Does Lupus Lead To Kidney Disease
About one-third of patients with systemic lupus erythematosus develop kidney disease, known as .
Many cases of lupus involving the kidney are mild, and treatments have significantly improved, but up to 10% of patients with lupus nephritis can l develop kidney failure, with a need for dialysis and, possibly, a kidney transplant. About one-third of patients who start dialysis during an acute lupus flare will improve and be able to discontinue it within the first year. Patients with severe kidney disease and lupus need close follow-up with a rheumatologist and kidney specialist, since new treatments continue to be developed.
Get more detailed information about lupus from the articles and other content below, or select Treating Physicians to find the best rheumatologist at HSS for your particular condition and insurance. The offers multidisciplinary patient care, support and education.
Spinal Arthritis May Contribute To Other Issues In The Spine
Spinal arthritis may cause bone spurs overgrowths on the edges of the bones. In the spine, bone spurs particularly affect facet joints, making them grow larger. This condition is called facet joint hypertrophy. Although bone spurs on their own are not harmful, they may narrow the passages for the spinal cord and the nerves exiting the spine. This may lead to two painful conditions:
-
Spinal stenosis compression of the spinal cord inside the spinal canal
-
Radiculopathy pinching of the peripheral nerves as they exit the spine
Ankylosing spondylitis may also cause additional problems such as:
-
Stress fractures in places where new bone has formed
-
Collapsed vertebrae
-
A spinal deformity called kyphosis
Should I See A Doctor
Its common to have aches and pains in your muscles and joints from time to time. This may especially be true if you take part in unusual or strenuous physical activities.
So, how can you tell the difference between the early signs of arthritis and normal pain and stiffness? And, how do you know when you should see a doctor about your symptoms?
If you have swelling or stiffness that you cant explain and that doesnât go away in a few days, or if it becomes painful to touch your joints, you should see a doctor. The earlier you get a diagnosis and start the right type of treatment, the better the outcome will be.
Here are some other things to think about that might help you decide whether you need to see a doctor:
Recommended Reading: What Causes Arthritis In Legs
What Are The Symptoms Of Spinal Arthritis
Symptoms of spinal arthritis may differ from person to person. In general, they may include:
-
Back and neck pain, especially in the lower back
-
Stiffness and loss of flexibility in the spine, such as being unable to straighten your back or turn your neck
-
Swelling and tenderness over the affected vertebrae
-
Feeling of grinding when moving the spine
-
Pain, swelling and stiffness in other areas of the body
-
Whole-body weakness and fatigue
-
Pain and numbness in your arms or legs if the nerves are affected
Although back pain is a common symptom, not all people have it, even those with advanced spinal arthritis. On the other hand, some may experience pain even before arthritis can be seen on an X-ray.
In certain types of spondyloarthritis, eye inflammation may occur, causing pain, watery eyes and blurred vision.
Working With A Rheumatologist
A rheumatologist is a doctor who specializes in inflammatory arthritis.
These medical professionals can help people find the best treatment for their condition. Rheumatologists can also provide support and guidance, advising a person on how to manage the impact their condition may have on their quality of life.
Below are answers to some common questions about inflammatory arthritis.
Recommended Reading: How To Tell If Your Dog Has Arthritis
How Is Lupus Diagnosed
A diagnosis for lupus is generally based on laboratory tests that exclude other diseases which may have similar symptoms , and specific serologic tests blood tests that determine the presence of certain antibodies.
Patients with lupus characteristically have the following lab test results:
- Antibodies against their own cells. Almost all people with lupus test positive for antinuclear antibodies .
- Positive signs of one or more of the following, which may be present along with a positive ANA:
- anti-double-stranded DNA
- antiphospholipid antibodies antibody)
People with lupus sometimes also have false-positive test results for syphilis. This has nothing to do with the disease syphilis, and a more specific test for syphilis will be negative in people who have this test result.
Your Ra Healthcare Team
After youve been diagnosed with RA, a team co-ordinates your treatment along with yourconsultant rheumatologist. This combination of professionals is the key to effective treatment. The exact team will vary, depending on where you live and your needs, but you should expect to see some of the following people as part of your rheumatology care:
Arheumatology specialist nursecan help you learn about RA and your treatments, how to look after your joints, and how to have a healthy lifestyle. The nurse will be your first point of contact at the hospital.
