Skin Psoriasis Treatment Options And Medications
Every case of psoriasis is unique, and ultimately every treatment plan will be unique as well. While there is no known cure, the goal of psoriasis treatment is to reduce inflammation and control shedding of the skin to make flare-ups more manageable. It is important to contact your dermatologist right away if you develop joint pain, as psoriatic arthritis can cause severe joint damage if left untreated.
Dermatology Associates of Plymouth Meeting offers a variety of treatment options to manage psoriasis and treat psoriatic arthritis symptoms:
Causes Of Psoriatic Arthritis
Almost 1 in 3 people with psoriasis also have psoriatic arthritis.
It tends to develop 5 to 10 years after psoriasis is diagnosed, although some people may have problems with their joints before they notice any skin-related symptoms.
Like psoriasis, psoriatic arthritis is thought to happen as a result of the immune system mistakenly attacking healthy tissue.
But it’s not clear why some people with psoriasis develop psoriatic arthritis and others do not.
When To Get Medical Advice
See a GP if you have persistent pain, swelling or stiffness in your joints even if you have not been diagnosed with psoriasis.
If you’ve been diagnosed with psoriasis, you should have check-ups at least once a year to monitor your condition. Make sure you let the doctor know if you’re experiencing any problems with your joints.
Recommended Reading: Why Is Rheumatoid Arthritis So Painful
Treatments For Your Skin
If your psoriasis is affecting your quality of life, or your treatment is not working, you may be referred to a dermatologist.
There are a number of treatment options for psoriasis.
Ointments, creams, and gels that can be applied to the skin include:
- ointments made from a medicine called dithranol
- steroid-based creams and lotions
- vitamin D-like ointments such ascalcipotriol and tacalcitol
- vitamin A-like gels such astazarotene
- tar-based ointments.
For more information about the benefits and disadvantages of any of these talk to your GP, dermatologist, or pharmacist.
If the creams and ointments dont help, your doctor may suggest light therapy, also known as phototherapy. This involves being exposed to short spells of strong ultraviolet light in hospital.
Once this treatment has started, youll need to have it regularly and stick to the appointments youve been given, for it to be successful. This treatment is not suitable for people at high risk of skin cancer or for children. For some people, this treatment can make their psoriasis worse.
Retinoid tablets, such as acitretin, are made from substances related to vitamin A. These can be useful if your psoriasis isnt responding to other treatments. However, they can cause dry skin and you may not be able to take them if you have diabetes.
Some DMARDs used for psoriatic arthritis will also help with psoriasis.
You May Like: Does Psoriatic Arthritis Cause Bruising
Pain In Your Knees Ankles Wrists Or Elbows
While shooting pain in the big toe is very characteristic of gout, it can affect any joint and present like psoriatic arthritis, says Dr. Malik. Uric acid crystals can form in your foot, ankle, knee, elbow, hand, wrist, and small joints in your fingers. Roughly 25 percent of gout patients experience polyarticular symptoms. This means the pain strikes in more than one joint at a time for example, the big toe and the left knee. While gout rarely impacts the spine, it can affect soft tissues in the body, including your bursae and sheaths around your tendons.
Don’t Miss: What’s The Best Treatment For Arthritis In The Knee
What Is Psoriatic Arthritis
Psoriatic arthritis is a type of inflammatory arthritis. It occurs when your bodys immune system works overtime, creating inflammation throughout your body. In psoriatic arthritis, that inflammation targets the joints and the places where tendons and ligaments attach to bones.
Most people with psoriatic arthritis also have psoriasis, a disease that causes red, scaly patches of skin. Psoriatic arthritis can strike at any age, though symptoms usually develop between ages 30 and 50.
Medical Writing And Editorial Assistance
The authors thank Linda Grinnell-Merrick, NP, of Novartis Pharmaceuticals Corporation, East Hanover, NJ for providing medical expertise and content development, and Charli Dominguez, PhD, of Health Interactions, Inc, Chicago, IL, for providing medical writing support/editorial support funding was provided by Novartis Pharmaceuticals Corporation, East Hanover, NJ, in accordance with Good Publication Practice guidelines . Authors had full control of the content and made the final decision on all aspects of this publication.
