Talk With Others Who Understand
MyPsoriasisTeam is the social network for people with psoriasis and their loved ones. On MyPsoriasisTeam, more than 105,000 members come together to ask questions, give advice, and share their stories with others who understand life with psoriasis.
Are you dealing with both skin and joint symptoms? Share your experiences in the comments below, or start a conversation by posting on your Activities page.
How Is Psoriatic Arthritis Diagnosed
To diagnose psoriatic arthritis, your doctor will probably first perform a physical exam to look for swollen joints skin or nail changes eye problems and joint tenderness.
You may be asked to undergo an X-ray, MRI, ultrasound, or CT scan, so your physician can get a better look at your joints.
Editorâs Picks
When To Seek Medical Advice
You should speak to your GP if you experience constant pain, swelling or stiffness in your joints even if you haven’t been diagnosed with psoriasis.
If you have been diagnosed with psoriasis, you should have check-ups at least once a year to monitor your condition. Make sure you let your doctor know if you’re experiencing any problems with your joints.
Also Check: What Does Arthritis Pain Feel Like In The Knee
Reducing Signs And Symptoms
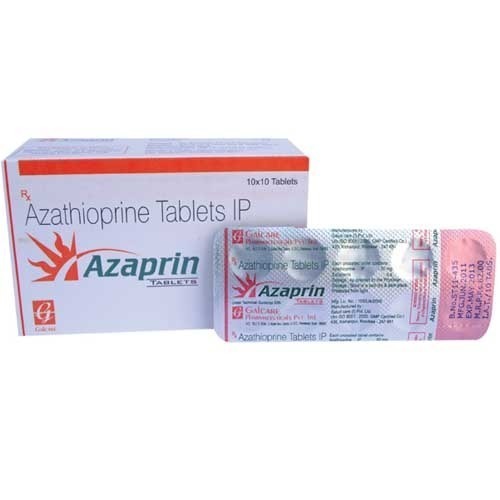
Both of these drugs reduce the signs and symptoms of psoriatic arthritis and most exciting they also can slow down damage to your joints, Dr. Smith says
DMARDs slow down psoriatic arthritis and improve quality of life for most people, Dr. Smith says. Some patients will even achieve a remission while taking them. But more typically, disease activity continues, but at a slower, less intense rate.
If your doctor prescribes DMARDs, here, according to Dr. Smith, are three things you should know about these powerful medicines.
1. All DMARDs may have side effects
Because DMARDs are a systemic treatment, they may have side effects, such as stomach upset, liver problems or blood issues, Dr. Smith says. It may take some tinkering for your physician to find the right regimen for you.
Possible long-term complications include liver damage with methotrexate and leflunomide. Some dormant long-term infections such as tuberculosis, can be re-activated by DMARDs.
DMARDs change your immune system, so you may get more intense viral or bacterial infections. Make sure to let your doctor know about any serious infections, Dr. Smith says.
You also should check with your doctor before getting any vaccines, Dr. Smith says. Live vaccines, like the shingles vaccine, may be dangerous with certain of medications, he says.
Some biologics also have been linked to a very small increased risk of cancer. You should ask your doctor about it, Dr. Smith says.
Buy Good Shoes With Arch Support
People who have psoriatic arthritis often experience pain in their toes, which can make it difficult to walk or exercise. Wearing supportive shoes with plenty of toe room and using orthotics, either off the shelf or custom-made, can relieve foot pain. Orthotics redistribute the pressure on your foot, Lawton says, and supportive or cushioned shoes can provide comfort and better skeletal alignment.
Your exercise shoes should be designated only as your exercise shoes. Wearing your shoes for other reasons than exercise wears them down much quicker and theyll need to be replaced sooner, says Lawton. She recommends replacing your shoes every nine to 18 months, depending on how frequently youre exercising.
If foot pain related to psoriatic arthritis is an issue for you, talk to your rheumatologist or a foot specialist .
