Psoriatic Arthritis Can Potentially Lead To Permanent Deformity And Disability
4 minute read
When a joint pain or joint tenderness exhibits, it might be solely mistaken for arthritis a common condition that causes pain and inflammation in the joints. In fact, if swollen or tender joints are present with scaly skin patches, psoriatic arthritis might be indicated. If it is left untreated, some patients with psoriatic arthritis can further develop a severe and disabling form of arthritis. Over time, arthritis destroys the small bones, leading to permanent deformity and disability.
Beyond Joints: How Psoriatic Arthritis Affects The Body
This autoimmune, inflammatory disease can reach beyond skin and joints to attack organs and more.
Joint pain is a big part of living with psoriatic arthritis . But the inflammation that affects your joints can cause problems for other organs and tissues, too, and comorbidities, or conditions that often occur with PsA, including obesity and diabetes, bring additional effects not directly related to joints. Youll probably think of skin issues first, but your eyes, heart, lungs, gastrointestinal tract , liver and kidneys may also be affected.
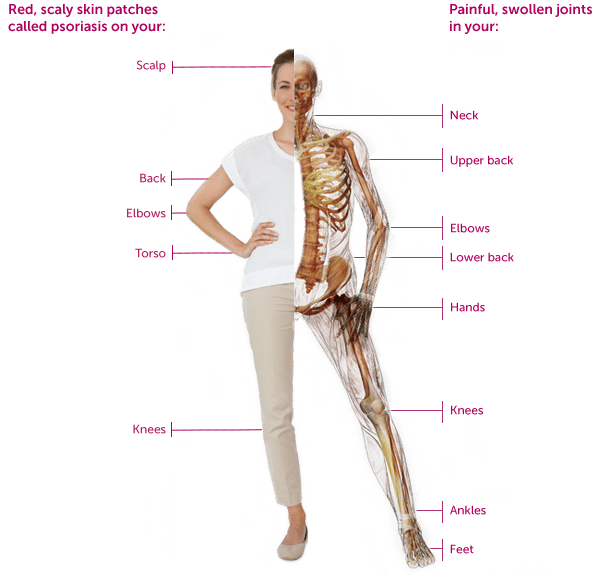
Skin. Psoriasis appears first in 60% to 80% of patients, usually followed within 10 years but sometimes longer by arthritis. Some people are diagnosed with both diseases at the same time, and 10% to 15% have psoriatic arthritis symptoms before psoriasis. Psoriasis creates thick, reddish, inflamed patches of skin, often with silvery-white scales. These patches, which sometimes itch and burn, may appear anywhere on the body, but are most common on the elbows, knees, scalp, back, face, palms and feet. Its considered severe when more than 10% of the body is covered.
Lungs. The inflammation that causes PsA may also harm your lungs, causing a condition known as interstitial lung disease that leads to shortness of breath, coughing and fatigue. This condition occurs less frequently with PsA than with certain other rheumatic diseases, such as rheumatoid arthritis.
Last reviewed 4/21/2021
Treatment For Psoriatic Arthritis
Treatment for psoriatic arthritis aims to:
- relieve symptoms
- slow the condition’s progression
- improve quality of life
This usually involves trying a number of different medicines, some of which can also treat the psoriasis. If possible, you should take 1 medicine to treat both your psoriasis and psoriatic arthritis.
The main medicines used to treat psoriatic arthritis are:
- non-steroidal anti-inflammatory drugs
- biological therapies
You May Like: What Can You Get For Arthritis
Digestive Problems: A Sign Of Inflammatory Bowel Disease
People who have both psoriasis and psoriatic arthritis are at risk for developing IBD, which includes Crohns disease and ulcerative colitis. This is likely because the mutations in the genes of people who have psoriatic arthritis and Crohns disease are similar or it may be related to side effects from treatment.
A 14-year study published in 2020 in the journal Wein Klin Wochenschr found that people living with psoriatic arthritis had a higher risk of IBD compared to the general population. The study also found that psoriasis was associated with 21 out of 23 gastrointestinal diseases, including celiac disease, autoimmune hepatitis, and fatty liver disease.
Symptoms such as abdominal pain and cramping, blood in your stool, and diarrhea could be signs of IBD. If youre experiencing any of these symptoms, talk to your doctor to help you get the best treatment.
