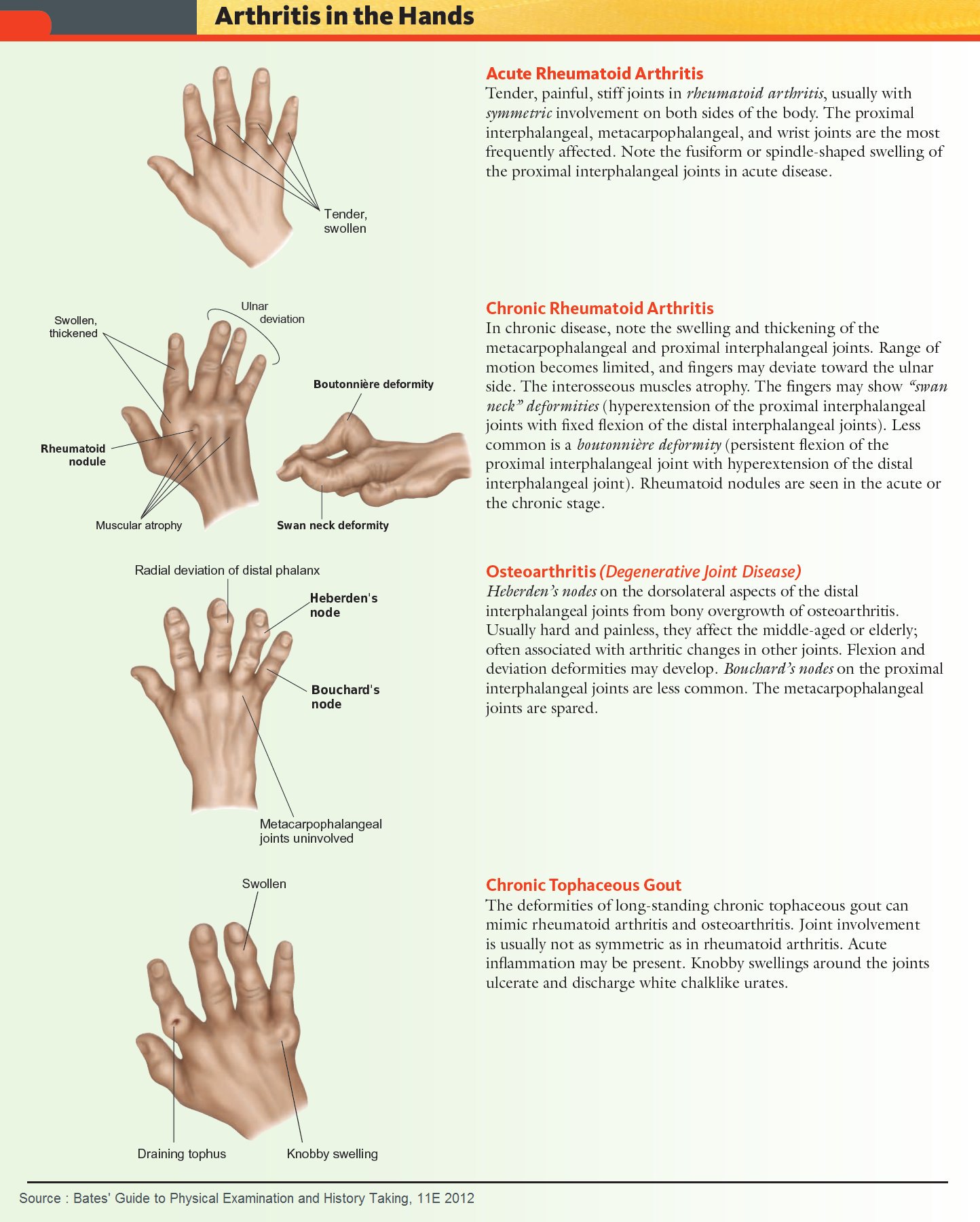
Telling The Difference Between Ra And Other Conditions
RA is often confused with other conditions that can cause joint pain, including:
- Inflammatory bowel disease and Crohns disease
- Palindromic rheumatism
- Reactive arthritis resulting from bacterial infection
Many of these conditions cause overlapping symptoms, including joint pain and stiffness.
RA is also potentially confused with osteoarthritis, which causes pain and stiffness in the joints, but is caused by wear and tear, not inflammation from an immune response.
In order to distinguish RA from other autoimmune conditions, your doctor will likely perform a variety of diagnostic tests, including imaging of your joints, blood tests, and comprehensive physical exams. Your doctor may also recommend that you see a rheumatologist .
If you have persistent swelling, pain, or stiffness in your joints, its important to find a medical professional to diagnose your condition as soon as possible. Dignity Health provides comprehensive care for rheumatoid arthritis as part of our orthopedic services. Consult with a trained specialist at Dignity Health through our Find a Doctor tool.