Don’t Miss: Is Marijuana Good For Arthritis Pain
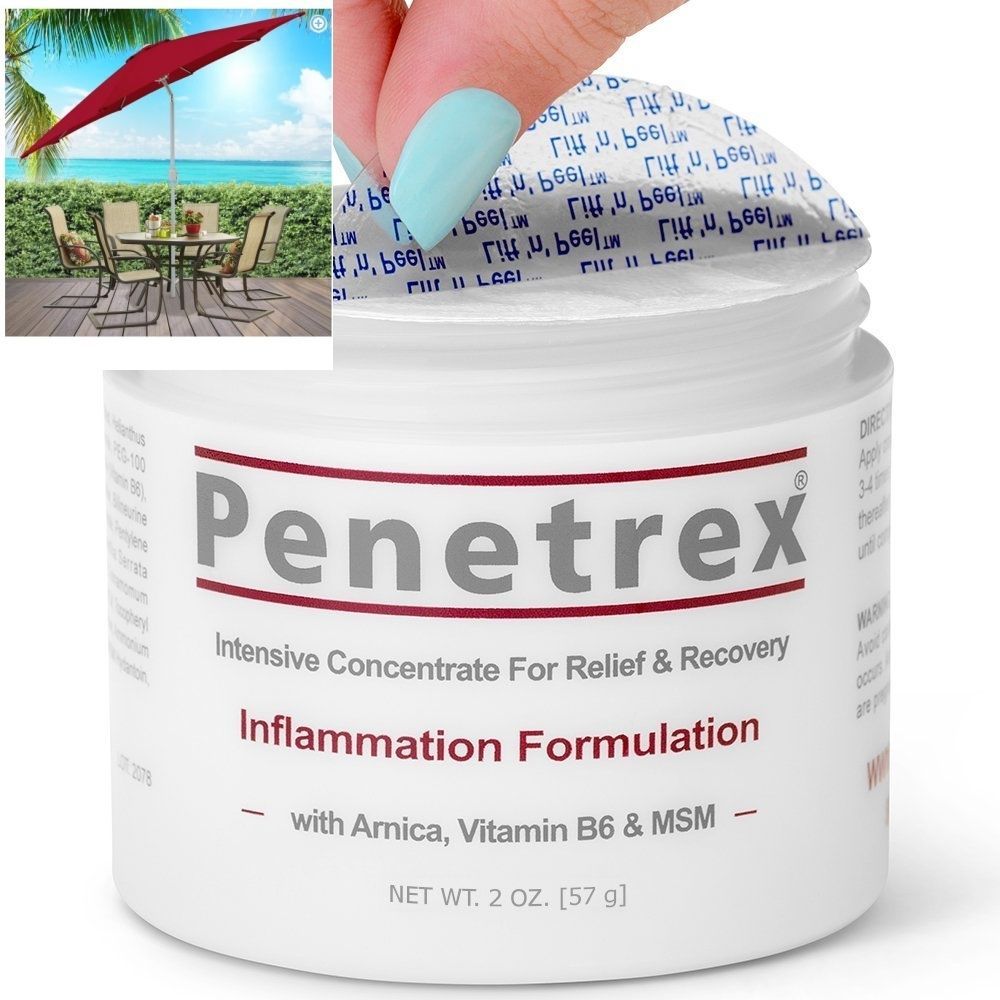
What Situations Call For Topicals For Psa
Before you load your shopping cart with tubes of ointment and boxes of sticky patches, you should know that not every topical medication is safe or effective for everyone with PsA. The rule of thumb here is to talk to your doctor first. Tell them about your pain and they can suggest topicals that might work for the aches or stiffness you’re having. They also can discuss potential side effects of any new topicals you’re thinking of trying and can cross reference them against other drugs you’re taking to manage your PsA or other health conditions, to make sure all potential interactions are safe. Then check with your insurance to see what might be covered via prescription. Now, let’s dig into the products.
Things To Consider When Taking A Biologic
Biologics are a type of medication that can be prescribed for some forms of inflammatory arthritis .
This sheet gives you general information about how biologics work, why they are used, as well as tips on the safe use of these medications.
This resource does not provide advice about the specific biologic you may be prescribed to manage your arthritis. It does not cover all the side effects and safety precautions that can occur with each biologic. You should discuss this with your doctor, rheumatology nurse or pharmacist, or see the For more information section at the end of this resource.
