Risk Of Bias Assessment
The risk of study bias was assessed using the Cochrane Handbook for Systematic Reviews. The risk of bias of the studies was evaluated with regard to the following aspects: random sequence generation, hidden methods utilization, blinding method application, incomplete results management, selective reporting of results, and other biases. Funnel diagrams were used to detect publication bias.
Basics About Vitamins And Minerals
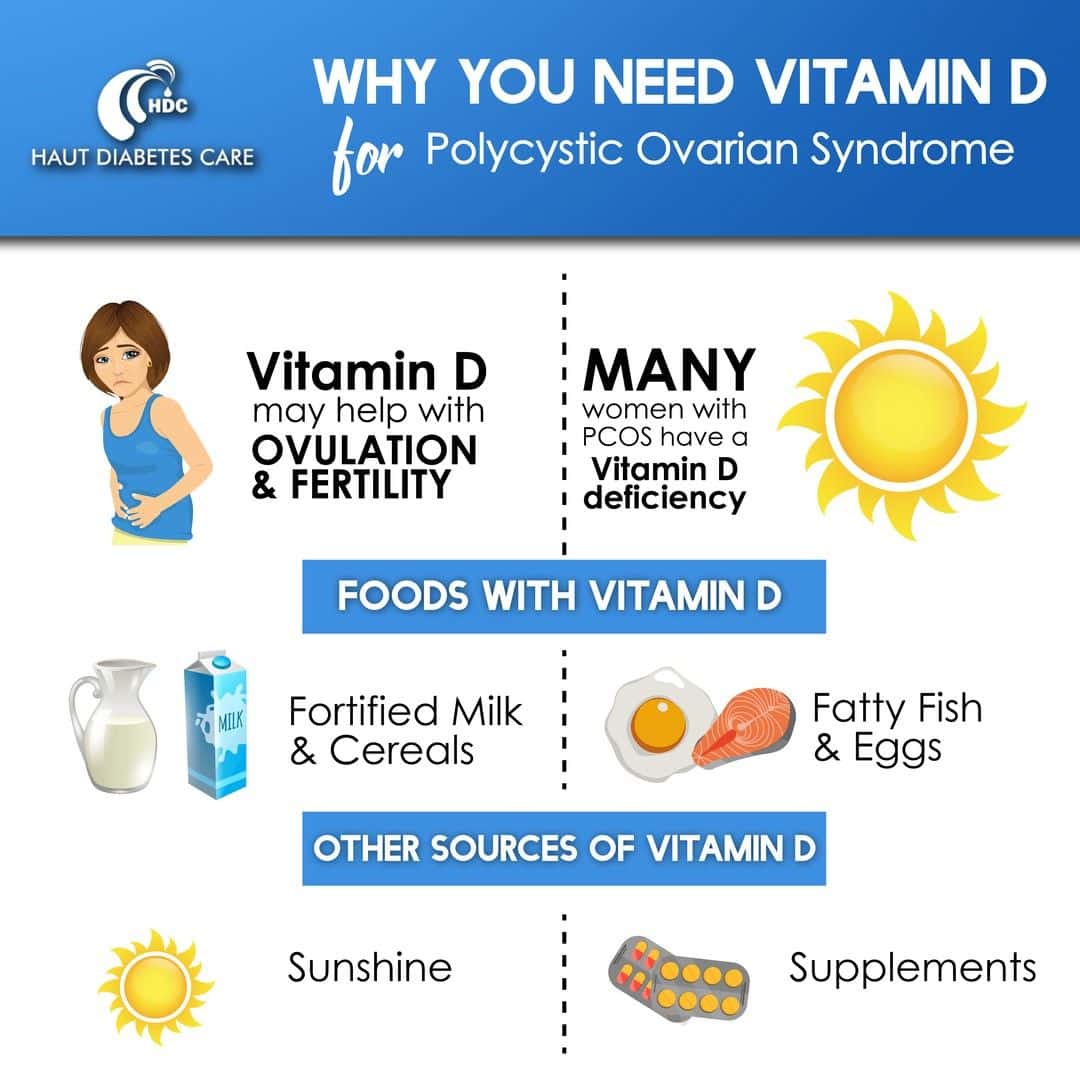
Vitamins are chemicals that our bodies need to maintain health. Except for vitamin D, which is produced in our bodies when were exposed to sun , we typically get our daily requirement of vitamins from dietary sources . Minerals are inorganic substances.
There is general agreement that consuming the recommended daily allowance of basic vitamins and minerals is needed to stay healthy. There is controversy, however, about whether some people should take more than the RDA of certain vitamins and minerals. Getting too much of some vitamins and minerals may be dangerous to general health. This is why it is important to talk to your doctor before you take any vitamin or mineral supplement .