Don’t Miss: What Are Biologics For Rheumatoid Arthritis
What’s The Difference Between Psoriatic Arthritis And Rheumatoid Arthritis
RA and PsA are both inflammatory conditions that affect people in the same age group and are often symmetrical, which means symptoms affect the joints on both sides of the body, rheumatologist Vinicius Domingues, MD, medical advisor to CreakyJoints, tells Health. Both conditions are also the result of an overactive immune systemone where your body attacks the joints and causes pain, stiffness, and swelling.
Many symptoms are the same between the two diseasesand treatments often overlap as wellbut the main difference is where those symptoms are located. People with PsA, for example, often have symptoms in the distal joints of their fingers and toes, whereas people with RA suffer in their middle joints. PsA also affects more than just your joints, often attacking your eyes, skin, nails, and tendons.
Treatment For Psoriatic Arthritis
Treatment for psoriatic arthritis aims to:
- relieve symptoms
- slow the condition’s progression
- improve quality of life
This usually involves trying a number of different medicines, some of which can also treat the psoriasis. If possible, you should take 1 medicine to treat both your psoriasis and psoriatic arthritis.
The main medicines used to treat psoriatic arthritis are:
- non-steroidal anti-inflammatory drugs
- biological therapies
Recommended Reading: How To Stop Arthritis Inflammation
Common Symptoms Of Gout
Gout is characterized by intermittent episodes of sudden onset of red, hot, and swollen joints one or more with symptom-free intervals, says Shailendra Singh, MD, FACP, Rheumatology Medical Director at White River Medical Center in Batesville, Arkansas. A gout attack can last anywhere from a few days to 10 days or longer. Gout attacks often strike in the middle of the night, so you feel sudden pain when you wake up in the morning . You can go to bed feeling fine and wake up with severe symptoms.
Swollen Fingers And Toes
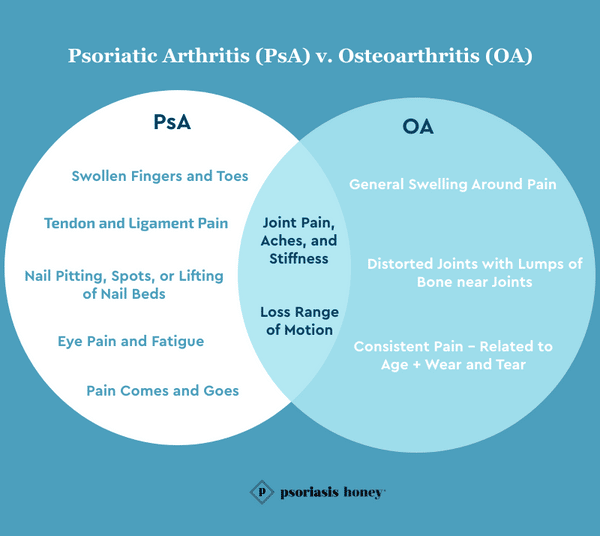
PsA is an inflammatory condition that causes swelling of the fingers and toes, which may come to resemble sausages. Inflammation is not typically a significant symptom of OA, although it may occur around the affected joints. In this case, the inflammation usually affects a single finger or toe during a flare.
You May Like: What Young Living Oil Is Good For Arthritis
Psoriatic Arthritis Versus Osteoarthritis
Joint pain and stiffness, especially in the morning or after resting, can be a symptom of either psoriatic arthritis or osteoarthritis the most common type of arthritis.
Unlike autoimmune forms of arthritis, osteoarthritis is the result of wear-and-tear damage to cartilage the slippery covering that allows bones to easily slide over each other when joints bend, says the Arthritis Foundation.
Damage to the cartilage can result in bone grinding directly on bone, which causes pain and restricts movement.
Osteoarthritis primarily affects the hands, knees, hips, and spine, and can create a grating sensation, along with popping or crackling, when you use the joint, says the Mayo Clinic. You may also notice hard lumps of bone near the joint or the joint may look distorted.
While psoriatic arthritis symptoms tend to flare and subside, osteoarthritis-related pain and swelling usually become progressively worse over time.
