Heres Why Your Arthritis Is Flaring Up September 17 2017
arthritis, heart health
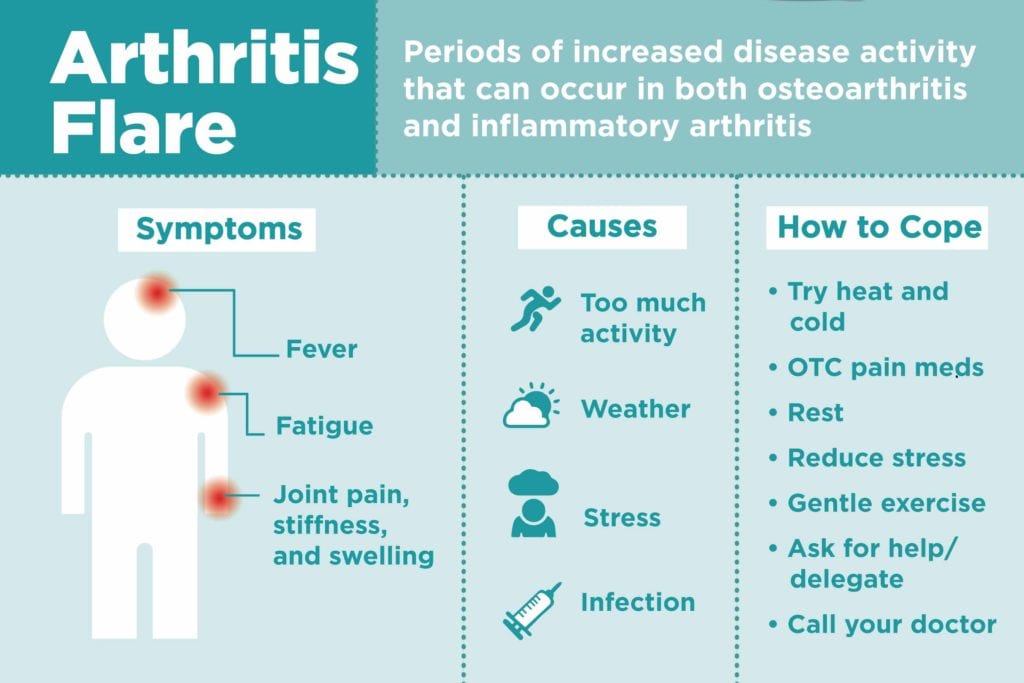
It doesnt always feel like this. Sometimes its a dull ache, other times a sharp pain, and occasionally its unnoticeable. Arthritis is a touchy condition, and its nearly impossible to pin down when it will flare up. However, many people will find themselves hurting a little more than normal as the weather begins to cool. Today, were going to discuss what it means for arthritis to be flaring up, possible causes, and treatments.
If you find yourself questioning why your arthritis is flaring up, you are not alone. According to the Arthritis Foundation, 40 million American adults suffer from arthritis, and they expect another 38 million diagnoses by 2040. As a matter of fact, the Arthritis Foundation also reports that arthritis is the number one disability facing Americans today. It affects 1 in every 5 adults, 1 in every 250 children, and causes $156 billion in loss every year. With that knowledge, its easy to see that arthritis is an important condition to understand.
What does Flaring up actually mean?
To understand what flaring up is, we need to understand the science behind arthritis. Arthritis itself is not actually a disease, but instead a group of joint disorders. There are over 100 types of arthritis, the most common of which is osteoarthritis. The Arthritis Foundation notes that osteoarthritis occurs:
What causes osteoarthritis flares?
How can I treat an arthritis flare?
Red And Processed Meats
Many meat products are produced by adding preservatives, artificial ingredients, hormones, and other additives. These are chemical ingredients that are foreign to the human body and can cause adverse and systemic inflammatory reactions in some people and in particular those people with RA.
Avoid processed meats like deli meats, bacon, and pepperoni which have been altered and cooked with hydrogenated oils and contain saturated or trans fats. Instead, choose lean cuts of meat that are labeled organic and grass-fed as opposed to grain-fed. Try to reduce your intake of red meat by swapping it for fish instead.
Just When You Thought Your Back Was Safe From Rheumatoid Arthritis An Ra Flare Up Strikes Your Spine Learn How To Manage And Prevent Ra Flare Ups
Managing your rheumatoid arthritis is an ongoing balancing act. Youve had your share of painful symptoms, and your rheumatologist has prescribed medication that should help you handle them. Youre also doing your best to follow your doctors lifestyle instructions, even though you may have hit a few bumps in the road. Overall, you think youre on a good path.
