What’s The Difference Between Ra And Oa
There are common misconceptions when it comes to understanding what’s the difference between osteoarthritis and rheumatoid arthritis. The major differences are that osteoarthritis is associated with age and presents degenerative changes, while rheumatoid arthritis is an autoimmune disease and commonly affects younger people specifically women under the age of 40.
Because one is linked to aging and the other to an autoimmune disease, the treatment between the two will differ. For rheumatoid arthritis, the medication prescribed will focus on suppressing the immune system, but in osteoarthritis, treatment mainly concentrates on managing the pain.
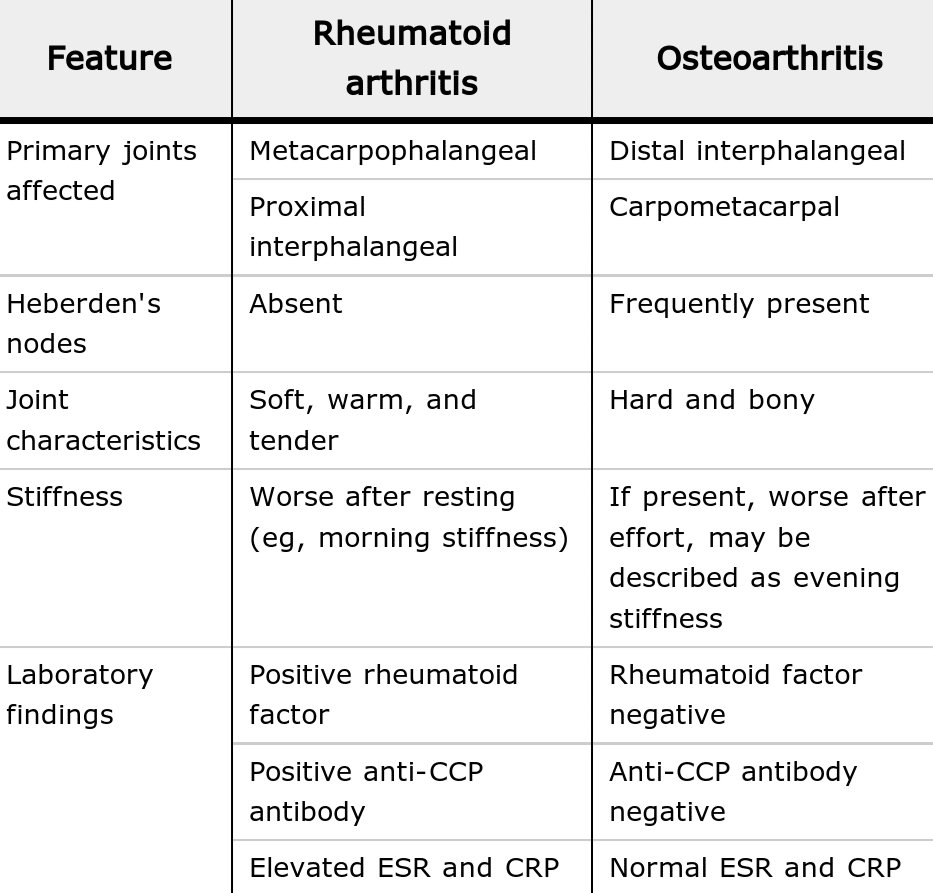
There are also differences in the pattern of symptoms and affected joints. In rheumatoid arthritis, the small and large joints are affected on both sides of the body, for example both hands or both wrists. In osteoarthritis, the symptoms typically start on one side of the body and may or may not spread. The symptoms are gradual and commonly restricted to one specific set of joints, for example the finger joints or, the weight-bearing joints such as the knees or hips.
Degenerative Joint Disease Vs Arthritis
When youre dealing with pain in your spine or any other joint in your body, medical terminology doesnt mean a whole lot to you. As far as youre concerned, pain is pain no matter what its called.
So when your doctor mentions degenerative joint disease as the cause of your discomfort, you might find yourself asking, how is that different from arthritis?