You May Like: Is Red Wine Bad For Arthritis
Causes Of Psoriatic Arthritis
Almost 1 in 3 people with psoriasis also have psoriatic arthritis.
It tends to develop 5 to 10 years after psoriasis is diagnosed, although some people may have problems with their joints before they notice any skin-related symptoms.
Like psoriasis, psoriatic arthritis is thought to happen as a result of the immune system mistakenly attacking healthy tissue.
But it’s not clear why some people with psoriasis develop psoriatic arthritis and others do not.
Psoriatic Arthritis And Psoriasis: Which Comes First
People with psoriatic arthritis almost always have psoriasis first, says Francis C. Luk, MD, a rheumatologist at Wake Forest Baptist Health in Winston-Salem, North Carolina. There is a small percentage of people who will actually get the arthritis first, but thats a minority of cases, says Dr. Luk.
Its estimated that about 30 percent of people with psoriasis go on to develop psoriatic arthritis, according to the National Psoriasis Foundation. The first signs of arthritis are often swelling and pain in the hands, but the disease can cause early symptoms in other parts of the body too. Feet, knees, or ankles pretty much any joint can be involved in the arthritis, Luk says.
Symptoms of psoriasis and psoriatic arthritis can flare or subside at different times, according to the American College of Rheumatology. Either condition can be mild, moderate, or severe for instance, you can have severe psoriasis and mild psoriatic arthritis, or vice versa. The disorders might target the same or different parts of the body you could have psoriasis lesions on your elbows, say, but no pain in your elbow joints. When the two conditions flare at the same time, one may be worse than the other, according to an overview published in the American Journal of Managed Care.
Read Also: Is Heat Good For Arthritis
When To Get Medical Advice
See a GP if you have persistent pain, swelling or stiffness in your joints even if you have not been diagnosed with psoriasis.
If you’ve been diagnosed with psoriasis, you should have check-ups at least once a year to monitor your condition. Make sure you let the doctor know if you’re experiencing any problems with your joints.
What To Know About Insurance
One of the biggest challenges in your PsA treatment may be getting insurance approval. Most insurance companies require you to first try and fail a cheaper drug before theyll pay for something more expensive like a biologic, says Dr. Shoor. What is or isnt covered varies by insurer. Talk with your doctors billing department about any questions or concerns you have they may be able to help you get coverage for the medications you need.
You May Like: Is Arthritis And Autoimmune Disease
Treatment Options For Psoriatic Arthritis
A combination of medication, exercise, and complementary therapies can improve skin symptoms and joint pain.
Treating psoriatic arthritis is tricky because this disease affects both the skin and joints. PsA treatment includes a combination of medication and non-drug therapies like exercise, massage, heat and cold. Its personalized to your symptoms and the severity of your disease.
The goals of treatment are to
- Slow the disease and possibly put it into remission
- Relieve pain and other symptoms
- Protect your skin and joints
You may need to see a team of specialists, including a rheumatologist to manage joint pain and a dermatologist for skin symptoms. Work with your medical team to find the treatment approach that works for you.
Medications
Medicines are an important part of treating PsA. They may include some or all of the following:
Physical Therapy and Exercise
Exercise is an important part of treating PsA. Staying active relieves pain and stiffness, boosts energy and mood, and improves overall health and function. The ideal workout program for PsA includes a mix of aerobic exercises, strength training and stretching.
Living With PsA
In addition to medication, exercise and physical therapy, you can do a few things on your own to relieve symptoms and minimize the impact of PsA on your life.
Psoriatic Arthritis Related Articles
Your Psoriatic Arthritis Treatment Options

There are many treatments that may give you relief, so its important to talk with your doctor to find the right one. The type of psoriatic arthritis you have, its severity, and your reaction to treatment will help determine what treatment is best for you.
Some options for treatment include:
- Nonsteroidal Anti-Inflammatory Drugs : Over-the-counter medications like aspirin and ibuprofen, but can also include prescription products, which help to reduce inflammation, joint pain, and stiffness
- Disease-Modifying Antirheumatic Drugs : Typically for more severe symptoms, these attempt to slow or stop joint/tissue damage and the progression of psoriatic arthritis
- Biologics: Protein-based medicines produced from living cells that target specific parts of the immune system
âFor people like me with psoriatic arthritis, I would tell them to go on the website, and do your research.â
â Patti, actual Taltz patient with psoriatic arthritis.