Medication and other forms of treatment play a major role in managing rheumatoid arthritis. Supplements arenât a treatment â they donât promise to cure or treat any condition, and they donât have to meet the same standards as medications. But if youâre looking into trying some in addition to your treatment plan, hereâs what you should know.
First, be sure you talk to your doctor before you begin using any supplement or herbal medication. They may interact with other drugs, supplements, or herbal medicines you are taking and cause serious side effects. They may also put you at a higher risk for certain conditions.
Vitamin D As A Potential Arthritis Treatment
More research is needed to determine the potential of vitamin D as a rheumatoid arthritis treatment, and the exact vitamin D form and dosage required for improving arthritis. High dose oral vitamin D supplements have the potential to cause harm, and therefore it is important to consider what is a safe and appropriate dose.
The Institute of Medicines recommended dietary allowance for vitamin D is 600 International Units per day. This recommendation is based on what is needed to prevent rickets and osteoporosis. Many vitamin D researchers disagree with this recommendation and say that the IOMs recommended allowance isnt enough to prevent deficiency or support bone health. Generally, 4,000 IU or less per day is considered safe, as long as your blood values are being monitored. It is important to avoid excessive doses of oral vitamin D. If vitamin D intake is too high, it can cause elevated blood calcium levels and potentially dangerous consequences.
Obtaining vitamin D from light allows your body to self-regulate vitamin D production and make as much as it needs to stay healthy, without any risk of overdose or toxicity. Unlike with oral supplements, you cannot overdose on vitamin D produced in your skin. If you have enough vitamin D, your body will simply produce less.
Also Check: Is Rice Bad For Arthritis
Q: How Do I Check If My Vitamin D Levels Are Low
Ask your doctor for a simple blood test called a total serum 25-hydroxy vitamin D test, which is generally covered by insurance, says Weijia Yuan, M.D., a rheumatologist at the Hospital for Special Surgery in New York City. While experts disagree on what constitutes a healthy level, the NIH recommends between 20 and 50 ng/mL. Ideally, you should be around 50, says Dr.
Also Check: Does Lidocaine Work For Arthritis
It Is Not Just About The Immune System
The effects of vitamin D on the bones is also beneficial for reducing the onset risk of rheumatoid arthritis. It is also essential to reduce the symptoms and progression of the disease.
Vitamin D helps to strengthen the bones. Most importantly when it comes to RA, the nutrient helps to strengthen the cartilage. It is the cartilage that helps to protect against the development of any arthritis. Cartilage is the bit between the bones that help to prevent the two from rubbing. The joints can move around much smoother and easier. Think of it as the lubricant between rocks. When the lubricant goes, the rocks rub together and start shaving away parts of each other. This is excruciating for the bones.
Cartilage will disappear over time. It is a natural part of aging, but you can help to slow down the process with the right amount of vitamin D and calcium. Even if you do not think vitamin D will help prevent the onset of rheumatoid arthritis, you can protect your joints from wear and tear.
There are also studies that show adequate vitamin D can also prevent the onset of other bone diseases, especially rickets. Children who have spent all the time indoors, especially in countries with little sun, have found issues with rickets and other bone diseases.
Recommended Reading: How To Lessen Arthritis Pain
Are You Getting Enough Vitamin D
Your doctor can order blood tests to determine whether youre getting enough vitamin D, but here are a few more telltale signs of a deficiency:
- Chronic pain or aches that last for weeks, similar to symptoms associated with rheumatoid arthritis
- Melancholy or depressed mood
- Osteoporosis and brittle bones
- Fatigue and weakness that doesnt seem normal
- Excessive sweating, especially on your forehead
Vitamin And Mineral Guide For Arthritis
Learn about key vitamins and minerals and which ones are especially important when you have arthritis.
Vitamins and minerals play a critical role in staying healthy, but getting enough of certain nutrients is even more important when you have arthritis. This guide provides thorough research of key vitamins and minerals to help you figure out what you may be missing. But remember: While some supplements may help arthritis symptoms, nothing can substitute doctor-prescribed medications, a healthy diet and exercise. Always talk to your doctor before adding a new supplement, vitamin or mineral to your regimen. Just because something is natural doesnt mean it cant cause side effects or interact with medications. For more tips on choosing safe supplements, read this article.
Calcium
What it does: Calcium is an essential mineral thatmaintains strong bones and teeth regulates muscle contractions transmits nerve impulses and helps release essential hormones and enzymes. It also helps prevent osteoporosis and fractures, which are higher risks among people with rheumatoid arthritis and those taking corticosteroids.
