How Is Osteoarthritis Managed
There is no cure for osteoarthritis, but most people with osteoarthritis can manage their symptoms, continue with daily activities and live healthy and enjoyable lives. Be careful of any products or treatments that claim to cure osteoarthritis completely your doctor will help to find the right treatment for you.
The Australian Commission on Safety and Quality in Health Care has developed a guide to help you discuss the main treatment options for osteoarthritis of the knee with your doctor.
Also Check: Why Do Knees Crack When Squatting
What Are The Risk Factors For Developing Rheumatoid Arthritis
There are several risk factors for developing rheumatoid arthritis. These include:
- Family history: Youre more likely to develop RA if you have a close relative who also has it.
- Sex: Women and people designated female at birth are two to three times more likely to develop rheumatoid arthritis.
- Smoking:Smoking increases a persons risk of rheumatoid arthritis and makes the disease worse.
- Obesity: Your chances of developing RA are higher if you have obesity.
How Can A Physical Therapist Help
Once you have received a diagnosis of knee OA, your physical therapist will design an individualized treatment program specific to the exact nature of your condition and your goals. Your treatment program may include:
Range-of-motion exercises. Abnormal motion of the knee joint can lead to a worsening of OA symptoms when there is additional stress on the joint. Your physical therapist will assess your kneeâs range of motion compared with expected normal motion and the motion of the knee on your uninvolved leg. Your range-of-motion exercises will focus on improving your ability to bend and straighten your knee, as well as improve your flexibility to allow for increased motion.
Muscle strengthening. Strengthening the muscles around your knee will be an essential part of your rehabilitation program. Individuals with knee OA who adhere to strengthening programs have been shown to have less pain and an improved overall quality of life. There are several factors that influence the health of a joint: the quality of the cartilage that lines the bones, the tissue within and around the joints, and the associated muscles. Due to the wear and tear on cartilage associated with knee OA, maintaining strength in the muscles near the joint is crucial to preserve joint health. For example, as the muscles along the front and back of your thigh cross the knee joint, they help control the motion and forces that are applied to the bones.
Read Also: What Vegetable Is Bad For Arthritis
Other Injections: Hyaluronic Acid Botox And More
Some people have used other types of injections for OA of the knee.
However, experts from the American College of Rheumatology and the Arthritis Foundation dont currently recommend using these, as theres not enough evidence that they work.
Examples of other types of injections include:
- hyaluronic acid injections, also known as viscosupplementation
You may not know exactly what type of injection youre receiving or what the effect might be.
Always discuss the pros and cons of any treatment with your doctor before starting, so that you can make an informed decision.
You May Like: Inversion Table Benefits For Knees
While Oa And Inflammatory Arthritis Do Share Some Symptoms Namely Pain Tenderness And Swelling The Similarities Tend To End There
If you have persistent knee joint pain, arthritis in your knees could be the culprit. While many forms of arthritis exist, its usually fairly easy for your doctor to first determine which of the two main categories osteoarthritis or inflammatory/autoimmune arthritis you might have.
Those include whats known as mechanical knee arthritis or inflammatory/autoimmune knee arthritis, which includes a number of illnesses such as rheumatoid arthritis , psoriatic arthritis, and ankylosing spondylitis.
While OA and inflammatory arthritis do share some symptoms namely pain, tenderness, and swelling the similarities tend to end there, as youll see below. The answers to the following questions can often help determine if your knee pain is osteoarthritis or inflammatory arthritis.
Also Check: Bioknee Cost
You May Like: Can Arthritis Be In Your Muscles
Diagnosing Arthritis In The Knee Or Other Joints
Diagnosing arthritis starts with a physical exam. However, correctly diagnosing the condition in its early stages can be tricky.
The following diagnostic tests can help your orthopedic doctor examine your joint closely and arrive at an accurate diagnosis:
- X-ray imaging can create images of your bones to show damage, cartilage loss, and bone spurs, and is often used to track arthritis progression.
- Magnetic resonance imaging produces detailed cross-sectional images of tissues throughout the body, including tendons, ligaments, and cartilage.
- Computerized tomography scan can create three-dimensional images of bones and surrounding tissues by combining X-ray images taken from different angles.
- Ultrasound produces images of soft tissues, bursae, and cartilage via high-frequency sound waves.
- Bone scan can detect the presence of arthritis by identifying areas of chemical and physical changes or abnormalities in the bone.
Osteoarthritis Of The Knee
Knee OA is a very common source of pain that can limit your mobility.