What Does Psoriatic Arthritis Look Like On Hands
Stiff, puffy, sausage-like fingers or toes are common, along with joint pain and tenderness. The psoriasis flares and arthritis pain can happen at the same time and in the same place, but not always. You may also notice: Dry, red skin patches with silvery-white scales.
Recommended Reading: What To Do When You Have Arthritis In Your Knee
What Should I Tell My Doctor Before Starting Humira
Tell your doctor about all of your health conditions, including if you:
- Have an infection, are being treated for infection, or have symptoms of an infection
- Get a lot of infections or infections that keep coming back
- Have TB or have been in close contact with someone with TB, or were born in, lived in, or traveled where there is more risk for getting TB
- Live or have lived in an area where there is an increased risk for getting certain kinds of fungal infections, such as histoplasmosis, coccidioidomycosis, or blastomycosis. These infections may happen or become more severe if you use HUMIRA. Ask your doctor if you are unsure if you have lived in these areas
- Have or have had hepatitis B
- Are scheduled for major surgery
- Have or have had cancer
- Have numbness or tingling or a nervous system disease such as multiple sclerosis or Guillain-Barré syndrome
- Have or had heart failure
- Have recently received or are scheduled to receive a vaccine. HUMIRA patients may receive vaccines, except for live vaccines. Children should be brought up to date on all vaccines before starting HUMIRA
- Are allergic to rubber, latex, or any HUMIRA ingredients
- Are pregnant, planning to become pregnant, breastfeeding, or planning to breastfeed
- Have a baby and you were using HUMIRA during your pregnancy. Tell your babys doctor before your baby receives any vaccines
How Do Doctors Diagnose Psoriatic Arthritis
If your doctor or dermatologist suspects you may have psoriatic arthritis, he or she may recommend you see a rheumatologist. These specialists excel at diagnosing autoimmune diseases like PsA. There is no specific test for psoriatic arthritis. Instead, doctors make a diagnosis based on a combination of factors, and by ruling out other conditions.
Your doctor will perform a physical examination to look for symptoms, such as joint pain, stiffness, warmth, swelling, and nail changes. He or she will consider your medical history, including the frequency and progression of your symptoms, as well as any family history of psoriasis or psoriatic arthritis.
You likely will undergo imaging scans to check for joint damage, as well as simple blood tests to rule out diseases with similar symptoms, such as gout and rheumatoid arthritis . The presence of rheumatoid factor in blood test results often indicates RA most patients with psoriatic arthritis are RF-negative.
You May Like: Why Do People Get Rheumatoid Arthritis
Focusing On People With Psoriasis
Most people with psoriatic arthritis have psoriasis first. For a small percentage of patients, psoriatic arthritis occurs before psoriasis, although most often they will have a first-degree relative with skin psoriasis, notes Dr. Haberman. Still, others have no skin psoriasis or dont notice the psoriasis hidden in areas like the scalp, umbilicus, and gluteal fold.
Read more about the connection between psoriasis and PsA.
Up to 30 percent of patients with psoriasis will go on to develop psoriatic arthritis, says Dr. Haberman. The majority of cases begin with the skin condition and then progress to joint pain within seven to 10 years. Recent studies have found that patients with psoriasis who develop severe fatigue, heel pain, and joint pain without overt swelling are more likely to develop PsA.
While we dont yet know which individual patients with psoriasis will go onto develop PsA, researchers have identified a few potential risk factors for the progression of PsA, including:
- Family history of psoriatic arthritis
- Psoriasis that affects the scalp and groin
- Nail involvement in psoriasis, such as nail pitting
- Being overweight or obese. PsA is worse in patients who are overweight and often biologics may not work as effectively in people who are overweight, says Dr. Haberman.
- Exposure to certain infections
- Physical trauma
What Are The Potential Complications Of Psoriatic Arthritis
Left untreated, psoriatic arthritis can permanently damage joints. It also puts you at risk for certain other medical conditions, including type 2 diabetes and cardiovascular disease. Thankfully, there are several medications for psoriatic arthritis that improve joint pain and swelling and reduce the potential for joint damage.
Although some psoriatic arthritis medicines have side effects, your doctor will tailor the dose to your specific symptoms and intensity of the disease. In this way, you are not taking more medicine than you need for symptom relief and good quality of life. Still, discuss the risks and benefits of any psoriatic arthritis treatment with your doctor. Some people experience few or no medication side effects, and others experience very mild complications that pass. Your doctor will work with you to develop a treatment plan with the fewest risks and highest benefits.