Aphysiotherapistand/oroccupational therapistcan teach you how best to protect your joints and the best exercises to keep them moving. He or she may advise splints for severely affected joints. Evidence shows that staying active and exercising regularly is beneficial.
Generally, theGPworks together with others in the practice to provide support and reassurance to patients with long-term conditions, advising about self management and lifestyle issues as well as prescribing the recommended drugs, monitoring your blood tests and advising about pain management. TheGPsinvolvement in your care may vary from practice to practice.
If your feet are significantly affected, apodiatrist is an essential member of the team. He or she can advise you about looking after your feet and footwear and provide appropriate insoles for your shoes.
Also Check: Can Arthritis Be In Your Muscles
How Is Arthritis Treated
Theres no cure for arthritis, but there are treatments that can help you manage the condition. Your treatment plan will depend on the severity of the arthritis, its symptoms and your overall health.
Conservative treatments include:
- Medication: Anti-inflammatory and pain medications may help relieve your arthritis symptoms. Some medications, called biologics, target your immune systems inflammatory response. A healthcare provider may recommend biologics for your rheumatoid or psoriatic arthritis.
- Physical therapy: Rehabilitation can help improve strength, range of motion and overall mobility. Therapists can teach you how to adjust your daily activities to lessen arthritic pain.
- Therapeutic injections: Cortisone shots may help temporarily relieve pain and inflammation in your joints. Arthritis in certain joints, such as your knee, may improve with a treatment called viscosupplementation. It injects lubricant to help joints move smoothly.
What Are The Risk Factors For Arthritis
Some factors make you more likely to develop arthritis, including:
- Age: The risk of arthritis increases as you get older.
- Lifestyle: Smoking or a lack of exercise can increase your risk of arthritis.
- Sex: Most types of arthritis are more common in women.
- Weight: Obesity puts extra strain on your joints, which can lead to arthritis.
Recommended Reading: How To Heal Arthritis In Feet
Can Rheumatoid Arthritis Affect Your Jaw
Rheumatology Arthritis
Rheumatology arthritis is an autoimmune disease caused by an overactive immune system. This inflammatory condition affects your joints and causes severe pain and inflammation. Seeking medical help immediately is very important if you are diagnosed with rheumatology arthritis because this autoimmune condition can lead to joint damage and immobility.
One important thing you need to note is that rheumatoid arthritis can affect your jaw also. When it affects your jaw, you will experience stiffness, tenderness, and severe pain when you chew your food. In advanced cases of rheumatoid arthritis, the joint may make noises when moving and it will be very painful.
What Types Of Arthritis Affect The Jaw
The joint responsible for jaw pain is the temporal mandibular joint . This is where the lower jaw hinges at the level of the ear, Dr. Bykerk says. Responsible for talking as well as eating, the TMJ is the most frequently used joint in the body. This frequency of use also makes the jaw susceptible to different kinds of arthritis.
Like other joints, the TMJ is at risk for osteoarthritis, along with other types of arthritis such as rheumatoid arthritis, says Lauren Levi, DMD, dentist at The Mount Sinai Hospital in New York City. Osteoarthritis is the most common type of arthritis that affects the TMJ.
Some people may be more at risk for arthritis in the jaw than others. Macro or microtrauma, through grinding or clenching, along with decreased lubrication in the joint may increase the risk for developing arthritis, Dr. Levi says.
Stress and chronic pain in the body, such as may occur with arthritis elsewhere, can cause clenching so in a vicious cycle, jaw pain and arthritis may become a chicken or the egg scenario, Dr. Bykerk says.
People will clench if they have pain, if they are stressed, or pain can result if they clench too much or grind their teeth, called bruxism, she says. If bruxism and clenching go on too long the TMJ can wear out, the cartilage in the joint can break down and degenerative arthritis occurs.