Learn how to manage RA flare ups in your spinal joints.
And then, you wake up one morning and you can barely get out of bed. Your joints feel swollen and stiff, and its a challenge to even get through your morning routine. Youre likely experiencing a rheumatoid arthritis flare up, and youre certainly not alone. Even people with well-controlled RA symptoms can be surprised by sudden flare ups.
Learning how to manage your RA flare ups will help you to better manage your overall health. By monitoring your daily activities, you can also minimize your chances of experiencing these uncomfortable episodes.
Also Check: How Does Methotrexate Help Rheumatoid Arthritis
Symptoms Of An Arthritis Flare
There are some arthritis flare symptoms found in every type of arthritis, like extreme joint pain and stiffness. Morning joint stiffness is a common symptom for rheumatoid arthritis, osteoarthritis and psoriatic arthritis. However, each type of arthritis also has symptoms unique to the particular arthritis. For example, rheumatoid arthritis is symmetric, meaning it usually affects both sides of the body, like both hands, both knees and/or both feet. Following are some of the typical symptoms of each type of arthritis.
Rheumatoid arthritis joint pain and swelling joint is warm to the touch joint stiffness fatigue joint redness loss of appetite low-grade fever limited range of joint motion symmetrical joint effect.
Osteoarthritis joint pain and stiffness joint swelling can occur but is not as common as it is in people with rheumatoid arthritis fatigue, often induced by pain experienced during the night that keeps a person awake may affect a joint on one side of the body, like one knee or one ankle.
Psoriatic arthritis joint pain, swelling and stiffness joint is warm to the touch most likely to cause foot pain where ligaments and tendons attach to the bones, swollen fingers and toes and/or lower back pain .
Gout develops quickly and joint becomes very painful joint swelling, warmth, reddish discoloration tenderness.
Signs Of A Rheumatoid Arthritis Flare

Whats more, people with rheumatoid arthritis have different receptors on their immune cells MHC receptors which are more likely to bind to self-proteins, explains Ashira Blazer, MD, a rheumatologist at New York University’s Langone Medical Center in New York City. Environmental triggers can aggravate the immune system and cause these proteins to end up in the joint space, which can lead to inflammation and damage. Also, during a flare, antigens make their way into the joints, and when immune cells in the joints become activated, the linings of the joints become inflamed. The result: Red, hot, tender, swollen joints signs of a flare.
Also Check: Does Walking Help Knee Arthritis
What Is The Treatment For Rheumatoid Arthritis Rashes
The treatment for a rheumatoid arthritis-related rash depends on its cause and severity. A treatment that works well for one type of rash may be useless for another. Treatment usually focuses on managing pain and discomfort, and preventing an infection. Its also important that treatments target the underlying condition, since rashes may be a sign that your rheumatoid arthritis isnt well-controlled.
Common over-the-counter medications that may reduce the pain of a rash include acetaminophen and nonsteroidal anti-inflammatory drugs . There are several types of NSAIDs, such as ibuprofen , naproxen sodium , and aspirin .
If your pain is severe, your doctor may also consider prescription NSAIDs. Opioid pain drugs are usually only prescribed for very severe pain since they have a high risk of addiction.
Your physician may also prescribe corticosteroids to reduce the inflammation of your rash, which may in turn reduce painful symptoms. However, these drugs arent recommended for long-term use. If your doctor is concerned that your rash could get infected, theyre likely to prescribe either a topical or oral antibiotic, or both.
When it comes to treating the underlying condition, there are several different medication options available:
Treatments for interstitial granulomatous dermatitis include topical steroids and antibiotics. Doctors may also prescribe etanercept , a medication thats also used to treat psoriasis and psoriatic arthritis.
Monitoring And Discussing Rheumatoid Arthritis Pain
Pain is pretty subjective and variable, says Dr. Schulman. How people perceive and tolerate pain may differ a lot from person to person.
Some patients with little joint tenderness may experience a lot of pain, and some people with really bad inflammatory arthritis dont experience any pain, she notes.
