Is There A Cure For Psoriatic Arthritis
There is currently no cure for psoriatic arthritis. Medications may be able to help with painful symptoms and slow or stop the progression of the disease. It is important as a patient to learn how your body responds to psoriatic arthritis, and how to use exercise, medications, and other treatments to manage symptoms. Vitamin D may help with the inflammation associated with psoriasis.
- American Academy of Dermatology: “Psoriatic Arthritis.”
- American College of Rheumatology: “Psoriatic Arthritis.”
Anemia Of Chronic Disease Vs Iron
Chronic inflammatory disease can cause both iron deficiency and anemia of chronic disease.
People who have arthritis, for example, often take a nonsteroidal anti-inflammatory drug as part of their treatment regimen. NSAIDs have been tied to an increased risk of gastrointestinal bleeding.
If bleeding is suspected, it’s important that the source of bleeding is identified.
How To Spot It
Symmetric PsA symptoms are a lot like asymmetric PsA symptoms. Symmetric PsA tends to affect the smaller joints of the feet or hands, though, rather than larger joints like your knees or elbows.
FYI: Symmetrical PsA is sometimes confused with rheumatoid arthritis . A simple blood test can help you know if youre dealing with RA instead.
Recommended Reading: What Can Be Done For Arthritis In The Back
Types Of Psoriasis: Pictures Locations And More
Psoriasis is a common chronic inflammatory skin condition. It can cause red, purple, or grayish patches to develop that are covered in silvery scales. There are numerous types of psoriasis, and knowing which type a person has allows medical professionals to develop a treatment plan. Psoriasis is not contagious.
Psoriasis is a common condition that affects over 8 million people in the United States.
There are a number of types of psoriasis, and they often have similar triggers. These triggers can include:
- skin injuries, such as scratches, sunburns, bug bites, and vaccinations
- certain medications, including beta-blockers, antimalarials, and lithium
- illnesses, such as ear infections, bronchitis, tonsillitis, and respiratory infections
- cold weather
This article will discuss different types of psoriasis. For each one, it will list symptoms, locations, and treatment options.
Plaque psoriasis is the most common type of psoriasis.
Deterrence And Patient Education
Patients should be extensively educated and counseled with regards to the chronic nature of psoriatic arthritis and the importance of non-pharmacological measures, including exercise, smoking cessation, weight loss, physical therapy, and occupational therapy. They should be made aware of the fluctuating nature of this disease, requiring very close monitoring by the multi-disciplinary treatment team. The side effects related to immunosuppressive medications require a detailed explanation, and an attempt should be made to educate the patient family as well.
You May Like: Can You Get Rheumatoid Arthritis In Your Back
Clinical Features Of Psa In Observational Cohorts And Clinical Trials
Since PsA presents in different patterns, how do patients included in longitudinal observational cohorts compare with those included in drug trials? Some of the drug trials have included patients with five or more swollen joints, whereas others have included patients with three or more swollen joints. Table 2 presents a comparison of the clinical features noted among patients followed prospectively in a longitudinal clinic with those reported in recent drug trials. Generally, the ages at onset and presentation are similar and sex distribution and the numbers of tender and swollen joints are similar in the longitudinal cohort and the drug trials.
Comparison of features from longitudinal clinic data and drug trials of psoriatic arthritis
Enhancing Healthcare Team Outcomes
Patients with psoriatic arthritis have a heterogeneous clinical presentation with the involvement of various domains and are best managed with an interprofessional approach to the treatment of articular disease, skin disease, other manifestations, and medical comorbidities. Patient education is vital to ensure that the symptoms are under control. The physical therapist should encourage exercises to restore joint function. The pharmacist should educate the patient on different medications, their benefits, and adverse reactions, as well as monitoring agent selection, dosing, and checking for potential drug-drug interactions. Nurses should educate patients on the importance of abstaining from alcohol and discontinuing tobacco, answer questions, and help monitor treatment progress. The dietitian should encourage a healthy diet and weight. A mental health nurse and psychiatrist should be involved, as many patients do develop severe anxiety and depression. Patients should be encouraged to seek stress relief. The social worker should assess the home to ensure it can accommodate the patient’s lifestyle. All of these various disciplines need to chart and share their perspectives with the rest of the team so that all members of the healthcare team are operating from the same information base.
