Biochemical Markers In Ankylosing Spondylitis
Due to the paucity of information provided by standard clinical and laboratory parameters to guide treatment decisions, several of the biomarkers studied in RA have been analyzed in other inflammatory joint diseases, particularly spondyloarthritis , on the basis that these disorders may share aspects of pathophysiology with RA. There has been particular interest in evaluating biomarkers in AS that reflect disease activity and predict structural progression . For disease activity, CRP and ESR lack the sensitivity seen in RA, as these markers are elevated in only about 50% of ankylosing spondylitis patients . Unlike RA, they also correlate poorly with clinical measures of disease activity, although good correlations have been noted with MRI evidence of inflammation in the spine . In contrast to RA, they do not appear to predict progression of structural damage, although similar to RA, CRP does predict clinical response to anti-TNF therapy .
Biomarkers reflecting cartilage turnover have been analyzed in limited cross-sectional studies of patients with AS. Elevated levels of CPII and the aggrecan 846 epitope were observed, as they were in RA , and normalization was seen with anti-TNF therapy . One study has shown that urinary CTX-II may predict progression of structural damage in AS, as also documented for RA . However, unlike RA, the collagen II degradation markers C2C and C1-2C were not elevated.
Background And Advantages Over Existing Technology
Early diagnosis and treatment of rheumatoid arthritis is important in preventing long-term damage and disability. RA should be suspected largely on the basis of clinical findings, such as persistent joint pain, swelling, and stiffness. Further investigations, particularly in primary care, may contribute to the diagnosis. Rheumatoid factor is an autoantibody associated with RA and its presence has traditionally been used to support the diagnosis. However, RF has a low specificity in primary care and cannot be used to rule in or rule out disease. In contrast, anti-citrullinated peptide antibody has emerged as an alternative serological test, as it has greater specificity and may be preferable to RF in the diagnosis of RA. However, it is not yet generally available in primary care.
What Do Rheumatoid Factor Test Results Mean
Testing positive for rheumatoid does not necessarily mean the patient has rheumatoid arthritis. A positive for rheumatoid factor test results means that it can lead to or is the cause of inflammatory symptoms from an autoimmune disorder.
In certain cases, however, patients may test positive for rheumatoid factor, yet remain healthy and never experience any obvious symptoms.
Rheumatoid factor can be present in patients several months or even years before clinical rheumatoid arthritis symptoms develop. Depending on the level of symptoms a patient exhibits, the rheumatoid factor test results can assist doctors in reaching a rheumatoid arthritis diagnosis.
Positive rheumatoid factor results in someone who has been clinically diagnosed with rheumatoid arthritis may also indicate the potential for a more aggressive disease course. This is possible in both children and adult patients.
Patients who test negative for rheumatoid factor but still exhibit symptoms and meet other diagnostic criteria may still be diagnosed with rheumatoid arthritis.
Recommended Reading: How To Relieve Arthritis Pain In Thumb
Offgel Fractionation And Lc
The serum proteins in each sample were separated into 12 fractions through pH310 isoelectric points, using the OFFGEL fractionator according to the manufacturers instructions. Twelve fractions were loaded onto an Eksigent nanoLC 400 system and the cHiPLC® and analyzed, and the proteins were identified using a TripleTOF 5600 mass spectrometer . Thereafter, for relative analysis, SWATH acquisition was conducted. In each run, 100g/mL of samples was injected onto an Eksigent ChromXP nanoLC trap column at a flow rate of 5000nL/min. Samples were eluted from the Eksigent ChromXP nanoLC column at a flow rate of 300nL/min for 120min, and mobile phase B buffer was added gradually into the column over a 120-min total run time. The gradient of mobile phase B buffer was 0min/mobile phase B 5%, 10.5min/40%, 105.5min/90%, 111.5min/90%, 112min/5%, and 120min/5%. Mobile phase B and A buffer, and the search parameters are as described .