This is why its important to monitor your pain and be open with your rheumatologist about the level of your pain, your personal threshold for pain, and whether the pain seems new or different from your past RA pain. Pain is very tricky for everyone involved, says Dr. Domingues. There is no lab test for pain, so we really need to have a good honest doctor-patient relationship to gauge pain.
Tracking your RA pain can help you better understand your condition. Join ArthritisPower, a patient-centered research registry, to learn more about tracking your RA. .
Having an open dialogue with your doctor can help them identify the causes of your pain whether RA inflammation or a co-occurring condition is the likely culprit and come up with a treatment plan. Treatment is very different for fibromyalgia than for rheumatoid arthritis than for osteoarthritis, notes Dr. Domingues.
What specifically does your rheumatologist want to know about your pain?
Keeping a pain diary can help you clearly communicate the details of your pain to your rheumatologist. Here are some questions to consider when monitoring your pain prior to your next visit whether in-person or telehealth:
Read Also: Is Cabbage Bad For Arthritis
Common Medications To Treat Arthritis Flares
OA patients might just need some OTC pain-relieving medication such as acetaminophen, ibuprofen, or naproxen. Dr. Bose also recommends topical gels and lotions like diclofenac gel or 2 Old Goats. If that doesnt work, Dr. Ashany says joint injections of steroids may be given. RA flares are more complicated. In inflammatory arthritis, steroids are often used to try to quickly bring a flare under control, Dr. Ashany says. If only one joint is involved a steroid can be given by injection, but otherwise it can be taken orally .
In inflammatory arthritis, if flares continue to occur, this indicates that the patients regimen of maintenance medication is not adequate, Dr. Ashany says. This may lead to addition of a medication, switching one drug for another or increasing the dose of medication that the patient is currently taking.
Comprehensive Joint Supplements To Help With An Arthritis Flare
There is not a cure for arthritis. However, there are different medications and supplements that can ease its symptoms. Most treatments aim for remission, where the patient has few or no symptoms. When treatment is preventative or begins early in the disease process, this can help minimize or slow damage to the joints and improve the quality of life for patients. Treatment usually involves a combination of medication, supplements, exercise, rest, and protecting the joints.
An effective joint supplement addresses arthritis symptoms, and may even reduce the occurrence of an arthritis flare-up. Flexcin is a joint supplement that has all-natural and effective ingredients. It is highly reviewed and has a reputation for good manufacturing practices. If you have arthritis and suffer from flare-ups adding a daily joint supplement may be a course of action for you. Flexcin helps many people combat arthritis flare-ups without the harmful side effects of pain medications.
The Flexcin formula contains all-natural ingredients: CM8, Glucosamine Sulfate Potassium, Hydrolyzed Collagen Type II, MSM, Bromelain, Vitamin C, Manganese, Zinc, and an enzyme blend. The combination of these powerful ingredients increases energy, builds up the immune system, and decreases joint pain and inflammation.
Also Check: What Causes Arthritis In The Knee
What Are The Symptoms Of Inflammatory Arthritis
The most common symptoms of inflammatory arthritis are:
- Joint pain and stiffness after periods of rest or inactivity, particularly in the morning
- Swelling, redness and/or a feeling of warmth in the affected joints
- Inflammation of other areas in the body, such as the skin or internal organs like the lungs and heart
People with inflammatory arthritis generally experience alternating periods of “flares” of highly intense symptoms with periods of inactivity.
What Is A Flare
Simply put, flares are episodes of increased disease activity. Because RA is an autoimmune disease, a flare basically means the body is fighting itself more than usual, says Stuart Kaplan, MD, the chief of rheumatology at South Nassau Communities Hospital in Oceanside, New York. Antibody levels may go up, and markers of inflammation go up, too.
Also Check: Does Arthritis Pain Cause Fatigue
Follow Your Doctors Advice
Arthritis flare ups are inevitable, so you need to prepare yourself before they hit you. Always consult your doctor in advance, and make sure you follow the above tips to eventually get rid of the pain.
Hopefully, this article helped you to understand arthritis, its causes, and symptoms and more importantly, you learned how to prevent, treat, and potentially cure arthritis flare ups.
Managing Rheumatoid Arthritis Flares
There are ways to manage rheumatoid arthritis flares. These include:
You May Like: Can You Exercise With Arthritis
Further Breakdown Of The Joint
Osteoarthritis involves a breakdown of joint cartilage. This happens naturally with age, but an injury or another form of physical stress can accelerate the process.
When cartilage breaks down, it causes the bones of the joint to rub together, leading to pain.