Also Check: Can You Get Arthritis In Your Head
Diagnostic Tests/lab Tests/lab Values
- There is no definitive test. Diagnosis is made by ruling out other conditions.
- X-rays are the current gold standard. However, signs of psoriatic arthritis often do not appear on radiographs until later stages of the disease when bone erosion has occured.
- Contrast enhanced ultra sound is starting to play a leading role since it can detect changes in bone and soft tissue much sooner than X-rays.
- Early studies have demonstrated that ultrasound and MRI are both highly sensitive to early inflammatory joint changes that occur in psoriatic arthritis.
- DIP erosive changes on X-rays may support the diagnosis.
- Blood work will be done to detect for the HLA-B27 since it is a common histocompatibility complex marker in people with psoriatic arthritis.
- A blood test for rheumatoid factor should be done to rule out rheumatoid arthritis.
- A blood test for antinuclear antibody should be done to rule out Lupus.
- CBC should be done to check for a reduction in red blood cells that sometimes occurs in psoriatic arthritis.
- A joint aspiration may be done in which a syringe removes fluid from a joint. The fluid is then examined for the presence of infection, crystals, and white blood cells.
Why Is Psoriatic Arthritis Classified By Both Domains And Types
In addition to the older classification systems involving the five types of psoriatic arthritis, treatment and classification guidelines for the disease now categorize the disease by domains too. These have been developed to better diagnose and treat people and allow healthcare providers to better describe how the disease manifests itself in different people.
Also Check: Why Is My Arthritis Acting Up
What Are The Treatment Options For Psoriatic Arthritis
The aim of treatment for psoriatic arthritis is to control the disease and relieve symptoms. Treatment may include any combination of the following:
- Splinting.
- Surgery.
Choice of medications depends on disease severity, number of joints involved, and associated skin symptoms. During the early stages of the disease, mild inflammation may respond to nonsteroidal anti-inflammatory drugs . Cortisone injections may be used to treat ongoing inflammation in a single joint. Oral steroids, if used to treat a psoriatic arthritis flare, can temporarily worsen psoriasis. Long-term use of oral steroids should be avoided when possible due to the negative effects on the body over time.
DMARDs are used when NSAIDs fail to work and for patients with persistent and/or erosive disease. DMARDs that are effective in treating psoriatic arthritis include: methotrexate, sulfasalazine, and cyclosporine.
Biologic agents are an important consideration when disease control is not being achieved with NSAIDS or DMARDs. Biologics have been utilized for the treatment of psoriatic arthritis since 2005 and are highly effective at slowing and preventing progression of joint damage. Your healthcare provider will complete additional laboratory tests and review safety considerations before initiating a medication regimen. Gaining good control of psoriatic arthritis and psoriasis is important to avoid increased systemic risks, particularly heart disease.
Exercise
Heat and cold therapy
Splinting
Surgery
How Is Psoriatic Arthritis Diagnosed
There is no single test to diagnose psoriatic arthritis. Healthcare providers make the diagnosis based on a patient’s medical history, physical exam, blood tests, and X-rays of the affected joints. Magnetic resonance imaging is generally not needed except in unusual circumstances.
Laboratory tests that may be helpful in diagnosis or used to monitor disease activity include:
- Rheumatoid factor and anti-CCP – types of blood tests to help diagnose rheumatoid arthritis.
- HLA-B27 – blood test to help diagnose, may also be indicated with a family history of psoriasis or psoriatic arthritis.
- Sedimentation rate and C-reactive protein – may indicate inflammation.
X-rays are not usually helpful in making a diagnosis in the early stages of the disease. In the later stages, X-rays may show changes that are more commonly seen only in psoriatic arthritis. One such finding is called the “pencil-in-cup,” which describes the finding where the end of the bone gets whittled down to a sharp point. This finding indicates more severe inflammatory changes to joints, which may require more aggressive treatment.
