How Is Systemic Juvenile Idiopathic Arthritis Diagnosed
To diagnose systemic JIA, doctors:
- ask about symptoms
- ask whether other family members have had similar problems
- do X-rays or other imaging studies to look inside the joints
- order blood tests to check for:
- anemia or other blood problems
- inflammation in the body
Sometimes, an orthopedic surgeon takes samples of joint fluid or synovium . The sample is sent to a lab for testing.
How Is Juvenile Idiopathic Arthritis Treated
The goal of treatment is to reduce pain and stiffness, and help your child keep as normal a lifestyle as possible.
Treatment will depend on your childs symptoms, age, and general health. It will also depend on how severe the condition is.
Treatment may include medicines such as:
- Nonsteroidal anti-inflammatory medicines , to reduce pain and inflammation
- Disease-modifying antirheumatic medicines , such as methotrexate, to ease inflammation and control JIA
- Corticosteroid medicines, to reduce inflammation and severe symptoms
- Medicines called biologics that interfere with the body’s inflammatory response. They are used if other treatment isnt working.
Talk with your childs healthcare provider about the risks, benefits, and possible side effects of all medicines.
Other treatments and lifestyle changes may include:
- Physical therapy, to improve and maintain muscle and joint function
- Occupational therapy, to improve ability to do activities of daily living
- Nutrition counseling
- Regular eye exams to find early eye changes from inflammation
- Regular exercise and weight control
- Getting enough rest
- Learning to use large joints instead of small joints to move or carry things
How Is Sjia Treated
There is no cure for SJIA, but there are treatments which can reduce the severity of the symptoms and even make remission possible.1 Doctors are so much better equipped to help people with SJIA than they were 20 years ago.
- NSAIDs can reduce the pain, inflammation and stiffness caused by SJIA
- Corticosteroids lower inflammation
- Biologics may be prescribed1 to target and block inflammation-causing substances in the body
Exercise is an important part of the SJIA treatment process, as it will help build muscle strength, increase energy and reduce pain.
Good communication with doctors and specialists will help provide a better understanding of the diagnosis and the treatment options available.
Monitoring
Read Also: What Is The Best Natural Remedy For Rheumatoid Arthritis
Different Types Of Juvenile Idiopathic Arthritis
There are three kinds. Each type is based on the number of joints involved, the symptoms, and certain antibodies that may be in the blood.
Itâs the most common form. About half of all children with juvenile idiopathic arthritis have this type.
It usually affects large joints like the knees. Girls under age 8 are most likely to get it.
Some children with this type have special proteins in the blood called antinuclear antibodies. They are more likely to get eye diseases like iritis, which is inflammation of the iris, or colored part of the eye. They can also get uveitis, which is inflammation of the inner eye. These children need regular eye exams by an ophthalmologist, a doctor who specializes in eye diseases.
Lots of children with this condition will outgrow it by adulthood. Still, eye problems can continue, and joint symptoms may come back.
About 30% of all children with juvenile idiopathic arthritis have this type. It usually affects the small joints, like those in the hands and feet, but it can sometimes involve the large joints.
This type of juvenile idiopathic arthritis is usually symmetrical. That means it affects the same joints on both sides of the body.
Distinct Phenotypes Of Monocytes And Macrophages In Sjia/mas
Another intriguing finding in the study performed by Fall et al is the co-regulated expression of the genes involved in the negative feedback regulation of innate immune responses including SOCS3 and the markers of the alternative pathway of macrophage differentiation . This is consistent with the recent reports describing expansion of alternatively activated CD163+ macrophages in the bone marrow of a large proportion of patients with new onset systemic JIA . Since hemophagocytic macrophages seen in MAS also express CD163, this feature may provide some new clues to the understanding of the high prevalence of MAS in systemic JIA .
Read Also: Is Arthritis Treatable Or Curable
Causes And Risk Factors Of Juvenile Idiopathic Arthritis
Theres no solid answer right now about why JIA develops, experts say. Some families develop a collection of autoimmune conditions, though not usually the same ones, and JIA can be one of those diagnoses, says Dr. Sura. Other families have no history of any autoimmune disease when it is diagnosed.
Some believe JIA happens as a combination of genetics and some environmental triggers, says Dr. Mehta, but we dont know what they are. There are some genes that are identified as having a potential role, but not everyone with those genes gets arthritis, and not all with arthritis have those genes.