Epidemiological Characteristics Of Ra And Psa
RA is more common than PsA, affecting more than 1 million in the USA. PsA affects roughly half a million people in the USA and approximately 30% of patients with psoriasis. Worldwide prevalence estimates for RA and PsA are variable. In many populations, RA prevalence is estimated to be 0.5%1.0% however, prevalence is much higher in Native American Indian populations but lower in China and Japan . PsA prevalence estimates in the USA and Europe range from 0.1% to 0.4%, whereas in Japan, PsA prevalence is lower. This variability in prevalence suggests that both environmental and genetic factors affect risk for disease.
Read Also: What Meds Are Best For Arthritis
What Are The Symptoms Of Psa
Beyond the classic symptoms of arthritis, including painful and swollen joints, PsA presents itself with a number of symptoms. If you are living with PsA, you may have one or several of these symptoms during flare-ups. Additionally, the presence of psoriasis is also a classic symptom of PsA. Though, in a small percentage of individuals who live with PsA, no symptoms of psoriasis appear at all. In the overwhelming majority of cases, even if no psoriasis is present, there is a family history of it.
Some of the more common symptoms of PsA include:
- Joint pain and inflammation
Common Symptoms Of Psoriatic Arthritis
The symptoms of PsA can differ from person to person and depend on the type of psoriasis you have. For some, PsA may just involve the skin while others may have joint or even spine involvement. In 10 to 15 percent of cases, people get joint pain before having psoriasis skin plaques.
Classic psoriatic arthritis symptoms include:
Don’t Miss: How To Exercise With Arthritis
Introduction To Psoriatic Arthritis Rheumatoid Arthritis And Osteoarthritis
Psoriatic arthritis is a chronic inflammatory heterogeneous arthritis that is associated with psoriasis, and approximately 30% of patients with psoriasis develop PsA . It is estimated that PsA has a prevalence rate of approximately 12 per 1000 in the general population and an incidence rate of approximately 6 per 100,000 per year . Generally, onset of PsA occurs between ages 30 and 50 years but can develop at any point throughout a patients lifetime. The Group for Research and Assessment of Psoriasis and Psoriatic Arthritis defined six clinical domains that can be involved with PsA: peripheral arthritis, enthesitis, dactylitis, psoriasis, psoriatic nail disease, and axial disease .
A proper diagnosis and timely treatment of PsA are essential to prevent permanent joint damage and decrease functional disability . Patients are often seen by various healthcare providers on their pathway to a diagnosis of PsA, including dermatologists, orthopedists, general practitioners, chiropractors, and advanced practice providers . Diagnosis of PsA relies on early detection through appropriate history taking, careful examination, and clinical judgment, and APPs are in a position to see many patients with different rheumatic diseases therefore, it is imperative that APPs are aware of and receive proper training to accurately screen for features to identify PsA.
Tips For Identifying Oa
OA isnt a disease that cycles, like PsA. Instead, it can gradually get worse.
OA pain may be mild at first. You might notice a slight twinge in your knee when you bend it, or your joints might ache after a workout.
The pain, swelling, and stiffness will get worse as the joint damage increases. Along with the pain, your joints will feel stiff especially when you first wake up in the morning.
OA will most likely affect the joints of your body that move the most.
This includes the joints in your:
You May Like: What Can You Do With Arthritis In The Knee
Stay Educated And Aware Of Symptoms
Overall, both conditions can present very similarly, and cause confusion for both individuals with the condition, and the healthcare providers trying to diagnose and treat them. The most important thing is to remain educated and aware of your symptoms, in order to best help your healthcare team get to the root of your struggles!