Patti was compensated for her time.
PURPOSE AND SAFETY SUMMARY
Important Facts About Taltz® . It is a prescription medicine also known as ixekizumab.
Taltz is an injectable medicine used to treat:
- People 6 years of age and older with moderate to severe plaque psoriasis who may benefit from taking injections or pills or treatment using ultraviolet or UV light .
- Adults with active psoriatic arthritis.
- Adults with active ankylosing spondylitis.
- Adults with active non-radiographic axial spondyloarthritis with objective signs of inflammation.
WARNINGS
Recommended Reading: Which Is Better For Arthritis Tylenol Or Aleve
Take Pain Medications For Psoriatic Arthritis
Over-the-counter pain medications such as ibuprofen and naproxen are often used to manage pain in psoriatic arthritis. If those don’t provide enough relief, John M. Davis, III, MD, a rheumatologist at the Mayo Clinic in Rochester, Minnesota, also recommends trying non-narcotic prescription medications, which change the way the brain’s pain center processes certain proteins that trigger pain. Although these drugs aren’t narcotics, side effects can include stomach upset and bad dreams.
Other medications to treat psoriatic arthritis include traditional disease-modifying anti-rheumatic drugs and biologic therapies, which can help ease pain and slow joint damage. Always follow your treatment plan as prescribed and talk to your doctor before taking a pain medication.
What Counts As A Topical Pain Medication
Topicals come in patches, gels, sprays, or creams but they all work the same way: by delivering treatment through the skin. Most topical pain relievers sold to relieve psoriatic arthritis pain fall into one of three categories: Counterirritants, nonsteroidal anti-inflammatory drugs , or lidocaine products, says Draper. Lets explore these categories and list some products that are worth a try.
Recommended Reading: Is Arthritis In The Bones Or Muscles
There Are Many Drug Options For Managing Active Psa Heres What Happened When A Study Compared Them With Each Other
New psoriatic arthritis treatment guidelines from the American College of Rheumatology say that most people with active psoriatic arthritis should choose an anti-TNF drug, such as adalimumab or infliximab , as their first line of therapy.
If a patient doesnt respond well to one or more of these drugs or cant take them for some reason, they might then consider a newer type of biologic an interleukin inhibitor like ustekinumab or secukinumab .
Although interleukin inhibitors have also been proven to help patients with psoriatic arthritis, there havent been many large studies directly measuring them against anti-TNF drugs.
A new study published in the Journal of Rheumatology aimed to compare these classes of medication in terms of how well they work for two specific complications of psoriatic arthritis: enthesitis and dactylitis .
This study, a literature review that analyzed data from 18 previous trials, included information on a total of nearly 7,000 psoriatic arthritis patients who had enthesitis and dactylitis. Researchers determined that both types of drugs beat out placebos and that they worked equally well for PsA patients with enthesitis and dactylitis.
After 24 weeks, the anti-TNF drugs demonstrated significant resolution of these complications, the authors reported. The two classes also worked similarly in terms of improving disease activity scores as well as quality of life scores.
Pharmacoeconomic Issues And Biosimilars
Biosimilars to INF and ETN are currently licensed for PsA treatment.
Although their impact on rheumatic diseases has been remarkable, biological drugs are a very large financial burden for payers. Since a number of patents pertaining to certain biological drugs are expiring, there is a growing interest in developing biosimilar agents. However, it is expected that the decline of biological originator therapies will not be as strong as that given by the introduction of generics for brand synthetic drugs.,
According to the World Health Organization, a biosimilar is a biotherapeutic product which is similar in terms of quality, safety, and efficacy to an already licensed reference biotherapeutic product. The FDA and the EMA agree that at least 1 adequately powered equivalence trial is necessary to demonstrate biosimilarity. Both the agencies indicate the importance of equivalence trial more than non-inferiority one, whereas a challenge remains how powerful an RCT should be to demonstrate safety.,
PLANETAS is another study evaluating the appearance of adverse events in ankylosing spondylitis patients who remain in INF and those who transit to CT-P13. The rates of infusion-related reactions seem to be similar . RCTs for biosimilars appear to be underpowered for identifying unexpected adverse events since they usually enroll fewer than 600 participants. For this reason, careful postmarking pharmacovigilance is particularly important.