Synovial Fluid And Serum Concentrations Of Inflammatory Markers In Rheumatoid Arthritis Psoriatic Arthritis And Osteoarthitis: A Systematic Review
, Departments of Life, Health and Environmental Sciences, University of L’Aquila, L’Aquila, Italy, Departments of Life, Health and Environmental Sciences, University of L’Aquila, L’Aquila, Italy, Departments of Life, Health and Environmental Sciences, University of L’Aquila, L’Aquila, ItalyRheumatology Clinic, Department of Clinical and Molecular Sciences, Marche Polytechnic University, Ancona, Italy
Affiliation:
Journal Name: Current Rheumatology Reviews
Volume 13 , Issue 3 , 2017
Graphical Abstract:
Abstract:
Background: The aim of this review is to investigate systematically the presence of themost extensively studied Synovial Fluid and/or serum markers in patients with RheumatoidArthritis , Psoriatic Arthritis and Osteoarthritis , and their associations andcorrelations with laboratory and clinical data, with a view to providing insights for future research.
Method: Considering the sample size of the studies reviewed here, their findings need confirmation inlarger samples, while the potential prognostic value of SF and/or serum biomarkers requires prospectiveinvestigation.
Current Rheumatology Reviews
Title:Synovial Fluid and Serum Concentrations of Inflammatory Markers in Rheumatoid Arthritis, Psoriatic Arthritis and Osteoarthitis: A Systematic Review
VOLUME: 13ISSUE: 3
Emma Altobelli*, Paolo Matteo Angeletti, Domenico Piccolo and Rossella De Angelis
Keywords:Synovial fluid, , psoriatic arthritis, inflammation, systematic review, RA patients.
Don’t Miss: Why Does Psoriatic Arthritis Hurt So Bad
Human Leukocyte Antigen Tissue Typing
This test checks for a genetic marker called human leukocyte antigen .
Some studies suggest that around 60% of RA cases may be inherited. If a person has specific antigens, it could mean that they have a higher likelihood of developing RA. However, other factors, such as tobacco use, can also trigger the condition.
HLA markers in the blood can help indicate the likelihood of developing an immune-related condition such as RA. These markers may also be a sign of another condition, such as ankylosing spondylitis or reactive arthritis.
New Symptoms May Change The Diagnosis
Eventually, people with seronegative disease may be diagnosed with a different disease altogether, according to the Arthritis Foundation. If, say, a person diagnosed with seronegative RA develops a skin rash, her diagnosis might change to psoriatic arthritis. Other changes or new test results could lead to a new diagnosis of chronic gout or osteoarthritis. The most important thing at the time you see a rheumatologist is determining whether you have inflammatory arthritis or mechanical arthritis, where there is less that can be done to treat it, says Domingues.
You May Like: Is Red Meat Bad For Rheumatoid Arthritis
People With Seronegative Ra Often Have Different Symptoms
The conventional wisdom is that seropositive patients have more severe symptoms, but recent studies suggest that the difference between the two forms of the disease may have more to do with the joints affected than with the severity of the RA symptoms. And a report published in June 2016 in BMC Musculoskeletal Disorders found that further research is needed to better understand the long-term outcomes of patients with seronegative RA. My experience has been that while the symptoms are similar, seronegative patients are more difficult to treat, says Vinicius Domingues, MD, a rheumatologist in Daytona Beach, Florida, and a medical adviser to CreakyJoints.
How Rheumatoid Factor Affects Prognosis
Determining a prognosis for rheumatoid arthritis patients can be a complicated process. The disease affects different people in different ways. A prognosis can depend largely on the type and severity of symptoms the patient displays, as well as their medical history.
Many doctors and researchers feel that a positive rheumatoid factor test result may predict a more severe pattern of symptoms and overall disease course. Extra-articular symptoms like rheumatoid nodules may be more likely to form in patients who have positive rheumatoid factor blood test results. Other aggressive symptoms, though rare, could be more likely to occur in rheumatoid factor positive patients. These may include symptoms due to an autoimmune effect on the lung and heart.