Don’t Miss: What Can I Do For Arthritis In My Shoulder
How Lifestyle Changes Help
In addition to drugs that slow down the march of psoriatic arthritis, you can change your lifestyle to ease the pain, stiffness, and fatigue that come with the disease:
Simplify tasks. Why strain your joints when there are products to make twisting, turning, pushing, and pulling easier? Look for arthritis-friendly products to suit your needs, large and small — from gardening tools to walk-in bathtubs. You can also change the way you do everyday things. For example: Use your body, not your hands, to push open doors lift cookware with two hands instead of one.
Slim down. Losing weight is hard, whether youâre trying to shed 10 or 100 pounds. But achieving a healthy weight can make a difference in your PsA. It lightens the load on your joints, which means less pain, more energy, and better mobility. Plus, being overweight can make some PsA medications less effective.
Master your stress. Like fanning a flame, stress causes your body to release chemicals that aggravate PsA. Consider a therapist or support group for PsA, as well as these proven ways to manage stress:
What Is Psoriatic Arthritis Again
Lets make one thing clear: Psoriatic arthritis and psoriasis are two relatedbut separatesystemic autoimmune conditions, both of which are driven by an out-of-whack inflammatory response. In psoriasis, your skin is the primary target, which leads to those uncomfortable, itchy rashes. In PsA, the immune system mistakenly zeroes in on the joints, ligaments, and tendons, causing joint pain, swelling, and stiffness. If left untreated, PsA can permanently damage the joints, seriously interfering with your ability to move or function normally.
About 30% of people with psoriasis will go on to develop PsA, and while we dont know the exact cause, scientists believe genetic susceptibility, an overactive immune system, and environmental factors all play a role.
Read Also: What Does Turmeric Do For Arthritis
Causes Of Psoriatic Arthritis
Almost 1 in 3 people with psoriasis also have psoriatic arthritis.
It tends to develop 5 to 10 years after psoriasis is diagnosed, although some people may have problems with their joints before they notice any skin-related symptoms.
Like psoriasis, psoriatic arthritis is thought to happen as a result of the immune system mistakenly attacking healthy tissue.
But it’s not clear why some people with psoriasis develop psoriatic arthritis and others do not.
Is Psoriatic Arthritis Considered A Disability
Psoriatic arthritis falls under the classification of immune system impairments of the Disability Evaluation Under Social Security. 2 More specifically, it is listed under section 14.09 titled Inflammatory Arthritis. If someone meets the requirements under section 14.09, they may be approved for disability payments.
Don’t Miss: How To Improve Rheumatoid Arthritis
Early Stages Of Psoriatic Arthritis
Recognizing the signs of psoriatic arthritis can be tricky since symptoms differ from patient to patient. For example, one person can experience psoriasis skin involvement and peripheral arthritis, another may experience axial disease , and someone else could have a combination of all three.
Whats more, especially during early disease, you may confuse your symptoms with other conditions. People can mistake enthesitis, inflammation of the entheses for tennis elbow or dactylitis for an infection, explains Dr. Mikulik.
If you have psoriasis and are having pain in your tendon and musculature and you think maybe Ive been too active lately, that may be the first sign of PsA, says Dr. Haberman. Doctors commonly hear people chalk up their symptoms to overuse, such as getting more exercise than usual or doing work around the house.
If you experience any of the following signs of early psoriatic arthritis its important to see your doctor as soon as possible:
- Changes in your fingernails or toenails, including holes, pitting, discoloration, or softness
- Eye inflammation
- Sausage-like swelling of an entire finger or toe
- Scalp psoriasis
- Tendon or ligament pain at the Achilles tendon, bottom of the foot , or elbow
Is Rheumatoid Arthritis Worse Than Psoriatic Arthritis
Even so, the pain and discomfort associated with psoriatic arthritis can be significant. A study published in 2015 in the journal PLoS One found that the overall pain, joint pain, and fatigue reported by psoriatic arthritis patients was significantly greater than that reported by people with rheumatoid arthritis.
Recommended Reading: How To Fix Hip Arthritis
Treatments For Your Skin
If your psoriasis is affecting your quality of life, or your treatment is not working, you may be referred to a dermatologist.
There are a number of treatment options for psoriasis.
