What Is A Subcutaneous Injection
Many PsA medications are administered through subcutaneous injection. These medications are injected through a needle and into a layer of fat underneath the skin that is called subcutaneous fat. Injecting the medication into this layer of fat allows the body to absorb the medication slowly and gently.
Subcutaneous injections are usually administered into areas of the body that have wide layers of fat, such as the upper arm, the thigh, or the abdomen. You may be able to perform subcutaneous injections at home, or you can book an appointment with your health care provider to receive an in-office injection.
Types And Side Effects
The most common DMARDs for PsA are:
- methotrexate
- hydroxychloroquine
Methotrexate
Methotrexate is an immunosuppressive drug that treats psoriasis. It also works well for PsA and can help prevent damage to joints. Rarely, methotrexate can cause liver damage, so a person will need to see their doctor regularly for tests.
Sulfasalazine
Sulfasalazine is a type of sulfa drug that has powerful anti-inflammatory effects. People who are allergic to sulfa drugs cannot take it. It helps prevent joint swelling, inflammation, and damage that PsA causes.
Leflunomide
Although this is a rheumatoid arthritis drug, some doctors prescribe it for PsA. It may cause diarrhea in up to 20 percent of people.
Cyclosporine
Cyclosporine is an immunosuppressant that helps treat autoimmune conditions. Side effects include high blood pressure, headache, and stomach pain.
Antimalarial treatment
Certain drugs that treat malaria can help with PsA. Results may take several months, however. Side effects include headaches, dizziness, nausea, vomiting, and vision changes.
Acthar
Acthar is an injectable medication that can help the body make its own steroid hormones, which helps lower inflammation. Acthar is useful for fast relief of severe inflammation and swelling.
Azathioprine
Azathioprine is a drug that suppresses the immune system, which helps with both PsA and skin psoriasis.
Newer Drug Treatments For Psoriatic Arthritis
Get more information about the medications, ustekimumab, apremilast and abatacept that were approved by the FDA as options for treating PsA.
Psoriatic arthritis is a chronic, autoimmune, inflammatory form of arthritis that causes painful, swollen joints, as well as the skin symptoms associated with psoriasis. Approximately 30 percent of people with psoriasis develop PsA in addition to their skin condition. The goal of treatment is to improve both joint and skin symptoms and prevent or minimize permanent joint damage.. While there are a variety of treatments available, many PsA patients are undertreated, making newer drug approvals important to give doctors and patients more options. Depending on its severity, psoriatic arthritis is typically treated with nonsteroidal anti-inflammatory drugs , corticosteroids and conventional disease-modifying anti-rheumatic drugs such as methotrexate. Biologics such as adalimumab , etanercept , golimumab and infliximab are used when other treatments fail to bring relief or as part of an aggressive treatment strategy. The U.S. Food and Drug Administration approved three new drugs between 2013 and 2017 for use in psoriatic arthritis:
Don’t Miss: How To Soothe Arthritis Pain
Where Research Is Now
Psoriatic arthritis is a multifaceted disease that affects both the skin and joints. Researchers are currently working to understand the causes of PsA and the multiple ways it affects the body. Other studies are working to identify biomarkers for PsA that can be used to predict a persons response to certain medications. Also, new medications may be developed that can better treat the disease and promote long-term remission.
The knowledge gained from this research may lead to better diagnostics, improved treatments, ways to prevent PsA, and a potential cure. For now, the goal is to help PsA patients achieve long-term remission.
Your Disease Seems To Be In Remission

Your psoriatic arthritis treatment is working, so you feel little or no joint pain and have minimal swelling. So, you might think, why continue taking your medication? Well, if you stop, you risk your symptoms returning. A small study published in April 2015 in the journal Annals of the Rheumatic Diseases found that 77 percent of people who stopped their disease-modifying antirheumatic drugs or biologics reported that their disease returned within three to six months. People with longer duration of psoriatic arthritis or more severe disease have the highest risk of recurrence. The Arthritis Foundation recommends you continue to take your medication even if you have low disease activity. But you can talk to your doctor about potentially lowering your dose or stopping one medication if you currently take several medications.
Also Check: How Much Curcumin Should I Take For Arthritis
Your Psoriatic Arthritis Treatment Options
There are many treatments that may give you relief, so its important to talk with your doctor to find the right one. The type of psoriatic arthritis you have, its severity, and your reaction to treatment will help determine what treatment is best for you.