Study Design And Participants
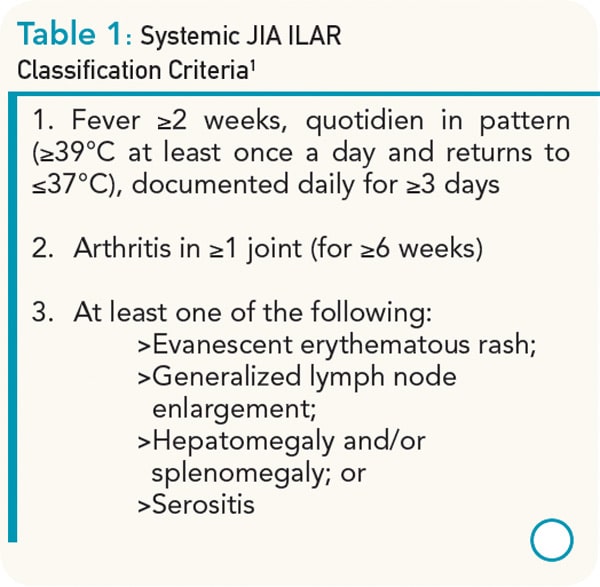
Peripheral blood specimens were collected from children diagnosed with sJIA according to the International League of Associations for Rheumatology criteria by paediatric rheumatologists at participating medical centres in nine countries . Blood samples were also obtained from geographically matched control subjects. In addition, single nucleotide polymorphism genotype data from geographically matched control populations were used, when available. The INCHARGE project was granted institutional review board approval by the University of Manchester. Subjects were enrolled in accordance with all local ethics regulations, with the approval of local IRBs at each contributing medical centre, and with informed parental consent.
You May Like: Can You Have Arthritis In Your Buttocks
Enhancing Healthcare Team Outcomes
A recent study was realized by the collaboration between physicians and patient associations. A questionnaire was proposed to 622 parents in 23 European countries. The questions covered various domains of JIA care, including demographics, diagnosis, referrals to different health care professionals, access to pain and fatigue management and support groups, the information they received about the disease, and awareness of and participation in research.
The data furnished a view on JIA patients and their parents perspectives regarding the care they receive. Its essential to increase the awareness of the existence of supportive care, such as pain and fatigue management, as well as support groups, or to start new initiatives where these are lacking. .
Pediatric pharmacists review medications and provide patient and family education about the importance of compliance and potential side effects, and report any concerns to the clinician staff. Pediatric and rehabilitation nurses provide direct care and facilitate communication between the interprofessional health team members. This type of collaboration among team members will lead to better outcomes for these patients.
What Other Problems Can Happen
Rarely, kids with JIA can get a life-threatening problem called macrophage activation syndrome. It happens when the immune system becomes too active and damages some of the bodys organs. It can lead to severe diarrhea, bleeding, hearing loss, confusion, and seizures.
Macrophage activation syndrome needs treatment right away:
- Go to the emergency room if your child has severe diarrhea, bleeding, confusion, or seizures, or seems very sleepy.
Also Check: What Is The Best Medicine For Arthritis In The Knees
What Causes Systemic Juvenile Idiopathic Arthritis
All types of JIA happen when the immune system, which normally attacks germs, mistakenly attacks the joints. This causes inflammation in the joints and other problems.
Systemic JIA can start anytime in kids 1 to 16 years old. Most cases start when a child is around 2 years old. The condition affects boys and girls equally.
Doctors dont know exactly why kids and teens get JIA. Idiopathic means from an unknown cause. It can run in families but often does not. Its likely due to a combination of:
- the way the immune system responds to infection and illness
- a trigger, such as an infection
What Are The Complications Of Juvenile Idiopathic Arthritis
Musculoskeletal complications may occur secondary to ongoing inflammation and poor disease control, including:
- A leg-length discrepancy
- Sacroiliac joint and spine ankylosis .
Sometimes JIA may result in more severe complications with devastating outcomes. These may include:
- Uveitis this may lead to vision loss screening and close monitoring by a paediatricophthalmologist is warranted for severe, active uveitis
- Macrophage activation syndrome this may be life-threatening it is characterised by fever, cytopenias, liver dysfunction, coagulopathy, purpura, hypofibrinogenaemia , hypertriglyceridaemia , and a very high level of ferritin .