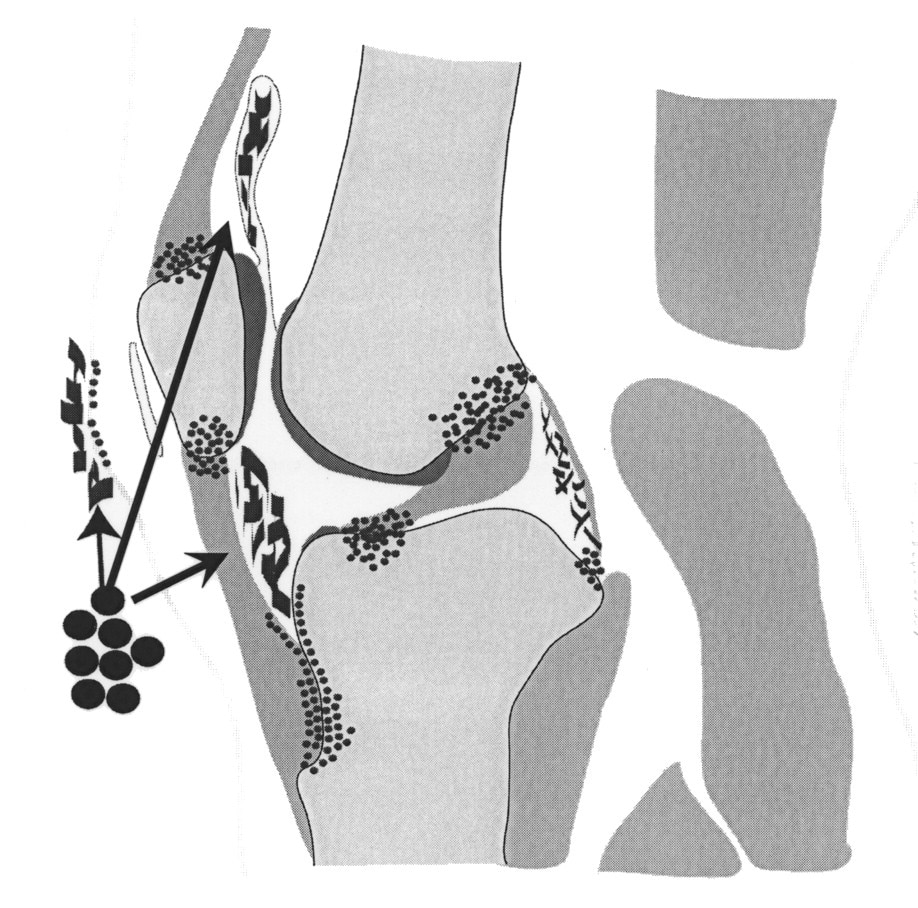
Underpinning Pathological Concepts For Common Ground Between Oa And Psa
It was proposed more than a decade ago that enthesitis may be the primary lesion in PsA and SpA . A number of imaging studies have since emerged showing that enthesopathy is common in psoriasis patients without clinical arthritis . Although it is difficult to prove the primacy of enthesitis in human PsA in all patients at all sites of disease, several animal models with features of PsA or SpA can clearly be shown to start at the enthesis . Likewise, several experimental studies have shown that spontaneous knee OA can start in the ligament and enthesis and not the articular cartilage, thus providing proof of principle of similar micro-anatomical topography for disease onset . Studies in the generalized form of human hand OA have also shown that the ligaments and enthesis are the sites of the earliest discernible pathology . The importance of the enthesis has also emerged in knee OA in man . Collectively this has resulted in a mechanistic anatomical classification of OA that recognizes that the generalized form of disease that was previously designated as idiopathic appears to have an enthesis-associated micro-anatomical basis .
The different entheses form what is now known as the synovialentheseal complex, where both degenerative and inflammatory processes can occur . If the pathological processes share the same micro-anatomical territory, then it is worth exploring anew the features that have been historically used to differentiate OA and PsA.
Also Check: How Do You Treat Gout Arthritis
Comorbidities Occurring In Ra And Psa
Differences in patient comorbidities may help clinicians differentiate between RA and PsA . Overall, comorbidity burden may be higher in RA than in PsA, but both diseases are similarly associated with increased risk for comorbidities linked to systemic inflammation . Han and colleagues found that patients with RA and PsA had similarly increased prevalence ratios of ischaemic heart disease, atherosclerosis, peripheral vascular disease, congestive heart failure, cerebrovascular disease, hyperlipidaemia and hypertension compared with healthy controls. However, registry data suggest that the rates of obesity, diabetes mellitus and metabolic syndrome are significantly higher in patients with PsA compared with those with RA. Notably, most patients with PsA are overweight or obese. Cardiometabolic comorbidities of PsA are associated with higher levels of systemic inflammation and increased disease severity. In addition, psoriatic skin lesions are associated with an increased risk for cardiovascular disease and mortality. Of interest, PsA is an independent predictor of non-alcoholic fatty liver disease in patients with psoriasis, while in patients with RA, the rates of NAFLD are similar to those observed in the general population.