The information contained in this article is meant for educational purposes only and should not replace advice from your healthcare provider.
Making A Diagnosis Of Rheumatoid Arthritis
Diagnosis of RA is not straight forward as there is no individual test for RA. A diagnosis tends to be made by a consultant rheumatologist on the basis of tests, examination and ruling out other possible causes for symptoms.
Sometimes it is clear from symptoms and initial blood tests that someone has rheumatoid arthritis, but not always. Specialist criteria have been developed jointly by American and European experts to try to help make a diagnosis of rheumatoid arthritis in people presenting with new-onset swollen, painful joints with no obvious cause . These should be used with care though as people with osteoarthritis or a crystal arthritis could meet the criteria and end up being incorrectly diagnosed with rheumatoid arthritis, which could have significant consequences for treatment. They have also been developed to classify, not diagnose, rheumatoid arthritis and so should not be used to decide who gets referred.
As already mentioned above, there are a number of other conditions that can cause very similar symptoms to rheumatoid arthritis and your GP will have to consider these when assessing each case.
Also Check: What Can Be Done For Arthritis In The Neck
Living With Rheumatoid Arthritis
Research shows that people who take part in their own care report less pain and make fewer doctor visits. They also enjoy a better quality of life.
Self-care can help you play a role in managing your RA and improving your health. You can:
- Learn about rheumatoid arthritis and its treatments.
- Use exercises and relaxation techniques to reduce your pain and help you stay active.
- Communicate well with your health care team so you can have more control over your disease.
- Reach out for support to help cope with the physical emotional, and mental effects of rheumatoid arthritis.
Participating in your care can help build confidence in your ability to perform day-to-day activities, allowing you to lead a full, active, and independent life.
Treatment And Medication Options For Rheumatoid Arthritis
To treat RA, doctors aim to stop the progression of the disease by reducing symptoms, controlling inflammation, minimizing joint and organ damage, and improving physical function.
Proven treatments include medication and physical therapy. Early, aggressive measures can help control symptoms and complications before the disease significantly worsens, by reducing or altogether stopping inflammation as quickly as possible.
You May Like: How Often Can You Get Steroid Injections For Arthritis
Reviewing Your Risk Factors
Your doctor may suspect you’re dealing with rheumatoid arthritis if youre a woman because about 75% of people who are diagnosed with RA are female. Some women are diagnosed with RA early, in their 20s or 30s, but a number are diagnosed later, in their 50s or 60s. Men who are diagnosed tend to be older. If you have first-degree family members who have been diagnosed with RA, tell your doctor, because that increases your risk as well.
What Types Of Lifestyle Changes Can Help With Rheumatoid Arthritis
Having a lifelong illness like rheumatoid arthritis may make you feel like you dont have much control over your quality of life. While there are aspects of RA that you cant control, there are things you can do to help you feel the best that you can.
Such lifestyle changes include:
Rest
When your joints are inflamed, the risk of injury to your joints and nearby soft tissue structures is high. This is why you need to rest your inflamed joints. But its still important for you to exercise. Maintaining a good range of motion in your joints and good fitness overall are important in coping with RA.
Exercise
Pain and stiffness can slow you down. Some people with rheumatoid arthritis become inactive. But inactivity can lead to a loss of joint motion and loss of muscle strength. These, in turn, decrease joint stability and increase pain and fatigue.
Regular exercise can help prevent and reverse these effects. You might want to start by seeing a physical or occupational therapist for advice about how to exercise safely. Beneficial workouts include:
- Range-of-motion exercises to preserve and restore joint motion.
- Exercises to increase strength.
- Exercises to increase endurance .
You May Like: How Bad Can Arthritis Get
Ra Life Expectancy: Does Rheumatoid Arthritis Affect Life Span
The predicted life expectancy of a patient diagnosed with rheumatoid arthritis is problematic to accurately calculate due to the vast amount of unpredictable variables involved. As a chronic disease, RA tends to be progressive. In other words, it is a long-term disease in which symptoms tend to accumulate over time. This accumulation results in an overall worsening of the patients symptoms. Presently, doctors do not know what causes nor triggers the disease. That being said, they suspect it is likely initiated by a combination of factors including genetics and environmental influences.
Because there isnt one specific cause of the disease, there is also no known cure for RA. Todays medical technology and research, however, provide a variety of treatment options, which can prolong the lives of patients, slow the progression of disease, and provide some symptom relief.
These are just some of the factors which make it difficult to predict an exact life expectancy for RA patients. What research has found is that it isnt the disease itself which reduces the life expectancy of patients. Its the varying complications that develop as a result of the disease which cause life expectancy to shorten. For example, RA can cause respiratory and cardiovascular conditions which can compound over time and lead to a shortened lifespan and possibly eventual fatality.