Read Also: What Is Degenerative Arthritis In The Neck
Read Also: How Do You Know If You Have Rheumatoid Arthritis
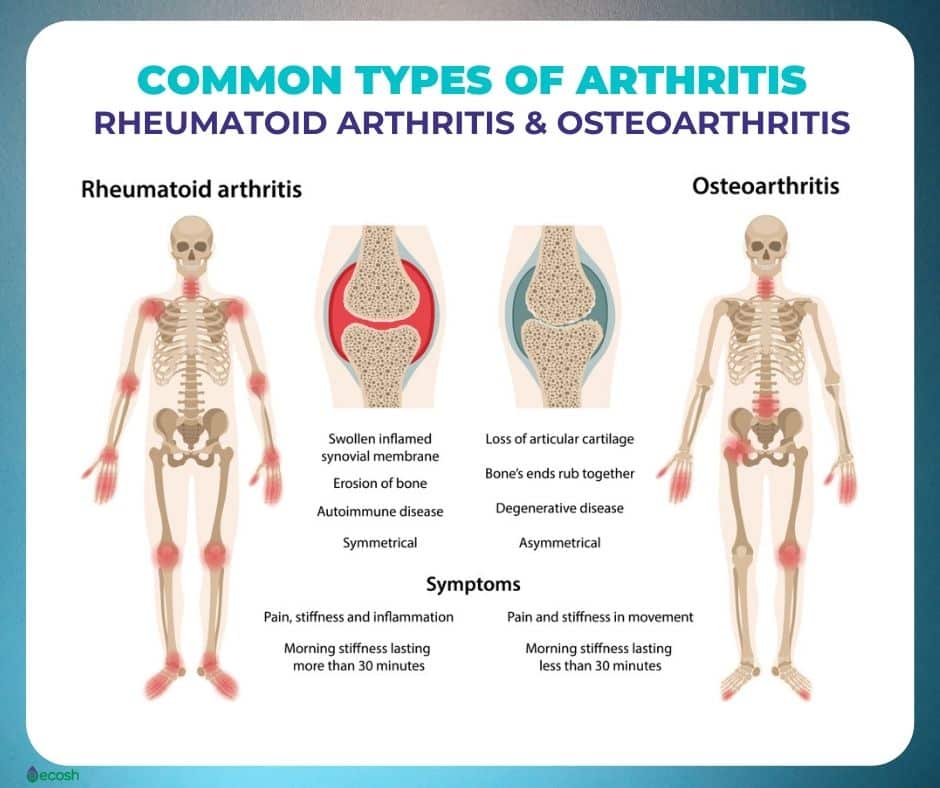
What Is Arthritis
Arthritis is a progressive condition marked by pain or stiffness in the jointsparts of the body where two or more bones meet . It can be caused by simple wear and tear or by an overactive immune system, depending on the type of arthritis. But in both cases, the condition can make it harder to carry out everyday activities and have a major impact on a persons quality of life.
Roughly 58.5 million US adults have been diagnosed with arthritis, and that number is expected to jump to 78 million by 2040, according to the Centers for Disease Control and Prevention. Its the leading cause of work disability, and may increase a persons risk for problems like excess body fat and depression.
With arthritis, even the simplest tasks can become monumental. Whether its knitting, hiking, cycling, or just playing with a beloved pet, the pain, stiffness and limitations that come with arthritis can render these activities difficult, says Elizabeth Ortiz, M.D., a Dallas-based rheumatologist in private practice and medical director of Motto Health.
The condition doesnt have to sideline you, though. With the right care plan, you can keep your arthritis symptoms in check and find ways to do more of the things you love with less pain.
Are You At Risk
Arthritis is a widespread disease, and risk factors depend on the type. Age increases the risk of arthritis types like osteoarthritis, while women are more predisposed to rheumatoid arthritis and lupus. Family history also plays a role in the amount of risk you may have. If you think you may have arthritis, make an appointment with your primary care physician.