Ointments, creams, and gels that can be applied to the skin include:
- ointments made from a medicine called dithranol
- steroid-based creams and lotions
- vitamin D-like ointments such ascalcipotriol and tacalcitol
- vitamin A-like gels such astazarotene
- tar-based ointments.
For more information about the benefits and disadvantages of any of these talk to your GP, dermatologist, or pharmacist.
If the creams and ointments dont help, your doctor may suggest light therapy, also known as phototherapy. This involves being exposed to short spells of strong ultraviolet light in hospital.
Once this treatment has started, youll need to have it regularly and stick to the appointments youve been given, for it to be successful. This treatment is not suitable for people at high risk of skin cancer or for children. For some people, this treatment can make their psoriasis worse.
Retinoid tablets, such as acitretin, are made from substances related to vitamin A. These can be useful if your psoriasis isnt responding to other treatments. However, they can cause dry skin and you may not be able to take them if you have diabetes.
Some DMARDs used for psoriatic arthritis will also help with psoriasis.
Who Is At Risk For Psoriatic Arthritis
Psoriasis affects 2-3 percent of the population or approximately 7 million people in the U.S. and up to 30% of these people can develop psoriatic arthritis. Psoriatic arthritis occurs most commonly in adults between the ages of 35 and 55 however, it can develop at any age. Psoriatic arthritis affects men and women equally.
It is possible to develop psoriatic arthritis with only a family history of psoriasis and while less common, psoriatic arthritis can occur before psoriasis appears. Children of parents with psoriasis are three times more likely to have psoriasis and are at greater risk for developing psoriatic arthritis. The most typical age of juvenile onset is 9-11 years of age.
Recommended Reading: Is Arnica Cream Good For Arthritis
How Do Doctors Treat Psoriatic Arthritis
There is no cure for psoriatic arthritis. However, you can certainly expect to reduce the severity of its signs and symptoms. It is ideal to consult with a rheumatologist who is a doctor who specializes in treating the condition of the bones, joints, ligaments and tendons affected by the immune system. By looking at your medical history and existing signs and symptoms, the rheumatologist will design a customized plan that involves
Medications used for treating inflammation in psoriatic arthritis and psoriasis can also help stave off other anti-inflammatory conditions such as hyperlipidemia , heart disease and diabetes.
There may be an initial trial-and-error period when beginning treatment for psoriatic arthritis. With effective treatments, you can likely expect a major improvement in your joint pain and swelling within a year. Evidence suggests that nearly six out of 10 people with psoriatic arthritis can attain remission after taking biologic drugs for a year.
As advised by your doctor, remember to continue taking the drugs despite a dramatic relief in symptoms. A disease-free period does not mean that psoriatic arthritis is cured. Stopping treatment can lead to a recurrence of the previous signs and symptoms within a few months.
Orthotic devices such as braces and splints can help you manage your daily activities with comfort and ease.
Massage, occupational therapy and physiotherapy can help relieve pain and stiffness and help restore joint mobility.
How Do You Reverse Psoriatic Arthritis
While theres no way to reverse or cure psoriatic arthritis, there are several things you can do to slow its development. These tend to work best when started earlier rather than later. You may want to consider seeing a rheumatologist as well. This is a type of doctor that focuses on autoimmune conditions.
Read Also: How Do I Know If I Have Knee Arthritis
What Causes Psoriatic Arthritis
The genes you inherit from your parents and grandparents can make you more likely to develop psoriatic arthritis. If you have genes that put you at risk of this condition, the following may then trigger it:
- being overweight
There is also an element of chance, and it might not be possible to say for certain what caused your condition.
Psoriasis and psoriatic arthritis are not contagious, so people cant catch it from one another.
What Does Psoriatic Arthritis Back Pain Feel Like

Back pain from psoriatic arthritis can feel like an aching pain and increased pressure in your back from joint stiffness and inflammation that develops. Where does your back hurt with psoriatic arthritis? Psoriatic arthritis can occur anywhere along the spine, but is most common in the lumbar spine, or low back.
Don’t Miss: Can You Have Arthritis In Your Legs
Effects On The Digestive System
There is a link between inflammatory bowel disease , such as Crohns disease, and PsA because inflammation underlies both conditions. IBD causes diarrhea and other gastrointestinal symptoms.
People with PsA have a significantly increased risk of developing IBD, according to research from 2017. Other studies suggest that psoriasis is eight times more common in people with Crohns disease.