You May Like: How Long Does Arthritis Pain Last
What Are Biologic Dmards
Biologic DMARDs are drugs made from living cells. These cells can come from parts of the blood, proteins, viruses, or tissue. This process creates drugs that can prevent, treat, and cure disease. In people with PsA, they work by interfering with specific substances in the immune system to reduce or better regulate the inflammatory responses that cause PsA and psoriasis symptoms. Common proteins targeted include tumor necrosis factor and various interleukins . Biologic DMARDs include:2,5
Also Check: Best Remedy For Arthritis In Hands
Treatment Options Reality Check
Internists may like to treat patients with mild psoriatic arthritis with NSAIDs to reduce pain and swelling, said Dr. Raychaudhuri. However, ideally psoriatic arthritis patients should be treated with the broader goal of preventing joint destruction, so they should be referred quickly, within a few weeks, to a rheumatologist with psoriatic arthritis expertise, he said.
Now that therapies are available to address and even prevent joint damage, internists should be conscious of the six-month window available to start treatment before that damage occurs, said Dr. Orbai. Even if only one joint , take it seriously, she said. If we don’t treat the inflammation, more joints will become involved.
For example, Dr. Mehta told the story of a patient, a deli owner in his 50s, who had psoriasis and reported that he couldn’t make sandwiches anymore because his fingers were deformed. He had seen physicians for five years and was never told his hand pain could be psoriatic arthritis. Dr. Mehta did a scan and found psoriatic arthritis throughout the patient’s body.
While internists may not be making specific drug treatment decisions, knowing the options will help inform their conversations with patients, said Jasvinder A. Singh, MD, MPH, lead author of the guideline and professor of medicine and epidemiology at the University of Alabama at Birmingham.
Read Also: Can Sugar Cause Arthritis Flare Up
When Joints Are Damaged
Although rare, some with PsA opt for surgical treatment when the condition causes significant damage to the joints. However, surgery is typically a last resort. Research shows that fewer than 10% of people with PsA need surgical treatment.
Some common PsA surgical procedures include:
- Joint fusion: Joint fusion is a procedure that fuses the ends of two joints together to a fixed position. The procedure can offer pain relief by stabilizing the joint and preventing movements that may be causing pain. However, the procedure can also limit the mobility of a joint.
- Synovectomy: Sometimes, the synovial membrane becomes inflamed and does not respond to medication, resulting in persistent pain. With synovectomy, all or part of the joint lining is removed. The procedure is typically considered when joint inflammation doesn’t respond to drugs.
- Joint replacement: Joint replacement surgery involves replacing part or all of a joint with an artificial one to restore joint function. This procedure is commonly done on large joints, such as the hips and knees.
Work And Psoriatic Arthritis
Having psoriatic arthritis may make some aspects of working life more challenging. But, if youre on the right treatment, its certainly possible to continue working.
Help and support is available, and you have rights and options.
The Government scheme Access to Work is a grant that can pay for equipment to help you with activities such as answering the phone, going to meetings, and getting to and from work.
The 2010 Equality Act, and the Disability Discrimination Act in Northern Ireland makes it unlawful for employers to treat anyone with a disability less favourably than anyone else. Psoriatic arthritis can be classed as a disability if its making every-day tasks difficult.
Your employer may need to make adjustments to your working environment, so you can do your job comfortably and safely.
You might be able to change some aspects of your job or working arrangements, or train for a different role.
In order to get the support youre entitled to, youll need to tell your employer about your condition. Your manager or HR department might be a good place to start.
Other available support might include:
- your workplace occupational health department, if there is one
- an occupational therapist. You could be referred to one by your GP or you could see one privately
- disability employment advisors, or other staff, at your local JobCentre Plus
- a Citizens Advice bureau particularly if you feel youre not getting the support youre entitled to.
Read Also: What Is The Best Supplement To Take For Arthritis