Read Also: Signs And Symptoms Of Arthropathy
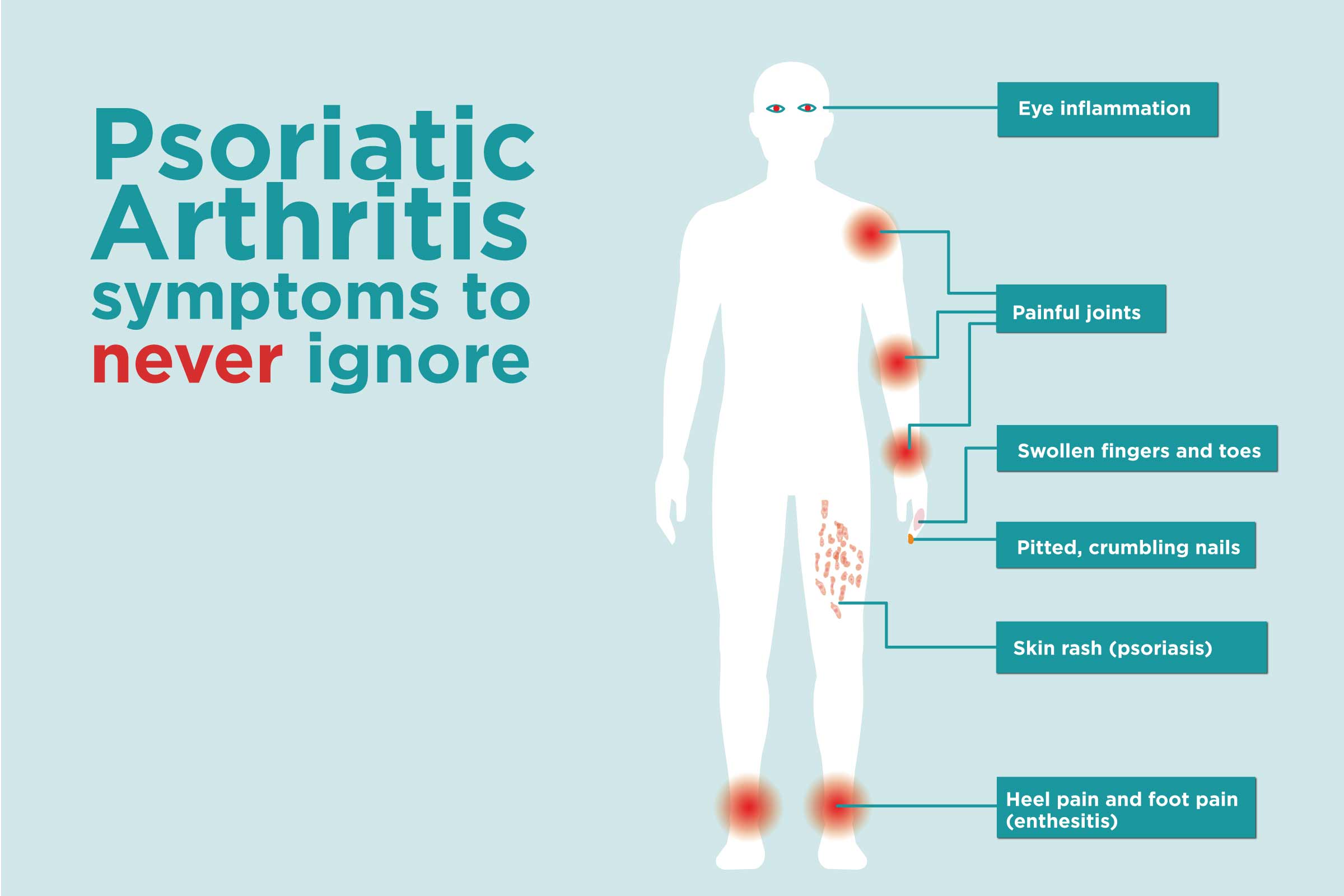
Psoriatic Arthritis Can Affect Any Joint But Certain Patterns Of Symptoms Are More Common Than Others
Psoriasis is a chronic inflammatory skin disorder that can cause a variety of symptoms. The most common type of psoriasis is plaque psoriasis, which manifests as thickened patches of red, scaled skin.