Comparison Of Imaging Parameters
All imaging was performed using a hybrid PET/CT scanner . Patients were instructed to fast for more than 5 h before FDG administration. FDG-PET/CT imaging was visually assessed by two board-certified nuclear medicine physicians working independently. Any difference of opinion was resolved by consensus. Visually abnormal FDG uptake seen in locations unaccounted for by the normal biodistribution of FDG was interpreted as lesion. A board-certified nuclear medicine physician performed the semiquantitative analyses. Lesion boundaries of voxels were determined using a fixed SUV threshold of2.5, as used in a previous report. Any FDG uptake by arthritic tissue was excluded. The maximum SUV , mean SUV , and peak SUV were calculated. The highest SUVmax, SUVmean, and SUVpeak among all the lesions showing FDG uptake were evaluated for each patient. MTV was defined as the lesion volume where the SUV exceeded a threshold value. TLG was calculated by multiplying the MTV by the SUVmean. The sums of the MTV and TLG of all lesions within a patient were defined as MTVsum and TLGsum, respectively. These imaging parameters were calculated using an open-source software tool developed for the efficient measurement of tumor volume on FDG-PET/CT.
Don’t Miss: Can I Take Tylenol Arthritis With Xarelto
How Your Doctor Can Tell If You Have Rheumatoid Arthritis
After testing is finished, your doctor will decide if you have RA. But before that, they will need to rule out other conditions that can mimic RA. It is important to rule out these other diagnoses because they often require a different treatment strategy. These conditions include:5
- Osteoarthritis, a type of arthritis in which the protective tissue at the ends of bones begin to break down
- Psoriatic arthritis, a type of inflammatory arthritis that is often associated with psoriasis
- Polymalagia rheumatica, a disorder that causes inflamed muscles around the shoulders and hips
- Infectious arthritis, an infection in the joint
In order to rule out these other diagnoses, your doctor will use a set of RA criteria established by scientific study and real-world practice. Here are the signs, symptoms, and test results your doctor will look for:2
- At least 2 joints impacted by inflammatory arthritis, including the shoulders, elbows, hips, knees, and ankles
- Smaller joints affected by inflammatory arthritis
- A positive result on a rheumatoid factor or CCP antibody test
- Higher CRP or sed rate levels
- Symptoms for 6 weeks or longer
Keep in mind that you may not meet all of these criteria, but your doctor could still diagnose you with RA.2
What Is Rheumatoid Arthritis
Rheumatoid arthritis, or RA, is an autoimmune and inflammatory disease, which means that your immune system attacks healthy cells in your body by mistake, causing inflammation in the affected parts of the body.
RA mainly attacks the joints, usually many joints at once. RA commonly affects joints in the hands, wrists, and knees. In a joint with RA, the lining of the joint becomes inflamed, causing damage to joint tissue. This tissue damage can cause long-lasting or chronic pain, unsteadiness , and deformity .
RA can also affect other tissues throughout the body and cause problems in organs such as the lungs, heart, and eyes.
Recommended Reading: Can You Get Arthritis From Popping Your Knuckles
Focus On The Rheumatoid Arthritis Patient Not On Their Disease
Medical school, residency, and fellowship taught me pathophysiology, diagnosis, and the most advanced treatments for autoimmune diseases like rheumatoid arthritis. As an attending physician, seeing my own patients, I noticed that targeted therapy is not able to control the disease in all patients with rheumatoid arthritis. The results varied. I could not stop asking myself, why is it so different?
In my previous article, I wrote about one of my patients stories as well as my discovery journey of integrative medicine. After taking a nutrition science course at Stanford University, a mindfulness training program at the University of Massachusetts, and doing a lot of research, I started to recognize the vital role of nutrition in managing my rheumatoid arthritis patients. However, to have the most optimal outcomes, we must discuss with patients about essential lifestyle changes. Despite acknowledging the role of lifestyle changes, many physicians will not have time to properly educate patients or are not properly rewarded by the current traditional billing/coding system.
Nutrition: the key to decreasing inflammation
Exercise: Modulating effects on mood and chronic pain
Sleep for rheumatoid arthritis patients
Mindfulness: the power of the mind to control chronic pain
I teach patients how to approach pain and how to incorporate simple breathing techniques, guided imagery, or other relaxation techniques. Less pain translates into better sleep and quality of life.
Summary
Whats The Normal Sed Rate For Rheumatoid Arthritis
Sed rate is a blood test that helps detect inflammation in your body. Your healthcare provider may also use this test to watch how your RA progresses. Normal sed rates are as follows:
| People designated male at birth | Erythrocyte sedimentation rate |
|---|---|
| > 50 years old | 30 mm/hr |
In rheumatoid arthritis, your sed rate is likely higher than normal. To take part in clinical trials related to rheumatoid arthritis, you usually need an ESR of 28 mm/hr. With treatment, your sed rate may decrease. If you reach the normal ranges listed above, you may be in remission.
You May Like: Does Paraffin Wax Treatment Help Arthritis