Causes of Knee OA
The cause of OA is unknown. These risk factors make it more likely you will develop knee OA:
- Age: OA can occur at any time of life, but it is most common in older adults.
- Sex: Women are more likely to have knee OA than men.
- Obesity: Being overweight adds stress to your knees. Fat cells also make proteins that can cause inflammation in and around your joints.
- Injuries: Any knee injury, even old ones, can lead to knee OA.
- Repeated stress: Frequent stress on your knee from your job or playing sports can increase risk for OA.
- Genetics: You can inherit a tendency to develop OA.
- Bone deformities: If you have crooked bones or joints, you are at higher risk.
- Some metabolic diseases: Diabetes and hemochromatosis, a condition in which your blood has too much iron, have been linked to OA
Symptoms of knee OA develop slowly and worsen over time.
- Pain: Movement causes pain. Sometimes your knee will ache while sitting still.
- Stiffness: Your knees may be stiff first thing in the morning or after sitting for a long time.
- Loss of motion: Over time, you may lose the ability to bend and straighten your knee all the way.
- Creaking and grating : You may hear crackling noises or feel a grating sensation.
- Instability: Your knee may give out or buckle, or feel like it could.
- Locking: The knee may lock or stick.
- Swelling: Your knee may get puffy all around or on one side.
Your doctor will check for:
Don’t Miss: How To Beat Arthritis Naturally
Rheumatoid Factor And Anti
Specific blood tests can help to diagnosis rheumatoid arthritis, but are not accurate in every person. About half of all people with rheumatoid arthritis have a positive rheumatoid factor present in their blood when the disease starts, but about one in every 20 people without rheumatoid arthritis also tests positive for this.
Another antibody test known as anti-CCP is also available. People who test positive for anti-CCP are very likely to develop rheumatoid arthritis, but not everybody found to have rheumatoid arthritis has this antibody.
Those who test positive for both rheumatoid factor and anti-CCP may be more likely to have severe rheumatoid arthritis requiring higher levels of treatment.
Complementary And Alternative Therapies
Some people with osteoarthritis try complementary or alternative therapies â such as acupuncture and aromatherapy â and find them helpful, although there is often a lack of medical evidence to suggest they are effective and they generally arenât recommended by the National Institute for Health and Care Excellence .
You May Like: Where To Get Knee High Converse
Don’t Miss: How Many Kinds Of Arthritis Are There
Factors That Predict Cartilage Loss In The Knee
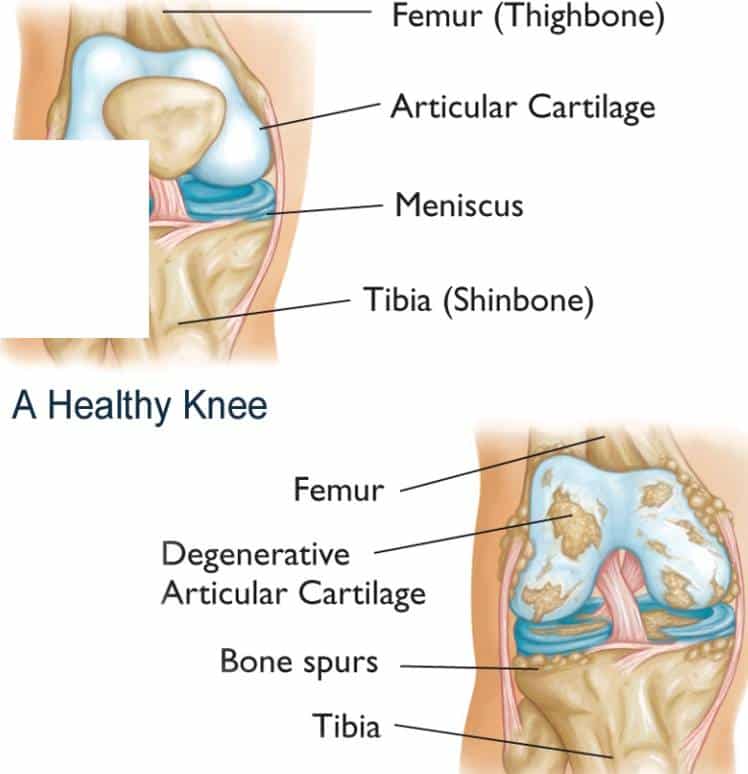
Researchers have analyzed cartilage loss in the knee joint and found that three factors predict it medial meniscal damage, lateral meniscal damage, and varus malalignment of the knee joint.