Psoriatic arthritis is a type of arthritis that affects an estimated 30 percent of people who have psoriasis. Psoriatic arthritis causes inflammation in the joints. In addition to being painful and uncomfortable to live with, psoriatic arthritis can cause permanent damage to the joints.
Most people who have psoriatic arthritis have already experienced psoriasis symptoms. However, some people experience symptoms of psoriatic arthritis before experiencing psoriasis symptoms.
Different patterns Psoriatic arthritis can affect any joint in the body, but the disorder tends to affect certain joints in certain patterns. These are sometimes referred to as different types of psoriatic arthritis.
The pattern and progression of psoriatic arthritis can be unpredictable, and the severity of psoriasis skin symptoms do not always correlate with the severity of PsA joint symptoms. A person may have mild psoriasis, but they may have severe psoriatic arthritis. Or a person may have severe psoriasis, but only mild psoriatic arthritis.
Work with a healthcare provider If you have psoriasis, psoriatic arthritis, or both, it is important to work with a healthcare provider.
Articles On Types Of Psoriasis
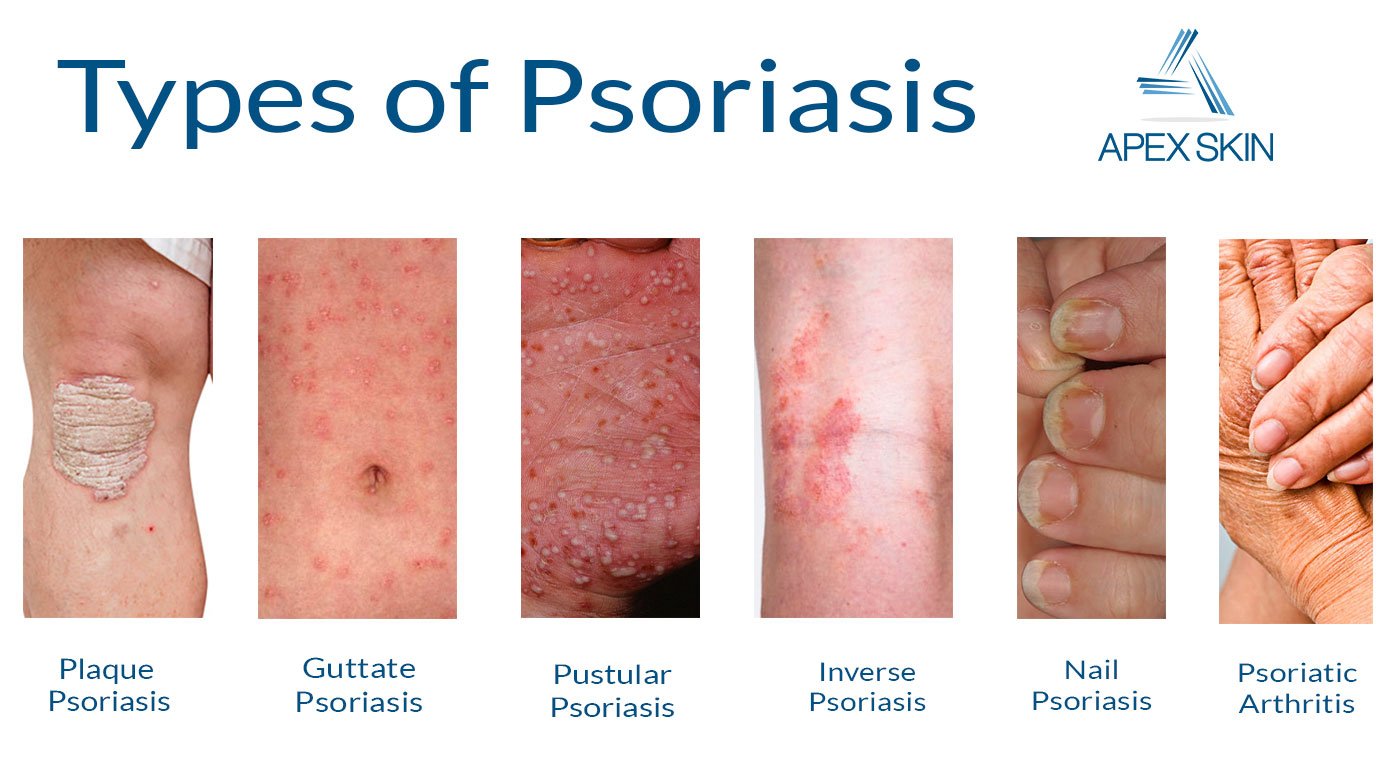
Knowing which kind of psoriasis you have helps you and your doctor make a treatment plan. Most people have only one type at a time. Sometimes, after your symptoms go away, a new form of psoriasis will crop up in response to a trigger.