Some options for treatment include:
- Nonsteroidal Anti-Inflammatory Drugs : Over-the-counter medications like aspirin and ibuprofen, but can also include prescription products, which help to reduce inflammation, joint pain, and stiffness
- Disease-Modifying Antirheumatic Drugs : Typically for more severe symptoms, these attempt to slow or stop joint/tissue damage and the progression of psoriatic arthritis
- Biologics: Protein-based medicines produced from living cells that target specific parts of the immune system
“For people like me with psoriatic arthritis, I would tell them to go on the website, and do your research.”
– Patti, actual Taltz patient with psoriatic arthritis.
Patti was compensated for her time.
PURPOSE AND SAFETY SUMMARY
Important Facts About Taltz® . It is a prescription medicine also known as ixekizumab.
Taltz is an injectable medicine used to treat:
- People 6 years of age and older with moderate to severe plaque psoriasis who may benefit from taking injections or pills or treatment using ultraviolet or UV light .
- Adults with active psoriatic arthritis.
- Adults with active ankylosing spondylitis.
- Adults with active non-radiographic axial spondyloarthritis with objective signs of inflammation.
WARNINGS
Odds Of Going Into Remission
Remission in PsA means that there are no signs of disease activity, including inflammatory blood markers and symptoms. In PsA, the two types of remission are:
- Drug-induced: Low disease activity when you are actively taking medications, such as biologics
- Drug-free: Low disease activity, relief from symptoms without medication, or both
The standard treatment approach for PsA is a treat to target strategy, with the goal being minimal disease activity. This typically involves adjusting medication over time to achieve remission. The process is ongoing and may require you to have close contact with your healthcare provider over time so they can closely monitor your condition and responses to medication. They may adjust your therapies/medications so you can achieve remission or low disease activity.
You and your healthcare provider will come up with a treatment plan to get you into remission. How quickly remission occurs depends on how mild or severe your PsA is. Most experts agree that an early and accurate diagnosis and starting treatment as early as possible increase the chances of remission and make it last.
You May Like: Inflammatory Arthropathy Symptoms
Don’t Miss: How To Apply Dmso For Arthritis
Yes This Information Is Right For You If
- Your doctor has told you that you have psoriatic arthritis .
- This is a type of arthritis that affects people with psoriasis .
- Psoriasis is an ongoing skin condition that causes red, scaly patches on your body.
Biologics: Another Type Of Dmard
Biologics are a different type of DMARD. People must take them via injection or intravenous drip.
Up to 60 percent of people may achieve remission after 1 year of treatment with biologics, according to the Arthritis Foundation. Remission means that there is minimal disease activity, or the disease is not causing serious symptoms or joint damage.
Don’t Miss: How To Treat Arthritis Pain In Fingers
Dendritic Cells And Macrophages
Immature and mature dendritic cells and macrophages are present in inflammatory infiltrates of skin and synovium of patients with psoriasis and PsA, where they present antigens to T cells, remove necrotic/apoptotic cells, and most importantly, they can be a source of a multitude of cytokines and chemokines such as CCL19. Several regulatory molecules are involved in this process, such as intercellular adhesion molecule 1 , lymphocyte function-associated antigen 3 and cluster differentiation -80/86 in DCs and LFA-1, CD2 and CD28 in T cells. In addition, plasmacytoid DCs , a main source of type I interferon , are also present in the skin. Myeloid dermal DCs are also increased in psoriatic lesions and induce autoproliferation of T cells as well as production of type 1 helper T cell cytokines. Keratinocytes are responsive to DC-derived and T-cell-derived cytokines, including IFNs, tumor necrosis factor , interleukin -17, and IL-20 family of cytokines, and in turn they produce proinflammatory cytokines and chemokines . Participation of cell-mediated immune responses in the pathogenesis of PsA is suggested by the demonstration in synovial fluid and peripheral blood lymphocytes of different natural killer surface markers and / T-cell receptor antigen . Endothelium may also play a role in the pathogenesis of longstanding PsA as evidenced by the increased expression of certain adhesion molecules in PsA synovium related to the disease duration .
What Are Immunosuppressants
Immunosuppressants are medications that turn off a piece of the immune system in order to decrease inflammation. An overactive immune system causes inflammation in PsA, so it makes sense that medications to treat it turn off a part of the immune system.
Immunosuppressants come in all different forms pills, injections, and infusions. They fit into three general categories: disease-modifying antirheumatic drugs , biologics, and small molecules.