Another study concurred, revealing that top risk factors that contribute to rapid cartilage loss include cartilage damage, meniscus tears, other injuries to the meniscus, and severe lesions observable on MRI. Synovitis and joint effusion also were predictors of cartilage loss. Interestingly, excess weight was a significant factor as well. For every 1-unit increase in body mass index , the risk of rapid cartilage loss increased by 11%.
You May Like: How Much Does Aflac Pay For Outpatient Surgery
What Does Arthritis In The Knee Feel Like
Millions of Americans suffer from chronic or acute knee pain every year.
Getting a proper diagnosis and receiving the needed treatments can be difficult without knowing the cause of your pain.
Many conditions can mimic one another, so its important to seek a medical professionals advice if you have been battling knee pain.
Arthritis is a prevalent cause of knee pain, and there are a few ways to tell if arthritis is causing your pain.
In the article below, we will answer the question: what does arthritis in the knee feel like?
Arthritis is the inflammation of one or more of your joints.
Joint pain, swelling, and stiffness are the main symptoms of arthritis.
Arthritis can affect any joint in your body, but your knee is particularly vulnerable.
Having arthritis in your knee can make it difficult for you to perform everyday activities, like climbing stairs or walking to the mailbox.
While there are many types of arthritis, the most common types of arthritis are osteoarthritis and rheumatoid arthritis.
Osteoarthritis is the most common form of knee arthritis.
Knee osteoarthritis is a degenerative disease caused by wear and tear.
Its the most common type of arthritis that occurs most often in people over 50, although younger people can get it as well.
The cartilage in your knee joint gradually wears away, and as it wears away, it becomes frayed and rough, and the protective space between the bones decreases.
Recommended Reading: Can You Get On Disability For Rheumatoid Arthritis
Medical Treatments For The Ra/oa Combo
The good news: There are many effective ways to manage RA. The not-so-great news: Treatments for OA are not as advanced, says Dr. Bhatt they temporarily ease pain, but do little to help long-term. Your doctor will likely recommend over-the-counter pain relievers including ibuprofen and acetaminophen or a corticosteroid injected directly into your inflamed joint every three-to-six months. Doctors also often prescribe duloxetine, a depression drug that is also approved to treat OA pain. A recent study, though, found that the drug had no effect in people with chronic knee or hip OA pain.
Symptoms Of Progressive Rheumatoid Arthritis
Here are some general warning signs and symptoms that you may have developed progressive rheumatoid arthritis:
The active state of the disease is becoming more frequent Flare-ups are occurring regularly and lasting for longer periods of time Your pain and swelling are becoming more intense, spreading throughout other areas of your body Your diagnosis occurred early on, and so the disease has had a long time to develop You are beginning to develop rheumatoid nodules that you didnt have before Your blood tests show high levels of Rheumatoid Factor or anti-CCP
If you suspect that your rheumatoid arthritis has become progressive, consult your rheumatologist to determine the changes in your condition and discuss potential adjustments to your treatment plan.
Read Also: Is Turmeric Effective For Arthritis
What Is The Prognosis For People Who Have A Knee Osteotomy
Most people who have a knee osteotomy experience relief from pain and increased function in the knee, which leads to an improved quality of life. In most cases, people do not need to limit their physical activity once they heal from the procedure.
People who have a knee osteotomy can typically return to their usual activities three to six months after the surgery.
Last reviewed by a Cleveland Clinic medical professional on 07/11/2019.
References
What Outcome Can I Expect If I Have Arthritis In My Hands
There is no cure for arthritis. However, you can usually manage mild to moderate symptoms with a combination of medication and non-medication approaches. Surgery may be an option if other treatments fail or the arthritis in your hands is severe. Your healthcare provider will explain what outcome you can expect for your type and severity of arthritis, your age, other existing medical conditions and other factors.
Recommended Reading: Does Aflac Pay For Sprains
Recommended Reading: How Many People Have Psoriatic Arthritis
When Can I Go Back To My Usual Activities After Knee Arthroscopy
Everyone responds to surgery differently. Ask your healthcare provider when you can get back to your daily activities, including driving and walking without assistance. Your healthcare provider may recommend waiting several weeks before doing more physical or strenuous activities.
Sometimes, people need to make changes to their lifestyle and activity level. Some sports can damage your knee. Talk to your healthcare provider about choosing lower-impact sports and activities that are easier on your knee.