It isnt. Degenerative joint disease is just another name for osteoarthritis, which is the most common type of arthritis and it occurs when the components of a joint wear down. So whether we call it degenerative joint disease, osteoarthritis, or arthritis, were really talking about the same condition.
What Are The Risk Factors For Oa
- Joint injury or overuseInjury or overuse, such as knee bending and repetitive stress on a joint, can damage a joint and increase the risk of OA in that joint.
- AgeThe risk of developing OA increases with age.
- GenderWomen are more likely to develop OA than men, especially after age 50.
- ObesityExtra weight puts more stress on joints, particularly weight-bearing joints like the hips and knees. This stress increases the risk of OA in that joint. Obesity may also have metabolic effects that increase the risk of OA.
- GeneticsPeople who have family members with OA are more likely to develop OA. People who have hand OA are more likely to develop knee OA.
- Race Some Asian populations have lower risk for OA.
Read Also: What Are The Best Gloves For Arthritis
Affected Joints In Ra
RA usually begins in the smaller joints. Youre likely to have pain, stiffness, and swelling in the finger joints. As RA progresses, symptoms can develop in larger joints such as knees, shoulders, and ankles.
RA is a symmetrical disease. That means youll experience symptoms on both sides of your body at the same time.
Difference Between Osteoarthritis And Rheumatoid Arthritis
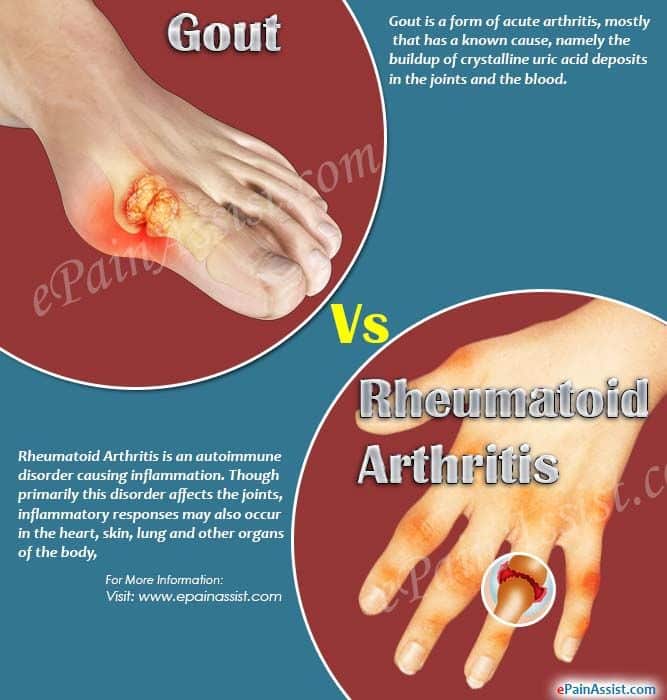
There are several different types of arthritis. Osteoarthritis and rheumatoid arthritis are two of the most common forms. Although the symptoms of these two types of arthritis can be similar, it’s very important to distinguish between them in order to determine the proper treatment.
At the University of Michigan Health System, our experienced rheumatologists will do appropriate tests to determine which type of arthritis you have. Then we will develop an effective treatment plan and will explain your options.
Osteoarthritis occurs when the smooth cartilage joint surface wears out. Osteoarthritis usually begins in an isolated joint.
Rheumatoid arthritis is an autoimmune disease, which means that the immune system malfunctions and attacks the body instead of intruders. In this case, it attacks the synovial membrane that encases and protects the joints. Rheumatoid arthritis often targets several joints at one time. The symptoms of rheumatoid arthritis include:
- the symmetrical nature of the disease ,
You May Like: Is It Osteoarthritis Or Rheumatoid Arthritis
What Are The Differences Between Osteoarthritis And Rheumatoid Arthritis
The main difference between these two types of arthritis is the cause of the joint pain and symptoms. Osteoarthritis is mainly due to the mechanical wear-and-tear placed on the joints, and it happens over the course of ones life. Rheumatoid arthritis, on the other hand, is an autoimmune disease that attacks the joints.