Also Check: What Can You Do For Arthritis In The Back
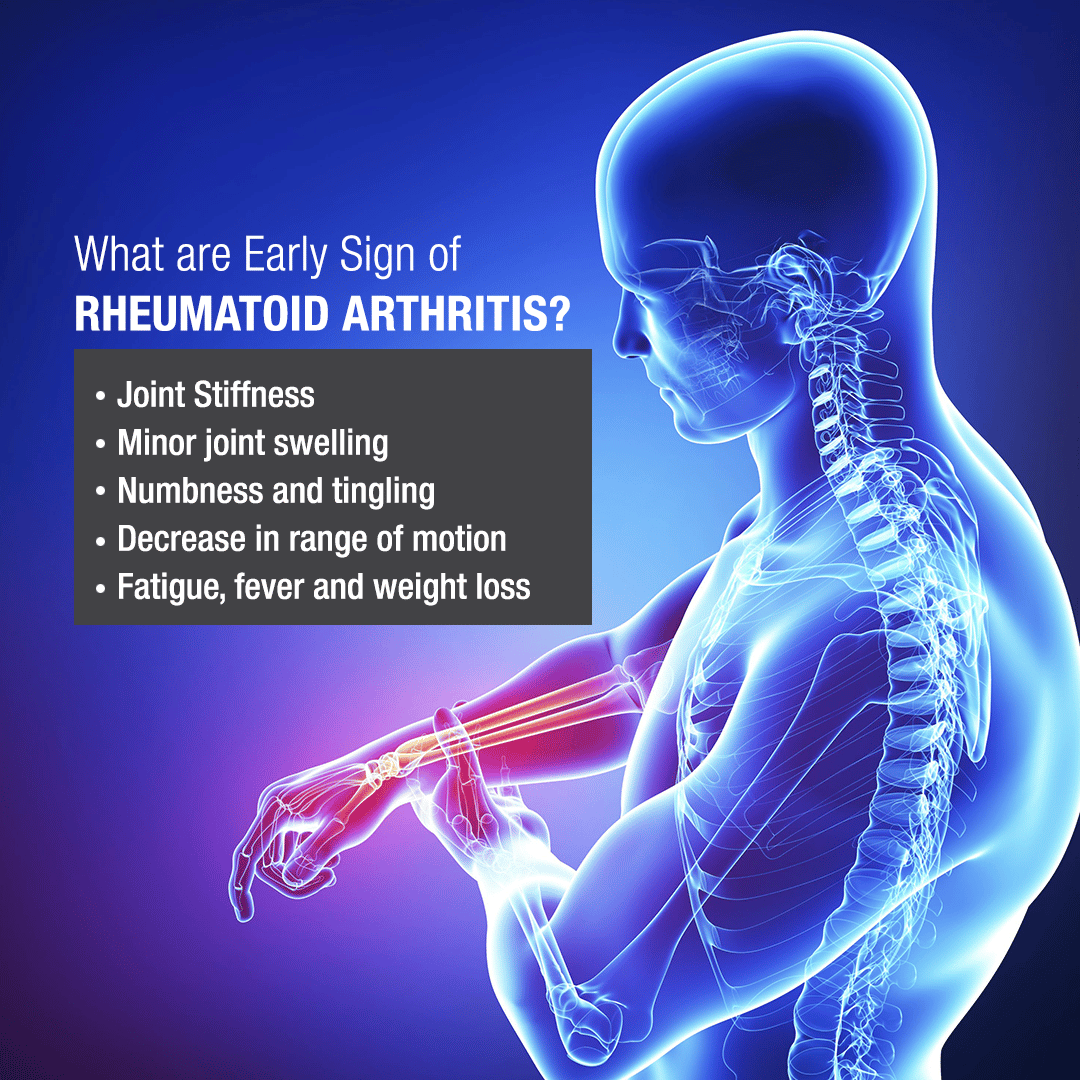
Signs And Symptoms Of Rheumatoid Arthritis
The main joint symptoms are related to the inflammation and include pain, swelling, redness, warmth and limitation in range of motion of the affected joints. These joints will be tender to pressure and can occasionally appear red. Inside the joints, the immune system has been activated, and many cells proliferate in the joints releasing multiple chemicals, such as cytokines, which cause fluid and additional inflammatory cells to enter the joint, and to cause pain. If the process remains active, the inflammatory process can cause damage in the joint .
Joint involvement in RA tends to affect multiple joints on both sides of the body, in what is called a symmetric pattern. That is, if your left knee is affected, your right knee will likely also be affected .
The joints most likely to be affected are the:
- small joints of the hands and feet
However, many other joints can be affected, such as the neck joints in the cervical spine, the shoulders, hips or temporo-mandibular joints .
Other Conditions And Joint Pain
Other forms of arthritis, and other conditions, can also cause joint pain. Examples include:
- fibromyalgia syndrome, a condition in which your brain processes pain in your muscles and joints in a way that amplifies your perception of the pain
- scleroderma, an autoimmune condition in which inflammation and hardening in your skin connective tissues can lead to organ damage and joint pain
Read Also: Does Arthritis Make Your Hands Shake
What If You Dont Respond To The Standard Disease Modifying Drugs
For some people, maybe 10% to 20% of people with RA, the disease is more aggressive and more difficult to get under swift control. But a range of injectablebiologic drugs have revolutionised treatment for people who dont respond to the standard DMARDs. Biologic drugs are a more complex form of DMARD. More recently, another class of drugs called JAK inhibitors have become available which are taken orally in the form of tablets which are as similarly highly effective as biologic drugs.