You May Like: How To Determine Rheumatoid Arthritis
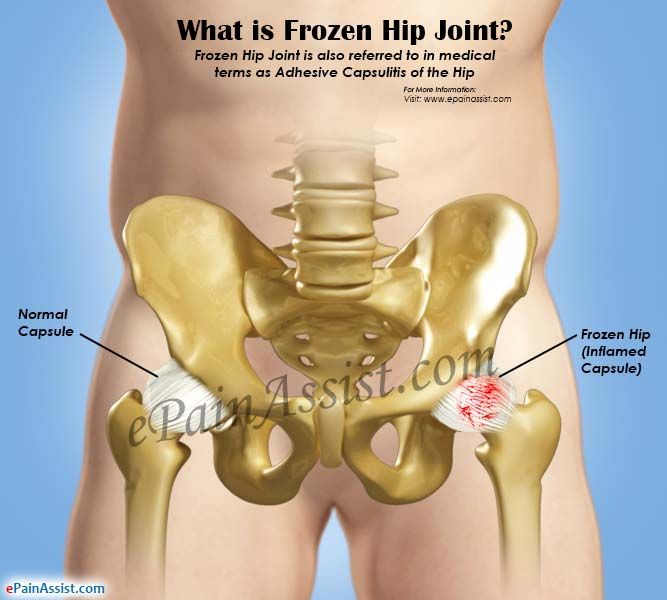
Sex Fertility And Pregnancy
Sex can sometimes be painful for people with psoriatic arthritis, particularly a woman whose hips are affected. Experimenting with different positions and communicating well with your partner will usually provide a solution.
Psoriatic arthritis wont affect your chances of having children. But if youre thinking of starting a family, its important to discuss your drug treatment with a doctor well in advance. If you become pregnant unexpectedly, talk to your rheumatology department as soon as possible.
The following must be avoided when trying to start a family, during pregnancy and when breastfeeding:
What Dietary Changes Can Help With Psoriatic Arthritis
There are no specific foods to eat or avoid if you have PsA. But a healthy diet will help you maintain a healthy weight and decrease your risk of heart disease. PsA increases heart disease risk due to inflammation, so a healthy diet is a win-win approach.
Of note, certain foods or drinks may cause psoriasis flares in some people. If thats true for you, its a good idea to avoid those if you have PsA, too.
Recommended Reading: What Is Humira For Rheumatoid Arthritis
Basics Of Psoriatic Arthritis
PsA is a type of inflammatory arthritis that often affects people who already have the inflammatory skin condition psoriasis.
Psoriasis is known for causing patches of red, inflamed skin with white, silvery flakes. PsA affects up to 30% of people with psoriasis.
Joint pain, stiffness, and swelling are the main symptoms of PsA. These symptoms can affect any part of the body, including the fingers and spine, and symptoms range from mild to severe.
PsA, much like psoriasis, causes periods of flare-ups and periods of remission .
There’s no cure for PsA. Healthcare providers focus on controlling symptoms and preventing joint damage. Without treatment, PsA can lead to permanent damage and disability.
Biologics are a type of disease-modifying anti-rheumatic drug designed to manage PsA symptoms and slow down PsA disease progression.
Researchers consider biologic drugs to be the most targeted therapies for treating PsA.
Traditional DMARDs, like methotrexate, suppress the entire immune system. Biologics only target parts of the immune system that are linked to PsA. This includes immune cells and inflammatory proteins such as:
- T-cells
- Interleukins 12, 17, and 23
These cells and proteins play a significant part in the development and progression of PsA and psoriasis.
Work And Psoriatic Arthritis
Having psoriatic arthritis may make some aspects of working life more challenging. But, if youre on the right treatment, its certainly possible to continue working.
Help and support is available, and you have rights and options.
The Government scheme Access to Work is a grant that can pay for equipment to help you with activities such as answering the phone, going to meetings, and getting to and from work.
The 2010 Equality Act, and the Disability Discrimination Act in Northern Ireland makes it unlawful for employers to treat anyone with a disability less favourably than anyone else. Psoriatic arthritis can be classed as a disability if its making every-day tasks difficult.
Your employer may need to make adjustments to your working environment, so you can do your job comfortably and safely.
You might be able to change some aspects of your job or working arrangements, or train for a different role.
In order to get the support youre entitled to, youll need to tell your employer about your condition. Your manager or HR department might be a good place to start.
Other available support might include:
- your workplace occupational health department, if there is one
- an occupational therapist. You could be referred to one by your GP or you could see one privately
- disability employment advisors, or other staff, at your local JobCentre Plus
- a Citizens Advice bureau particularly if you feel youre not getting the support youre entitled to.
You May Like: Can You Get Disability For Arthritis In Your Knees
Living With Psoriatic Arthritis
Living with psoriatic arthritis is all about maintaining the right treatment plan. With the right treatment plan in place, you can live a life free of pain and inflammation. Most doctors prescribe a combination of therapies to patients with psoriatic arthritis. This can include drug therapies, home remedies, and lifestyle changes to increase mobility, treat psoriasis symptoms, and minimize joint pain.