Do: Wear Comfortable Knee Joint
There are a fair number of studies that suggest shoe choice matters if you have knee osteoarthritis, Pisetsky says. In fact, flat, flexible shoes that mimic the foots natural mobility can decrease the force placed upon the knee during daily activities, according to a study published in the May 2013 issue of Arthritis and Rheumatology.
Recommended Reading: Knee Brace Infomercial
Recommended Reading: What Is The Difference Between Plaque Psoriasis And Psoriatic Arthritis
What Are The Stages Of Osteoarthritis
There are four stages of osteoarthritis. You probably wouldnt know if you had stage 1. In this stage there is minor wear and tear on your knee joint and possibly some bone spurs forming.
In stage 2 , you will probably begin having minor symptoms like pain when you first get up from sleeping, after sitting for a long time, or after exercise. Your X-rays will begin to show signs of arthritis, and simple remedies like stretching, exercise, and knee braces will ease your symptoms.
Stage 3 is considered moderate arthritis, and your symptoms will be more frequent and more significant. In this stage, the cartilage in the joint is wearing down, the space between the bones of the joint is narrowing, and more bone spurs will develop. In knee arthritis, pain and inflammation will be more pronounced when walking, running, and squatting, and treatments include over-the-counter medications, physical therapy, and possibly therapeutic injections in the joint.
Stage 4 is the most severe form of osteoarthritis and is characterized by a greater degree and increased frequency of pain. This arthritis pain is so severe, it will limit normal activity when it affects the knee anything from enjoying your daily walk to standing while cooking a meal.
People with severe knee arthritis usually get no or very limited relief from noninvasive treatments, and they will usually be recommended to have knee replacement surgery.
How Does Osteoarthritis In The Knee Affect My Body
Knee pain is the most common symptom of osteoarthritis in the knee, making it painful for you to jog, run, climb stairs or kneel. It can also make your knees feel stiff or swollen. Over time, osteoarthritis of the knee can change the shape of your knee joint, making your joint feel unstable or wobbly.
Read Also: How Do You Treat Rheumatoid Arthritis Naturally
How Can I Manage The Symptoms Of Post
The best way to manage your post-traumatic arthritis symptoms is to move and exercise your joints. Arthritis can get worse over time if its not treated. Follow the instructions your provider or physical therapist give you. Talk to your provider about any changes in your symptoms, especially if they get worse.
What Questions Should I Ask My Healthcare Provider About Arthritis Of The Knee

It might be helpful to arrive at your healthcare providers office with a list of questions you want or need to be answered. Consider:
- Do I have arthritis in one knee or both?
- What type of arthritis do I have?
- Whats a possible cause of my arthritis?
- What treatments do you recommend?
- What medications should I take?
- Do I need physical therapy?
A note from Cleveland Clinic
Knee arthritis can affect people of all ages. Its painful, impairs movement and causes swelling of the joint. Some people are so disabled by it that they cant work anymore. Others can only work after surgery. Meanwhile, for others, the pain isnt necessarily as bad, but it still prevents them from regular activities like cleaning, gardening and running after their kids.
Arthritis of the knee can decrease your quality of life. The good news is that treatments can lessen the severity of your symptoms. The pain and swelling might not be as bad. See your healthcare provider for evaluation and treatment if you have symptoms.
Last reviewed by a Cleveland Clinic medical professional on 10/18/2021.
References
Also Check: How To Diagnose For Rheumatoid Arthritis
Exercise And Other Knee Arthritis Remedies
For both OA and inflammatory knee arthritis patients, exercise is a key component of treatment, particularly if youre overweight or obese
Physical therapy may be a necessary first step for some to strengthen the muscles surrounding your knee joint and improve range of motion. Low-impact exercises walking, cycling, or swimming are usually best for those with arthritis of the knee, but you may be able to do higher-impact exercises if dont have much joint damage.
To help make activity more comfortable, your doctor may recommend using assistive devices such as a cane or a knee brace or sleeve. Wearing well-cushioned, shock-absorbing shoes or inserts is also key unsupportive styles such as flip-flops and flimsy flats only exacerbate knee joint pain. High heels, which throw off your alignment and place added stress on your knees, should also be avoided.
Its also a good idea to talk to your doctor about how to get more rest, since many people with arthritis experience sleep disturbances that studies suggest can lead to pain, depression, and greater disability. Simply practicing good sleep hygiene sticking to a regular bedtime, keeping your bedroom quiet and dark, exercising during the day, etc. can help in many cases.