The NHS follows guidance set out by the National Institute for Health and Care Excellence about when biologics or JAK inhibitors can be prescribed. They are used after standard DMARDs havent worked sufficiently well, so theyre not usually prescribed for people who are newly diagnosed. They are also used if someone does not respond sufficiently well to the first biologic or JAK inhibitor given after standard DMARDs. In many cases, biologic drugs and JAK inhibitors are used with concomitant methotrexate therapy as an anchor drug, as mentioned earlier, as this boosts the overall benefits.
Also Check: How Should I Sleep With Neck Arthritis
Causes Of Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disease. This means your immune system attacks the cells that line your joints by mistake, making the joints swollen, stiff and painful.
Over time, this can damage the joints, cartilage and nearby bone.
It’s not clear what triggers this problem with the immune system, although you’re at an increased risk if:
- you are a woman
- you have a family history of rheumatoid arthritis
Find out more about the causes of rheumatoid arthritis.
Recommended Reading: What Are The Long Term Effects Of Rheumatoid Arthritis
How Doctors Diagnose Arthritis Jaw Pain
The underlying causes for jaw pain can be hard for doctors to suss out, as the TMJ is a very complex joint with multiple factors affecting it. Your rheumatologist or dentist may recommend a specialist who deals with TMJ disorders, called an oral and maxillofacial surgeon. A thorough comprehensive evaluation and history taking is crucial to accurately diagnosing the etiology of jaw pain, Dr. Levi says.
Osteoarthritis is often diagnosed based on symptoms and imaging, and is commonly is associated with joint sounds, known as crepitus, Dr. Levi says. Osteoarthritis is also often associated with morning stiffness, jaw tightness, and decreased range of motion of the jaw.
Jaw bone and cartilage changes due to arthritis may be seen on imaging tests such as an X-ray, CT scan, or MRI. Changes that can be visualized on imaging include condylar beaking or flattening , and decreased joint space, Dr. Levi says.
Other forms of arthritis, such as rheumatoid arthritis, may be diagnosed with help from blood tests, Dr. Levi says. With inflammatory or autoimmune diseases, you will have elevated inflammatory markers like c-reactive protein or erythrocyte sedimentation rate many rheumatoid arthritis patients also test positive for antibodies such as rheumatoid factor and anti-CCP.
But if you have inflammatory arthritis, chances are jaw pain wont be your first symptom and if youve already been diagnosed, your doctor will have an indication that jaw pain may be due to your condition.
Cannabis: A Modern View On An Old Medicine
A diagnosis of arthritis has been made by a medical professional in about half of all persons aged 65 and up, according to the Centers for Disease Control and Prevention. More than half of US adults with the illness, however, are of working age . Nationwide, medical marijuana consumers tend to be middle-aged, with a median age of 45. These results show that elderly people with more severe arthritis are less inclined to try medical cannabis as a treatment option.
There is still a lot of social stigma attached to cannabis, which is unfortunate. However, older generations still feel the effects of the misinformation spread during Nixons war on drugs and the Reefer Madness era, even while newer generations view the plant through different eyes. However, scientific and policy developments are also influencing the perspectives of the elderly. Only 0.4% of persons aged 65 and up were cannabis users in 2007. The 2015 increase was a whopping 2.9%.
Cannabinoids, terpenes, and flavonoids are just some of the components in cannabis that are currently being studied to see if they might alleviate pain, inflammation, joint degradation, and other symptoms that negatively impact the quality of life of the elderly.
Responsible cannabis use guidelines are also being developed in an effort to remove the irresponsible, lazy stoner stigma associated with the drug.
- Dont smoke and drive
- Be mindful of others
Recommended Reading: Is Coconut Oil Good For Arthritis
There Are Different Types Of Arthritis
It is important not to mistake arthritis with osteoporosis. They are as follows:
- Arthritis: A general term for conditions that affect the joints and surrounding tissues. Joints are places in the body where bones come together, such as the knees, wrists, fingers, toes, and hips. The two most common types of arthritis are osteoarthritis and rheumatoid arthritis.
- Osteoporosis: A condition in which the bones become less dense and more likely to fracture. In osteoporosis, there is a loss of bone tissue that leaves bones less dense and more likely to fracture. It can result in a loss of height, severe back pain, and change in posture. Osteoporosis can impair a persons ability to walk and can cause prolonged or permanent disability
Recommended Reading: How To Cure Arthritis In Lower Back