Rheumatoid factor-positive patients may also have a higher disease activity score, meaning frequent flare-ups and fewer remission periods.
Keep in mind this isnt always the case. If rheumatoid factor is tested and symptoms are detected early, a diagnosis can be quickly reached. Early diagnosis means treatment can begin sooner, hence preventing further progression of joint damage, swelling and pain.
You May Like: How To Prevent Arthritis In Knees
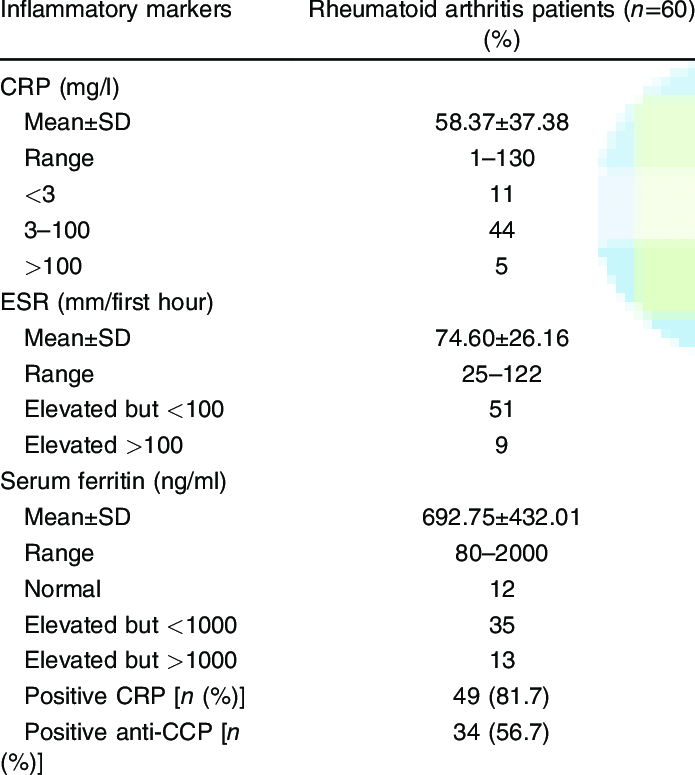
Crp Levels And The Diagnosis Of Rheumatoid Arthritis
No single test can confirm that you have RA. However, measuring levels of CRP in your blood can be part of a comprehensive diagnosis. A doctor can use your CRP levels to track the degree of inflammation over time.
If youre getting tested for RA, the doctor will likely order a standard CRP test rather than an hsCRP test.
To confirm a diagnosis of RA, the doctor will:
- analyze results from other lab tests, such as the rheumatoid factor antibody test and cyclic citrullinated peptide antibody test
- assess levels of morning stiffness and the amount of swelling and pain in your joints
- document the duration of your symptoms
- examine X-rays of the hands and feet to check for erosions or bone damage
Seronegative Ra May Not Be The Correct Diagnosis
According to Cush and Domingues, a small percentage of people with the seronegative form of RA will do very well on therapy and go into remission, and others will experience severe disease and require medication. And still others will not respond to conventional treatment, which may be because they dont have RA at all. Spondyloarthritis conditions, which often affect the spine, are sometimes mistaken for seronegative rheumatoid arthritis.
Read Also: What Tests Are Done For Rheumatoid Arthritis
Rheumatoid Factor And Anti
One blood test measures levels of rheumatoid factors in the blood. Rheumatoid factors are proteins that the immune system produces when it attacks health tissue.
About half of all people with rheumatoid arthritis have high levels of rheumatoid factors in their blood when the disease starts, but about 1 in 20 people without rheumatoid arthritis also test positive.
A related blood test known as anti-cyclic citrullinated peptide test is also available. Anti-CCPs are antibodies also produced by the immune system.
People who test positive for anti-CCP are very likely to develop rheumatoid arthritis, but not everybody with rheumatoid arthritis has this antibody.