Osteoarthritis
Osteoarthritis is the most common type of arthritis. It is a degenerative disease and is mainly caused by aging. However, obesity can also cause it and make it worse. Carrying extra weight puts more stress and strain on your joints, and the extra fat tissue produces proteins that can trigger a harmful inflammatory response in your joints.
With the development of OA, the cartilage at the ends of your bones deteriorates from wear and tear. Cartilage is a protective cushion that helps bones in joints move and glide smoothly. With the loss of this protective tissue, bone begins to grind against bone.This leads to pain, stiffness, tenderness, loss of range of motion, and a grating sensation in the joint. Common joints affected include knees, kip, and hands.
Your arthritis doctor can diagnosis the condition through X-rays and MRI imaging. Blood tests may also be performed to help provide a more complete diagnosis. Unfortunately, the damage from OA cant be reversed. However, pain can be effectively managed through treatments such as exercise, physical therapy, surgery, cortisone injections, medication, and lifestyle changes.
Rheumatoid Arthritis
What Are The Goals Of Treating Rheumatoid Arthritis
The most important goal of treating rheumatoid arthritis is to reduce joint pain and swelling. Doing so should help maintain or improve joint function. The long-term goal of treatment is to slow or stop joint damage. Controlling joint inflammation reduces your pain and improves your quality of life.
Recommended Reading: What Is The Medication For Arthritis
What Are The Four Stages Of Osteoarthritis
The four stages of osteoarthritis are 1) minor, 2) mild, 3) moderate and 4) severe.
Stage 1 Minor OA means your joint is showing signs of minor bone spur growth. These bony growths develop near the joint meaning there might be some cartilage loss but, in general, you won’t experience much, if any, pain at this stage of OA.
Stage 2 Mild OA reveals greater bone spur growth but the cartilage is still intact, usually within a healthy range and the bones won’t be rubbing together. You’ll also still usually have normal levels of synovial fluid between your joints at this stage. However, at this point, you’ll likely begin to experience some uncomfortable symptoms such as pain after a long period of walking or running, stiffness after the joint hasn’t been used in a while and tenderness when bending the joint.
Stage 3 Moderate OA means that your cartilage between the joint has undergone more obvious damage with less space between your bones. You’ll likely be experiencing joint pain more regularly especially when walking or bending. You might also start to experience stiffness after long periods of sitting still, some swelling of the joint or more achiness in the morning.
What Is The Safest Drug For Rheumatoid Arthritis
The safest drug for rheumatoid arthritis is one that gives you the most benefit with the least amount of negative side effects. This varies depending on your health history and the severity of your RA symptoms. Your healthcare provider will work with you to develop a treatment program. The drugs your healthcare provider prescribes will match the seriousness of your condition.
Its important to meet with your healthcare provider regularly. Theyll watch for any side effects and change your treatment, if necessary. Your healthcare provider may order tests to determine how effective your treatment is and if you have any side effects.
Read Also: What Makes Arthritis Pain Worse
How Is Rheumatoid Arthritis Diagnosed
Your healthcare provider may refer you to a physician who specializes in arthritis . Rheumatologists diagnose people with rheumatoid arthritis based on a combination of several factors. Theyll do a physical exam and ask you about your medical history and symptoms. Your rheumatologist will order blood tests and imaging tests.
The blood tests look for inflammation and blood proteins that are signs of rheumatoid arthritis. These may include:
- Erythrocyte sedimentation rate or sed rate confirms inflammation in your joints.
- C-reactive protein .
- About 80% of people with RA test positive for rheumatoid factor .
- About 60% to 70% of people living with rheumatoid arthritis have antibodies to cyclic citrullinated peptides .
Your rheumatologist may order imaging tests to look for signs that your joints are wearing away. Rheumatoid arthritis can cause the ends of the bones within your joints to wear down. The imaging tests may include:
In some cases, your provider may watch how you do over time before making a definitive diagnosis of rheumatoid arthritis.