In general, most types of psoriasis result from the same triggers:
- Diet
- Weather
Here’s how you can spot the 7 types of psoriasis and what you can do to treat them.
Recommended Reading: Stopping Arthritis Pain
When To Get Medical Advice
See a GP if you have persistent pain, swelling or stiffness in your joints even if you have not been diagnosed with psoriasis.
If you’ve been diagnosed with psoriasis, you should have check-ups at least once a year to monitor your condition. Make sure you let the doctor know if you’re experiencing any problems with your joints.
How Will Psoriatic Arthritis Affect Me
Starting the right treatment as soon as possible will give you the best chance of keeping your arthritis under control and minimise damage to your body.
Psoriatic arthritis can vary a great deal between different people. This makes it difficult to offer advice on what you should expect.
It will usually have some effect on your ability to get around and your quality of life, but treatment will reduce the effect it has.
Psoriatic arthritis can cause long-term damage to joints, bones and other tissues in the body, especially if it isnt treated.
Recommended Reading: Rheumatoid Arthritis Skin Rash
The 5 Type Of Psoriatic Arthritis Explained
1. Asymmetric oligoarticular
Asymmetric oligoarticular is one of the most common types of psoriatic arthritis. As the name suggests, this type of the disease affects different joints on either side of the body. While it can affect any joint, it tends to affect less than five joints in a particular person. It produces mild to severe symptoms.
2. Symmetric polyarthritis
Symmetric polyarthritis is another of the most common types of psoriatic arthritis. Unlike the asymmetric oligoarticular type, however, symmetric polyarthritis affects the same joints on each side of the body. It can affect any joints and tends to be found in five or more joints on both sides of the body. It produces mild to severe symptoms.
3. Distal interphalangeal predominant
Distal interphalangeal predominant psoriatic arthritis mainly affects the end of the fingers and toes. Phalanges are the 56 bones that make up the fingers and toes and the distal interphalangeal joints are the joints at the ends of your fingers and toes – the ones closest to the nails.
While nail changes also occur in other types of psoriatic arthritis, they are especially common in people with the distal interphalangeal predominant type of the disease. Nail changes include spotting, pitting and separation of the nail plates from the nail bed .
Distal interphalangeal predominant psoriatic arthritis usually occurs in people who also have other types of the disease, but a small number of people have only this type of psoriatic arthritis.
Causes Of Psoriatic Arthritis
Almost 1 in 3 people with psoriasis also have psoriatic arthritis.
It tends to develop 5 to 10 years after psoriasis is diagnosed, although some people may have problems with their joints before they notice any skin-related symptoms.
Like psoriasis, psoriatic arthritis is thought to happen as a result of the immune system mistakenly attacking healthy tissue.
But it’s not clear why some people with psoriasis develop psoriatic arthritis and others do not.