Don’t Miss: How Do I Relieve Arthritis Pain
Why Is Research Important For Rare Diseases
Research increases what we know about rare diseases so that people can get a diagnosis more quickly and can know what to expect. Research also helps doctors better understand how well a treatment works and can lead to new treatment discoveries. It may even help improve diagnosis and treatment of more common diseases.
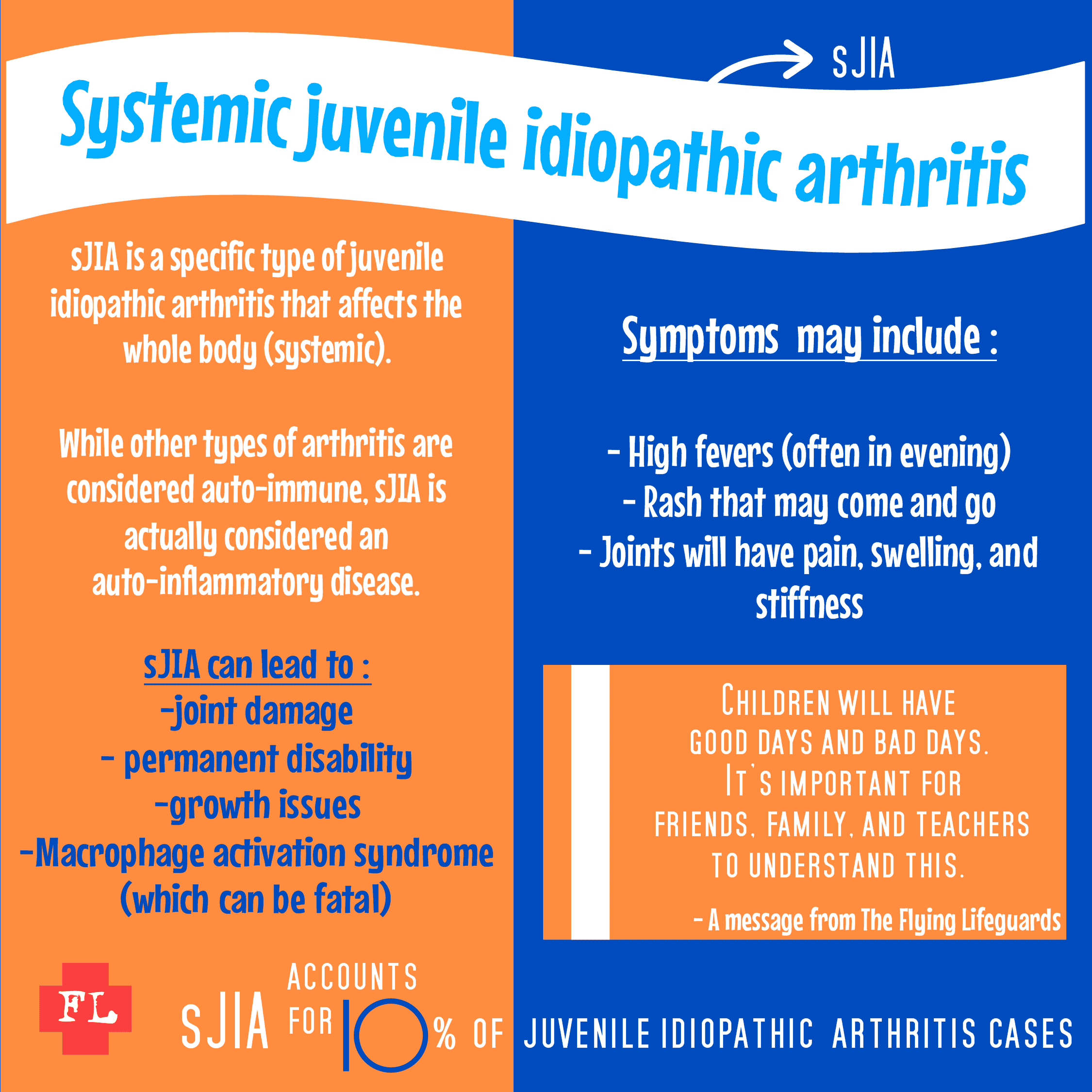
Sjia As An Autoinflammatory Disease

The emerging consensus in pediatric rheumatology is that since the abnormalities in the innate immunity play a major role in the pathogenesis of SJIA this disease should be viewed as an autoinflammatory syndrome rather than a classic autoimmune disease. Indeed, many clinical features of SJIA are similar to those seen in autoinflammatory syndromes . This includes fever, multisystem involvement as well as a polycyclic course in some patients. Autoreactive lymphocytes are usually not detected in systemic JIA patients. Only rare patients have positive ANA test. Rheumatoid Factor is usually absent. Finally, as in autoinflammatory syndromes, patients with SJIA are at risk for amyloidosis.