As cartilage deteriorates, bone spurs can start to appear. Known as osteophytes, these are small bony protrusions that can irritate the joint and worsen pain.
What Causes Bursitis To Flare Up
Complementary and Alternative Therapies. Alternative therapies may help reduce the pain and inflammation of bursitis. Eat whole grains, fruits, vegetables, and fatty fish to help reduce inflammation. Avoid processed foods and foods high in sugar and fat.
Beside this, What are 5 foods that cause joint pain?
Pasta. Wheat products like pasta, bread, crackers, and bagels may spell trouble for your joints, especially if you have rheumatoid arthritis. Butter and Margarine. These spreads may seem innocent enough, but theyre packed with advanced glycation end products, or AGEs. Hamburgers. Sugary Drinks.
Likewise, What are the 5 worst foods to eat if you have arthritis?
Trans Fats. Trans fats should be avoided since they can trigger or worsen inflammation and are very bad for your cardiovascular health. Gluten. More than just a health trend, there are good reasons to avoid gluten. Refined Carbs & White Sugar. Citrus Fruit.
Also, What vitamin is good for bursitis?
Try glucosamine or omega-3 fatty acids. Glucosamine is a substance found in cartilage. Research has shown that over-the-counter glucosamine supplements may help inflammation in bursitis. Do not take glucosamine if you take a blood-thinning medication, as glucosamine can increase the risk of bleeding.
What happens if you leave bursitis untreated?
Read Also: How To Deal With Arthritis
Causes Of Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disease. This means your immune system attacks the cells that line your joints by mistake, making the joints swollen, stiff and painful.
Over time, this can damage the joints, cartilage and nearby bone.
It’s not clear what triggers this problem with the immune system, although you’re at an increased risk if:
- you are a woman
Find out more about the causes of rheumatoid arthritis.
What Is A Rheumatoid Arthritis Flare Up
A rheumatoid arthritis flare up describes a short-term escalation of your RA symptoms. A flare up can subside within a day or two, or it can persist for several weeks or months.
An RA flare up generally involves joint stiffness and pain, although it can manifest itself as a worsening of any symptom. If the flare up is especially severe, it can affect your ability to perform your everyday activities.
Ai Mukai, MD, a physiatrist with Texas Orthopedics Sports and Rehabilitation in Austin, Texas, emphasizes that RA flare ups are a known part of rheumatoid arthritis and its course and symptoms. Dr. Mukai, who possesses board certifications in pain medicine and physical medicine & rehabilitation, is also a SpineUniverse Editorial Board member.
Don’t Miss: Is Diclofenac Sodium Topical Gel Good For Arthritis
How Long Do Ra Flares Last
The length of time an RA flare lasts can vary widely, from a few hours to several days or weeks. If a flare does not improve after 7 days, it may be a good idea to contact a physician. The doctor may suggest adjusting the persons medication.
Before a RA flare begins, a person may experience fatigue or feel that something is not quite right.
During a flare, symptoms tend to increase until they reach their peak. As the peak passes, the symptoms will lessen and may completely disappear.
The frequency and severity of flares can vary widely between individuals. With treatment, a person may spend months or years in remission, while others may experience flares more frequently.
RA flares can be predictable or unpredictable. A flare will occur when something triggers an increase in disease activity, which means that levels of inflammation go up.
Predictable flares usually occur in response to one or more triggers.
Some flares have no apparent trigger, and a person may be unable to identify why it started. This can make them harder to avoid.
In 2017, a involving 274 people with RA who attended a clinic in Turkey found the following appeared to worsen their symptoms:
- emotional or physical stress
What Is Total Knee Replacement
Total knee arthroplasty comprises a replacement of both the end of the femur bone and a replacement of the top part of the tibia . The procedure also involves placing a plastic spacer between where the cartilage used to be between the femur and the tibia.
In total knee arthroplasty surgery, a surgeon will remove the damaged cartilage and bone, and insert new state-of-the-art metal or plastic joint components to restore normal functioning of the knee.
From 1999 to 2008, total knee replacement procedures in the U.S. more than doubled for the population at large and tripled for people between the ages of 45 to 64. By 2012, surgery for end-stage knee osteoarthritis was performed on almost 660,000 Americans every year.
Also Check: How Do You Pop Your Knee
Read Also: What To Eat To Avoid Rheumatoid Arthritis