Recommended Reading: What Works For Arthritis Pain
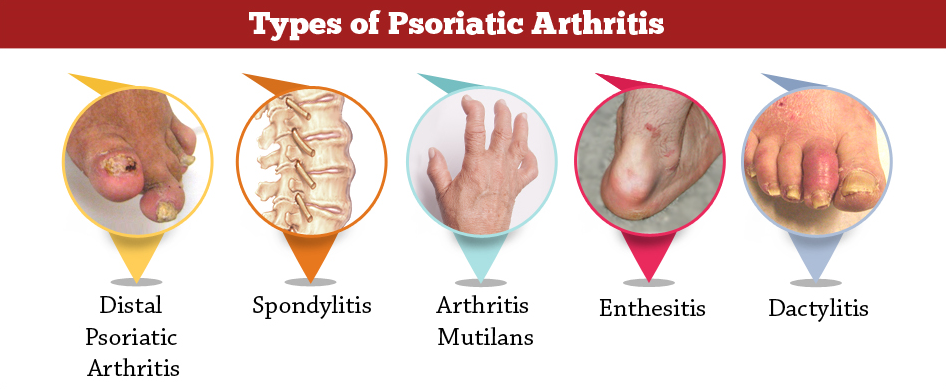
Types Of Psoriatic Arthritis
There are five different types of psoriatic arthritis, determined by which parts of the body are affected as well as the extent and severity of inflammation:
Symmetric arthritis
Symmetric arthritis usually affects the same joints on both sides of the body. Usually multiple pairs of joints, such as the right and left knees or right and left elbows, are affected. This type of psoriatic arthritis resembles rheumatoid arthritis, but its generally milder.
Asymmetric arthritis
Asymmetric arthritis doesnt typically affect the same joints on both sides of the body. Usually, it affects the fingers and toes first, which can lead to an enlarged and sausage-like appearance. Sometimes a larger joint, like the knee, is also affected.
Distal interphalangeal predominant
DIP affects the joints in the fingers and toes closest to the nail nail changes are common.
Spondylitis
Spondylitis refers to inflammation of the spinal column. Many people with psoriatic arthritis will have stiffness in the neck, lower back, or spinal vertebrae, making motion painful and difficult.
Arthritis mutilans
Arthritis mutilans is a severe, deforming, and destructive form of psoriatic arthritis. It usually affects the small joints at the ends of the hands and feet.
What Are The Symptoms Of Psoriasis
There are different types of psoriasis. The most common is chronic plaque psoriasis. This causes patches of red, raised skin, with white and silvery flakes.
It can occur anywhere on the skin, but most commonly at the elbows, knees, back, buttocks and scalp.
Psoriasis can cause small round dents in finger and toe nails, this is known as pitting. Nails can also change colour, become thicker and the nail may lift away from your finger.
Read Also: Is Ra Painful
Five Clinical Presentations Of Psoriatic Arthritis
Diagnosis of psoriatic arthritis may often be delayed since there are no identified biomarkers at this time. If left untreated psoriatic arthritis may lead to severe physical limitations and disability. Early diagnosis is critical to slow the progression of the disease with medications.
The Different Types Of Anemia
There are many different types of anemia, a condition in which there is a low number of red blood cells or a low hemoglobin concentration in the body. Hemoglobin is an iron-rich protein in the RBCs that binds to oxygen, transporting it to tissues throughout the body.
Anemia can develop due to nutritional deficits, blood loss, or chronic diseases. Anemia of chronic disease is a specific type of anemia that’s associated with inflammation. And anemia is common in people with inflammatory types of arthritis, such as rheumatoid arthritis .
The types of anemia can be distinguished from each other with diagnostic tests, such as a complete blood count. And the treatment of anemia is tailored to the type.
Recommended Reading: Edema Rheumatoid Arthritis
Clinical Signs And Symptoms
- Non-steroidal Anti-Inflammatory Drugs
- Local Corticosteroid Injections
NOTE: Neither NSAIDS or intra articular corticosteroids will stop structural joint damage