Summary of differences in common comorbidities associated with PsA and RA
Pharmaceutical Treatments For Ra And Psa:
- Non-steroidal anti-inflammatory drugs such as ibuprofen and naproxen
- Corticosteroids like prednisone
- Disease-modifying anti-rheumatic agents like methotrexate and hydroxychloroquine
- Biologics, a more advanced type of DMARD that can stop or slow inflammation these include Tumor Necrosis Factor- inhibitors and interleukin inhibitors
You May Like: Is Flaxseed Good For Arthritis
Early Diagnosis And Appropriate Treatment
Now the good news: treatment has come a long way in recent years.
There are a number of good treatment paradigms for psoriatic arthritis, and the likelihood of severe deformity like there was in the past is close to zero with the new therapies we have, Hylland says.
There are also effective treatments for managing rheumatoid arthritis. And while its possible to have both psoriatic arthritis and rheumatoid arthritis at the same time, that wont necessarily complicate your treatment plan.
The initial treatments are the same for both, says Bauer, noting that tumor necrosis factor inhibitors work well for both types of arthritis, especially for people who cant take methotrexate, which is another first-line treatment.
Parade Daily
Another med that can be used to treat either RA or psoriatic arthritis is a Janus kinase inhibitor, or JAK inhibitor, like tofacitinib. This type of drug interrupt your immune systems urge to overproduce lots of inflammation-causing proteins called cytokines. They may work better for you than other kinds of drugs and they have the bonus of being available in pill form, rather than an injection or infusion.
With either condition, its crucial that you dont ignore the symptoms until they become very severe. Early diagnosis is critically important for slowing the progression of these diseases.
The earlier we catch it, the less we have to do to quiet itthe less medication we have to use it quite it, says Hylland.
Different Underlying Causes And Types Of Pain
While PsA presents with joint stiffness and swelling due to an overactive immune response, osteoarthritis usually has minimal swelling, and is the result of wear-and-tear to joints. This is why OA affects primarily major or weight-bearing joints, such as the hips, knees, spine, or neck, and typically shows up later in life. PsA can arise across a variety of ages, and often affects the smaller joints of the fingers and toes first . The wear-and-tear of OA is a result of cartilage breaking down. Cartilage normally keeps joints smooth and allows them to function without friction, and without it, can lead to clicking or brittle joints.
Additionally, pain and stiffness in PsA is also typically cyclic, with periods of flare-ups and remission, whereas, OA is a degenerative condition that is constantly getting worse, despite attempts at movement. Finally, the risk factors that lead to the development of each condition are also varied. Obesity, advanced age, previous joint injuries or deformities, repetitive motions, and genetics can all play a role in developing OA, whereas PsAs causes are typically genetics, previous trauma , medications, and stress.
You May Like: How Can I Help My Dogs Arthritis
Overlap Between Psoriatic Arthritis And Gout
Interestingly, people with psoriatic arthritis and/or psoriasis also have a higher risk of developing gout compared to those without these conditions. According to a study in the journal Annals of the Rheumatic Diseases, the risk of developing gout was nearly five times greater for men and women with psoriasis and psoriatic arthritis. Individual studies have varied with incident rates ranging from one to seven times higher in people with psoriasis and psoriatic arthritis, says Dr. Kohler.
While researchers have yet to determine the exact link, possible theories include the fact that high uric acid levels in gout are thought to be a product of the high skin cell turnover and inflammation that occurs in PsA. People with PsA have injured skin or bone that contributes to increasing inflammation, which in turn may active existing gout crystals that may be present, says Dr. Kohler.
We need to be mindful that just because a person has psoriasis, it doesnt mean the acute joint pain is psoriatic arthritis, says Dr. Malik. It could also be gout.