On a genomic level, one distinctive feature of the systemic form of JIA is the lack of strong MHC Class II associations . This is very different from other clinical forms of JIA in which the contribution of the MHC genes is quite significant. In fact, a recently completed genome-wide screen showed that most of the genetic predisposition to oligo-JIA is contributed by the MHC loci . In contrast in systemic JIA, the most consistently reported genetic effects have been limited mainly to mild contributions from cytokine/chemokine gene polymorphisms involving the promoter elements and genes encoding TNF-, IL-6 and MIF .
Also Check: What Is Better For Arthritis Hot Or Cold
Identification Of Potential Jia Cases And Training Set
We identified 3190 potential JIA cases in the de-identified EHR by requiring 1 count of JIA ICD-9 or ICD-10-CM codes . A training set of 200 charts was randomly selected from these cases. We performed chart review on the training set and found 95 true JIA cases and 105 non-JIA cases. The kappa statistic for chart review between the Doctor of Pharmacy candidate and pediatric rheumatologist was 0.96. Of the 105 non-JIA cases, 8 had a diagnosis of a connective tissue
Alternative And Complementary Therapies
In early 2022, however, the American College of Rheumatology published guidelines for nondrug treatments for all people living with JIA. These cover physical and occupational therapy as needed, eating a well-balanced and healthy diet as it relates to ones age, and lab tests both before starting and during treatment with new JIA medication to determine if the drugs are effective. The ACR guidance also urges people with JIA and the people they live with to stay up-to-date on all recommended vaccinations, including annual flu shots and ongoing COVID-19 shots as directed by public health experts.
What I tell families is that they are welcome to try diet interventions, but there are no randomized control studies for juvenile idiopathic arthritis, says Mehta. If something works, Im super happy for them, but it has to be a complement to the standard-of-care medicines. In other words, such therapies help when they supplement but never replace drug treatment.
Always speak with your childs physician about what methods you may incorporate and in what capacity.
Don’t Miss: What Kind Of Food To Avoid When You Have Arthritis
Overview Of Juvenile Idiopathic Arthritis
Like adults, children can develop arthritis. The most common type of chronic, or long-lasting, arthritis that affects children is called juvenile idiopathic arthritis . JIA broadly refers to several different chronic disorders involving inflammation of joints , which can cause joint pain, swelling, warmth, stiffness, and loss of motion. The various forms of JIA have different features, such as the pattern of joints involved and inflammation of other parts of the body besides the joints. JIA may last a limited time, such as a few months or years, but in some cases it is a lifelong disease that requires treatment into adulthood.
JIA is idiopathic, meaning that its origins are not understood. While the exact causes of JIA are unknown, it begins when the immune system becomes overactive and creates inflammation.
With treatment, most children achieve periods of wellness , and sometimes the disease goes away permanently with no further need for medications. It is important to see a doctor early if your child has swollen or stiff joints because delaying therapy can lead to joint damage, a lesser response to treatment, and other problems.
Sexual Differences In Frequency
Girls with an oligoarticular onset outnumber boys by a ratio of 3:1. In children with uveitis, the ratio of girls to boys is 5-6.6:1, and in children with polyarticular onset, girls outnumber boys by 2.8:1. In striking contrast, systemic-onset occurs with equal frequency in boys and girls. Boys outnumber girls with enthesitis-related arthritis.
Read Also: How To Reduce Rheumatoid Arthritis Inflammation
How Can Parents Help
Systemic JIA usually is a lifelong disease, but treatments can help ease pain, keep kids active, and prevent long-term joint damage. To help your child:
- Be sure your child takes all medicines exactly as directed.
- Work with the physical therapist to develop a regular exercise program. This will help keep your childs muscles strong and flexible.
- Learn all you can about systemic JIA with your child. Your care team is a great resource. You also can find information and support online at:
Systemic Juvenile Idiopathic Arthritis :
Weight less than 30 kg: 12 mg/kg.