Those who test positive for both rheumatoid factor and anti-CCP may be more likely to have severe rheumatoid arthritis requiring higher levels of treatment.
Comparison Of The Clinical Performance
All three ACPA assays showed good discrimination between RA patients and controls, with AUC of 0.82, 0.83, and 0.82, respectively. At the cutoff values provided by the manufacturer, the CCP2 ELISA showed a high sensitivity and a moderately high specificity with a corresponding OR of 16.3 . The two CCP3 assays showed lower sensitivities , but significantly higher specificities , resulting in much higher predictive values, with OR of 99.3 and 107.5 , respectively. The clinical performance characteristics for all assays are summarized in Table 2.
Table 2. Summary of clinical performance characteristics of the assays used in this study.
When all assays were compared at the same specificity , the sensitivities varied from 27.6% to 68.1% . As results greater than 3× ULN carry more clinical weight for the diagnosis and classification of RA as seen in the 2010 ACR/EULAR classification criteria , the clinical performance at the 3× ULN was also analyzed. At this threshold, the sensitivities ranged from 16.0% to 59.0% and the OR varied from 14.7 to 192.5 .
In the RF IgM and CCP3 IgG negative population based on ELISA , the RF IgA ELISA had an 18.5% sensitivity with 76.9% specificity and an OR of 0.8 and the RF IgG ELISA reported a 10.6% sensitivity, an 88.0% specificity and OR of 0.9 . In the RF IgM and CCP3 IgG seronegative population defined by CIA , the RF IgA showed a 5.2% sensitivity with a 98.6% specificity and an OR of 4.0 .
Also Check: Does Rheumatoid Arthritis Affect Your Toes
Should I Take The Test
Genetic testing for rheumatoid arthritis is a good option if you have any type of doubt and want to make sure youre not a susceptible individual. It is especially recommended for patients with a family history of rheumatoid arthritis, and you can either run a test through your doctor or just order a simple genetic test kit to do it at home.
Doing it in the comfort of your own home is convenient and stress-free, and you can confirm your results with your doctor afterwards. Thus, it will be helpful if you have a family member with recently diagnosed rheumatoid arthritis and want to find out if youre carrying the same genetic predisposition.
But even if you dont have any mention of rheumatoid arthritis in your family, performing a test is an excellent option to evaluate your risk and act accordingly. As we mentioned in the previous section, genetic changes in the HLA complex are associated with a myriad of autoimmune diseases, including celiac disease, type 1 diabetes, and myasthenia gravis. Recent studies show theres a crossed risk when it comes to autoimmune diseases in your family.
Additionally, there are environmental factors and other elements increasing the risk of rheumatoid arthritis, and they can be addressed if you detect a genetic predisposition.
In a nutshell, you have nothing to lose by taking a test for genetic markers of rheumatoid arthritis, especially if you have a persistent doubt in your mind about this particular condition.
Seronegative Ra Has Become More Common In Recent Years
According to CreakyJoints, a support, education, advocacy, and research organization for people living with arthritis and rheumatic disease, the majority of rheumatoid arthritis patients are seropositive. But while youre far less likely to be diagnosed with the seronegative type of the disease, those numbers are on the rise, according to a study published in the March 2020 issue of Annals of the Rheumatic Diseases. Between 1985 and 1994, only 12 out of 10,000 people with RA were seronegative. Between 2005 and 2014, that number crept up to 20 out of 10,000.
Also Check: What Do You Do For Arthritis In Your Fingers
What Do Elevated Rheumatoid Arthritis Markers Mean
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
What Are The Risk Factors For Ra
Researchers have studied a number of genetic and environmental factors to determine if they change persons risk of developing RA.
Characteristics that increase risk
- Age. RA can begin at any age, but the likelihood increases with age. The onset of RA is highest among adults in their sixties.
- Sex. New cases of RA are typically two-to-three times higher in women than men.