Difference In Treatments For Ra Vs Arthritis
Because the cause of RA is different than other types of arthritis, like osteoarthritis, it makes sense that will differ as well. One big difference? There are a lot more treatment options for RA. When I see a patient for the first time, and I am trying to diagnose what is the cause of their joint pain, I am happier to diagnose them with rheumatoid arthritis than I am with osteoarthritis because we have such good medical therapies for rheumatoid arthritis, says Dr. Blank. For osteoarthritis, she adds, we don’t have anything that can halt the progression of the diseaseall we can do is treat the pain.
Treatments for RA include disease-modifying-anti-rheumatic-drugs , which work by suppressing the immune system and therefore reducing inflammation in your joints, slowing the progression of the disease. The recommendation is to start something like methotrexate for moderate to high disease severity, says Dr. Sharmeen. If over time, thats not enough, well add on another treatment such as biologic drug.
Biologics are drugs that target specific immune proteins that cause inflammation. There are several different options here, including:
-
tumor necrosis factor inhibitors which targets tumor necrosis factor, a substance people with RA make in excess
-
B-cell inhibitors which home in on inflammation-causing lymphocytes
-
T-cell inhibitors which target immune T-cells
-
Interleukin inhibitors which stop specific proteins from attaching to cells and causing inflammation
Don’t Miss: What Blood Tests Indicate Rheumatoid Arthritis
Osteoarthritis Vs Rheumatoid Arthritis Diagnosis
Rheumatoid arthritis is diagnosed by performing several tests. There is no single test that identifies rheumatoid arthritis:
- Physical examination to look for swelling, redness and other outward physical symptoms.
- Blood tests look for the rheumatoid factor, anti-CCP and antinuclear antibodies, and the level of inflammation.
- Imaging tests that include x-rays, MRIs and/or ultrasounds.
Considering what can be determined by an osteoarthritis vs rheumatoid arthritis xray, the x-ray is more beneficial for detecting osteoarthritis because the disease involves the bones in its early stages. Rheumatoid arthritis may not present itself in the bones in its early stages. Instead, the patient may experience non-bone issues first, like chronic fatigue, or synovial and tendon inflammation. For this reason, the MRI and ultrasound are better than x-rays for early diagnose of rheumatoid arthritis.
Can Rheumatoid Arthritis Go Away
No, rheumatoid arthritis doesnt go away. Its a condition youll have for the rest of your life. But you may have periods where you dont notice symptoms. These times of feeling better may come and go.
That said, the damage RA causes in your joints is here to stay. If you dont see a provider for RA treatment, the disease can cause permanent damage to your cartilage and, eventually, your joints. RA can also harm organs like your lung and heart.
A note from Cleveland Clinic
If you have rheumatoid arthritis, you may feel like youre on a lifelong roller coaster of pain and fatigue. Its important to share these feelings and your symptoms with your healthcare provider. Along with X-rays and blood tests, what you say about your quality of life will help inform your treatment. Your healthcare provider will assess your symptoms and recommend the right treatment plan for your needs. Most people can manage rheumatoid arthritis and still do the activities they care about.
Last reviewed by a Cleveland Clinic medical professional on 02/18/2022.
References
Also Check: Is Rheumatoid Arthritis An Inflammatory Disease
Whats The Most Painful Arthritis
Rheumatoid arthritis can be one of the most painful types of arthritis it affects joints as well as other surrounding tissues, including organs. This inflammatory, autoimmune disease attacks healthy cells by mistake, causing painful swelling in the joints, like hands, wrists and knees.
Finding An Arthritis Doctor
If you suffer from chronic joint pain and stiffness, it may be time to visit the doctor. If you need a referral, ask your primary care doctor for help. A doctor that specializes in arthritis and joint pain can help you effectively manage your pain and symptoms. If you are looking for a Las Vegas arthritis doctor, contact Apex Medical Center to see how we can help you. We specialize in the management and treatment of painful conditions.
Image courtesy of yodiyim at FreeDigitalPhotos.net
You May Like: How To Treat Arthritis At Home
How Do You Diagnose Arthrosis
How are arthrosis and other types of arthritis diagnosed?