Weight equal to or more than 30 kg:
8 mg/kg. Administer as an IV infusion once every 2 weeks. May be used as an IV infusion or as a SC injection alone or in combination with methotrexate. Do not adjust dose based on a single-visit body weight weight may fluctuate. See prescribing information for SC dosing and intervals. When transitioning from IV to SC administration, administer the first SC dose instead of the next scheduled IV dose
M. Batthish, R. Schneider, in, 2016
Read Also: Is Bike Riding Good For Knee Arthritis
What Is The Treatment For Juvenile Idiopathic Arthritis
Treatment of systemic JIA is directed at symptom management, improving or managing joint function, and minimising complications. Non-steroidal anti-inflammatory drugs are typically the first-line agents for mild articular or extra-articular presentations to control pain. Other pharmacological agents include:
- Oral corticosteroids for moderate to severe disease.
- Intravenous corticosteroids these may be required in patients with severe flare-up or complications, such as MAS.
- Disease-modifying anti-rheumatic drugs , such as methotrexate, ciclosporin, and leflunomide.
Drugs that block inflammatory cytokines, such as TNF-, IL-6, and IL-1, have proven efficacy, especially in longstanding JIA. These include:
- Anakinra an IL-1 receptor antagonist
- Canakinumab a humanised monoclonal antibody directed against IL-1
- Tocilizumab this humanoid monoclonal antibody blocks IL-6 .
What Are The Symptoms Of Juvenile Idiopathic Arthritis
Symptoms may appear during episodes . Or they may be ongoing . Each childs symptoms can vary. Symptoms may include:
- Swollen, stiff, and painful joints in the knees, hands, feet, ankles, shoulders, elbows, or other joints, often in the morning or after a nap
- Eye inflammation
- High fever and rash
- Swollen lymph nodes
These symptoms can seem like other health conditions. Make sure your child sees his or her healthcare provider for a diagnosis.
Recommended Reading: What To Take For Arthritis In Hands
Physical Effects Of Systemic Juvenile Idiopathic Arthritis
Systemic juvenile idiopathic arthritis is a rare and serious subtype of juvenile idiopathic arthritis that causes inflammation throughout the body.
Juvenile idiopathic arthritis is the most common type of arthritis in children and teens. Between 10% to 20%of children with JIA have a rare and serious subtype called systemic juvenile idiopathic arthritis . Symptoms of this rare disease can include overactivation of a type of immune cells called macrophages , unremitting fever, liver and spleen enlargement, abnormal bleeding, central nervous system dysfunction and other potential complications. Read about one familys plight.
Today, 9-year-old Cohen is having the time of his life. He is president of the barn on the ranch where his family now lives in New Mexico. He takes care of 13 goats, five sheep and eight pigs. He loves playing dodgeball, playing with other kids on the ranch, especially his older friends, Kylie and Mikela, who understand what he deals with, and cheering on the Kansas City Chiefs.
I love living here, Cohen says. I wont ever leave because I dont hurt here.
Cohen was just 2 years old when we knew something wasnt right, his mother says. He started vomiting and developed rashes and swelling in random areas of his body, accompanied by high fevers. The first joints affected were his ankles. Soon it spread to his fingers and elbows. Finally, Cohen was diagnosed with SJIA.
Tony Williams
What Causes Juvenile Idiopathic Arthritis
The exact cause of JIA is unclear, but a pronounced immune response in a perpetuating loop of both innate and adaptive immunity is believed to contribute to the pathogenesis of JIA. Aberrant activation of the innate immune system lead to the dysregulated production of proinflammatorycytokines. Tumournecrosis factor alpha , interleukin -1, and IL-6 play a critical inciting role. The effects of these cytokines provide explanations for the various clinical features seen in systemic JIA. These effects include:
- Bone marrow granulopoiesis
- Increase in osteoclast activity
- Hepatocyte stimulation
- Activation of thermoregulatory functions .
The increased recruitment of inflammatory cells in the joint synovial membrane was demonstrated in several studies by a significant elevation of proinflammatory cytokines in the synovial fluid of affected children. Proinflammatory cytokines in the synovium lead to increased production and accumulation of synovial fluid and thickening of the synovial lining. This chronic synovial inflammation is apparent and common to all JIA subtypes. In addition, RANKL cytokine, which is associated with bone resorption and cartilage damage, was reported to be present in large amounts in the synovial membrane of children with JIA.
Environmental factors may contribute to the development of JIA. Some studies have suggested associations with exposure to antibiotics, a bacterialinfection in immunosuppressed individuals, and maternal smoking during pregnancy .
Don’t Miss: How To Fix Arthritis In Fingers