- Genetics/inherited traits. People born with specific genes are more likely to develop RA. These genes, called HLA class II genotypes, can also make your arthritis worse. The risk of RA may be highest when people with these genes are exposed to environmental factors like smoking or when a person is obese.
- Smoking. Multiple studies show that cigarette smoking increases a persons risk of developing RA and can make the disease worse.
- History of live births. Women who have never given birth may be at greater risk of developing RA.
- Early Life Exposures. Some early life exposures may increase risk of developing RA in adulthood. For example, one study found that children whose mothers smoked had double the risk of developing RA as adults. Children of lower income parents are at increased risk of developing RA as adults.
- Obesity. Being obese can increase the risk of developing RA. Studies examining the role of obesity also found that the more overweight a person was, the higher his or her risk of developing RA became.
Characteristics that can decrease risk
You May Like: What To Do For Arthritis In The Thumb
Can My Doctor Use Imaware Results
Yes. All of our tests are performed by CLIA-certified labs, the gold standard in lab testing quality regulation. Within your results report you will also find detailed information intended for your healthcare professional. They can use this information to interpret your test results clearly. To see an example of this, you can request a sample report at the top of this page.
Laboratory Biomarkers Of Rheumatoid Arthritis
Rheumatoid arthritis is a systemic autoimmune disease that is an important socio-economic health problem. Recent evidence about the immunopathogenesis of this disorder might open new perspectives for a more appropriate laboratory approach. In this review, our attention is focused on the clinical relevance and appropriateness of laboratory biomarkers correlated with early diagnosis, prognosis, evolutive aspects of the disease and therapeutic efficacy.
RA is a multifactorial disease, in which environmental and genetic factors seem to play a role in the susceptibility and evolution of illness . Several studies have shown a close genetic association with antigens of the MHC-II, in particular HLA-DRB1 , and PTPN22 that encodes the lymphoid tyrosine phosphatase , which is a critical negative regulator of signalling through the T cell receptor . It is known that molecular targets of rheumatic autoimmune reaction are proteins that undergo post-translational modification typically associated with inflammation and apoptosis, such as citrullination and keratinization. Self-antigens probably play a role in the chronic evolution of the process, whereas super-antigens may be involved in the onset of illness. Pro-inflammatory substances released by cells from the immune system maintain the inflammatory process and contribute to the chronic damage .
Read Also: Do I Have Arthritis In My Hands
Blood Monocyte Subsets And Selected Cardiovascular Risk Markers In Rheumatoid Arthritis Of Short Duration In Relation To Disease Activity
Ewa Klimek
1Department of Internal Medicine and Gerontology, Jagiellonian University Medical College, University Hospital niadeckich Street 10, 31-531 Cracow, Poland
2Department of Internal and Agricultural Medicine, Jagiellonian University Medical College, J. Dietl Hospital, Skarbowa Street 4, 31-121 Cracow, Poland
3Department of Rheumatology and Balneology, Jagiellonian University Medical College, University Hospital, niadeckich Street 10, 31-531 Cracow, Poland
4Division of Rheumatology, Department of Internal Medicine and Gerontology, Jagiellonian University Medical College, University Hospital, niadeckich Street 10, 31-531 Cracow, Poland
52nd Department of Cardiology, Jagiellonian University Medical College, University Hospital, Kopernika Street 17, 31-501 Cracow, Poland
Abstract
1. Introduction
Due to increased integrin overexpression monocytes adhere to activated endothelium and migrate into the arterial wall, where foam cells arise from monocyte-derived macrophages to form fatty streaks.
To the best of our knowledge, peripheral blood monocytes heterogeneity has not been extensively studied in patients with RA of short duration so far. Therefore, our goal was to evaluate peripheral blood monocyte subpopulations and their functional properties and to assess traditional CV risk factors and signs of subclinical atherosclerosis in patients with RA of short duration in relation to disease activity.
2. Methods
2.1. Study Population
2.2. Study Protocol
2.4. Flow Cytometry