Even though psoriatic arthritis is a lifelong, chronic, autoimmune disorder, this does not have to impact your quality of life. Get diagnosed early, have your doctor develop a treatment plan, and stick to it. These are the keys to living a healthy life with psoriatic arthritis.
Recommended Reading: Stop Arthritis In Fingers
Psoriatic Arthritis: Best Treatments For You
Alexandra Benisek
With psoriatic arthritis, each person’s symptoms and situation are unique. Your rheumatologist will work with you to find a treatment plan thatâs tailored to you specifically, rather than a “one-size-fits-all” approach.
Before starting treatment for psoriatic arthritis, doctors do a full evaluation of each patient. We look to see if they have joint involvement, spine involvement, nail or skin disease, and more. Once thatâs done, we come up with a medication regimen as well as nondrug ways to target your specific symptoms.
Usually, we start with nonsteroidal anti-inflammatory drugs or other anti-inflammatory medications. Then, there’s usually some form of immunosuppressive medication — drugs that keep an overactive immune system in check. Finally, we explore treatments like exercise, physical therapy, and weight loss, if needed.
Patient education is also important. Part of that is learning what the goal of treatment is, which is remission, meaning your disease is not active and you have no symptoms.
You May Like: How To Detect Psoriatic Arthritis
How Is Psoriatic Arthritis Diagnosed
To diagnose psoriatic arthritis, your doctor will probably first perform a physical exam to look for swollen joints skin or nail changes eye problems and joint tenderness.
You may be asked to undergo an X-ray, MRI, ultrasound, or CT scan, so your physician can get a better look at your joints.
Editor’s Picks
Lifestyle And Complementary And Alternative Medicine
Following your treatment plan can help reduce the signs and symptoms of PsA. Lifestyle changes and CAM may also help you manage and better cope with the disease, including:
- Anti-inflammatory diet: Eating a balanced diet rich in protein, fruits and vegetables may help with PsA symptoms. You may benefit from avoiding processed foods, dairy, sugar, and red meat.
- Exercise:Low- or no-impact exercises such as walking and swimming can help you stay physically active without placing too much demand on painful joints.
- Identify triggers:Certain foods, activities, and stress can trigger PsA flares. Keeping a symptom journal can help you identify your triggers and avoid them.
- Maintain a healthy weight: Staying within a healthy weight range helps reduce stress on your joints.
- Reduce stress: Stress can trigger PsA flares. Manage your stress levels by finding time to relax each day.
- Quit smoking:Smoking can worsen symptoms and may interfere with your bodys response to medication.
Many people with PsA turn to CAM options to help reduce symptoms. Consult with your healthcare provider before seeking out CAM options. There are many different alternative therapies to consider to complement your traditional treatment, including:
Everyone is different, so finding the treatments that are right for you may take time, trial, and error. Stay in close communication with your healthcare provider to find the treatments that are most effective for you.
You May Like: Is Apple Cider Vinegar Good For Arthritis Pain
What Are Biologic Dmards
Biologic DMARDs are drugs made from living cells. These cells can come from parts of the blood, proteins, viruses, or tissue. This process creates drugs that can prevent, treat, and cure disease. In people with PsA, they work by interfering with specific substances in the immune system to reduce or better regulate the inflammatory responses that cause PsA and psoriasis symptoms. Common proteins targeted include tumor necrosis factor and various interleukins . Biologic DMARDs include:2,5
- Cimzia®
Also Check: Best Remedy For Arthritis In Hands
Who Develops Psoriatic Arthritis
About 1 person in 10 with psoriasis develops psoriatic arthritis. About 2 in 100 people develop psoriasis at some stage in their lives.
In most cases, the arthritis develops after the psoriasis most commonly within 10 years after the psoriasis first develops. However, in some cases the arthritis develops much later. In a small number of cases the arthritis develops first, sometimes months or even years before the psoriasis develops. Men and women are equally affected.
Psoriasis most commonly first occurs between the ages of 15 and 25 and psoriatic arthritis most commonly develops between the ages of 25 and 50. However, both psoriasis and psoriatic arthritis can occur at any age, including in childhood.
Note: people with psoriasis also have the same chance as everyone else of developing other types of arthritis such as rheumatoid arthritis and osteoarthritis. Psoriatic arthritis is different, and is a particular type of arthritis that occurs only in some people with psoriasis.
Dont Miss: What Does Ra Feel Like
Read Also: What Is The Best Exercise For Arthritis