Which Arthritis Is Worse
A common question people ask goes like this: Is osteoarthritis worse than rheumatoid arthritis? Rheumatoid arthritis is a more complex and widespread disease. It presents itself differently in each patient and is more difficult to diagnose because of its complexity. It can lead to other diseases, like cardiopulmonary disease and makes people more susceptible to diseases like lupus.
Osteoarthritis is localized in the joint, and some joints can be replaced if the damage from arthritis is severe. It does not impact organs or lead to other diseases.
However, both diseases are chronic and neither is curable. They both affect the quality of life. It is important to address the symptoms as soon as they appear. In both types of arthritis, the sooner treatment begins, the better.
Don’t Miss: How To Relieve Arthritis Pain In Knuckles
Want To Get More Involved With Patient Advocacy
The 50-State Network is the grassroots advocacy arm of CreakyJoints and the Global Healthy Living Foundation, comprised of patients with chronic illness who are trained as health care activists to proactively connect with local, state, and federal health policy stakeholders to share their perspectives and influence change. If you want to effect change and make health care more affordable and accessible to patients with chronic illness, learn more here.
Joint Pain: Where It Hurts Most
RA It can affect the entire body or just specific joints, most commonly the hands, wrists, fingers, elbows, knees, feet, and hips. Sometimes what is noticed first is the stiffness in the morning. The synovium, or the lining of the joint, is most affected.
OA It affects only a particular joint, and the pain doesn’t go away without physical or medical therapy. The joint cartilage is what is worn away.
As OA progresses it can result in bony growths or spurs that can further compromise joints . Sometimes you can have joints that make noise that can be painful . It is also possible to get some radiating pain .
Read Also: Does Acupuncture Help Rheumatoid Arthritis
Early Treatment Can Help Immensely
Degenerative arthritis is the most common type of arthritis, affecting around 30 million Americans. Also referred to as osteoarthritis, degenerative joint disease, and wear-and-tear arthritis, it occurs when joint cartilage and underlying bone begin to deteriorate, causing progressive pain, stiffness, and joint malformation.
While it can affect any joint, osteoarthritis typically develops in the hands, feet, shoulder, and neck and in the weight-bearing joints, so you may have degenerative arthritis of the spine, hips, or knees.
Diagnosis is typically made based on the signs and symptoms of the disease and supported by imaging tests. Treatment can vary based on the severity of symptoms, with more modest options like heat or ice application helping mild cases and more significant interventions, like injections and surgery, being used for severe cases.
The Location Of The Joint Pain
RA Most commonly these joints are affected: hands, wrists, fingers, elbows, knees, feet, and hips. However, the pain can be in any joint. The pain is usually symmetrical it effects both sides of the body at the same time.
OA There is pain wherever a joint has been injured or worn through overuse most commonly in the hands, fingers, thumb, knees, hips, lower back and neck. The pain is not symmetrical. The lifetime risk of developing OA of the knee is about 46 percent, and the lifetime risk of developing OA of the hip is 25 percent, according to the American College of Rheumatology.
Read Also: What Natural Remedies For Arthritis
Symptoms Of Degenerative Arthritis
The central symptoms of degenerative arthritis are pain and stiffness. The pain typically increases with activity and is relieved by rest.
Joint stiffness is common in the morning hours but tends to improve as you move about, usually within 30 minutes. Inactivity during the day, such as sitting for long periods, can also lead to stiffness and may even cause the locking of joints in some people.
Another common symptom of osteoarthritis is crepitus, in which a joint will make popping and crackling noises with movement. Crepitus most commonly affects the shoulder or knee joint but can also occur in the wrist, fingers, elbow, and ankle.
As the disease progresses, it can affect a person’s posture and gait, leading to instability and a decreased range of motion. As mobility is increasingly impaired, muscle loss may develop .
In advanced stages, degenerative arthritis can cause the visible malformation of a joint, particularly in the fingers where hard, bony enlargements can develop on and around the joint. The abnormal accumulation of fluid, known as an effusion, is also a common occurrence in people with advanced knee arthritis.
In some people, osteoarthritis can become so severe that the pain becomes relentless, making walking or even standing near impossible. While certain treatments can help ease symptoms, any damage sustained by a joint cannot be reversed without surgery.