How much:Experts recommend 1,200 mg a day for healthy adults, but people with inflammatory arthritis may need more up to 1,500 mg for men and postmenopausal women. Recent research has debunked the claim that calcium supplements raise heart attack risk.
Too much:Tolerable upper limit = 2,500 mg.
Chromium
Too much:No tolerable upper limit has been determined.
Iron
Don’t Miss: What Is The Best Thing For Arthritis In The Knee
Causes And Symptoms Of Rheumatoid Arthritis
Regrettably, scientists have yet to discover the precise cause of RA. Nonetheless, genetics can play a role in the development of this illness. Worse still, children as young as two years old may develop the disease, while adults normally notice symptoms about the age of 30. Symptoms vary from person to person, but the following are some of the most common:
- Swollen, stiff joints that are warm or painful.
- Stiffness in the morning or after a period of inactivity.
- Fatigue in your joints or general fatigue.
- Weight loss that isnt clarified.
A blood test is the safest way to diagnose RA because it checks for stuff like:
- C-reactive protein
- Antibody factor for rheumatoid arthritis
- Antibodies against cyclic citrullinated peptides
- Erythrocyte sedimentation rate has increased
- Iron deficiency anemia
Aside from that, the doctor can order imaging tests to determine what is going on in the affected areas and to monitor treatment progress.
Also Check: How Often Do You Use Vitamin C Serum
Vitamin D And Autoimmune Diseases
Autoimmune diseases are diseases where the immune system’s ability to discriminate between self- and non-self tissue fails. People with diseases like multiple sclerosis , arthritis, and inflammatory bowel diseases have T cells that target self and drive the immune system to induce inflammation in the peripheral tissues. The causes of the inappropriate immune attacks are not known however, it is clear that several risk factors play a role. Vitamin D status has been linked to
Don’t Miss: What’s Best For Arthritis Hot Or Cold
Individual Food Items In Diet And Their Relevance To Ra
In an average diet comprising of breakfast, lunch, and dinner, there are several food items which are rich source of some phytochemicals and their efficacy in eradication of diseases has been known and is included under traditional medicines on which 80% of the world population relies . Food items such as dietary fibers, cooking oil, polyphenols, bioactive compounds from several herbs and beverages like tea are among the cheapest sources of medication however, their bioavailability has always been a matter of concern.
Recommended Reading: How Early Should I Start Taking Prenatal Vitamins
Study Examined Cells From Inflamed Joints
In their journal paper, the researchers explain that previous studies have revealed that vitamin D has potent anti-inflammatory effects, including the ability to suppress activity in some types of immune system T cell that are known to be active in rheumatoid arthritis.
However, those studies have only used immune cells isolated from blood, and so the impact of vitamin D on immune cells at the site of active disease is unclear.
A significant feature of the new study is that it is the first to use immune cells taken from both the blood and from the inflamed joints of people with rheumatoid arthritis.
Unlike previous studies, explains senior study author Karim Raza, a professor in the Institution of Inflammation and Ageing at the University of Birmingham, we isolated different immune cell types from the actual site of disease to determine whether specific subsets of immune cells have equal sensitivity to vitamin D.
Also Check: Can You Reverse Psoriatic Arthritis
The Connection Between Vitamin D And Rheumatoid Arthritis
Vitamin D , or vitamin sunshine, has a miraculous ability to promote health in our body.
Strong bones, cancer prevention, healthy blood pressure, and a strong immune system are all positively correlated to adequate vitamin D levels.
In fact, the medical community, as a whole, touts vitamin D as a foundational building block to good health.
Vitamin D can help regulate the immune system, ward off sickness and disease and if youre taking medication that lowers immune system defenses it can help you from getting sick as often. -Karen Langston, spokesperson for the National Association of Nutrition Professionals
Rheumatoid arthritis is no exception.
It appears that vitamin D deficiency is highly prevalent in patients with RA, and that vitamin D deficiency may be linked to disease severity in RA.
As vitamin D deficiency has been linked to diffuse musculoskeletal pain, these results have therapeutic implications.
Vitamin D supplementation may be needed both for the prevention of osteoporosis as well as for pain relief in patients with RA. U.S. National Library of Medicine, National Institutes of Health
Physicians and rheumatologists cannot say that healthy vitamin D levels will prevent or cure RA. Rheumatoid arthritis is far too complex with a multitude of variables.
Yet, there is enough evidence for doctors, scientists, and researchers to prescribe vitamin D to RA patients and those at risk for RA.
You May Like: Does Vitamin D Make You Tired
Vitamin D And Ra Medications
Some RA medications can raise your risk of vitamin D deficiencies, which can lead to complications.
According to an older 2011 study, people who take oral glucocorticoids have an increased risk of 25D deficiency. Theyre twice as likely to be short on this form of vitamin D than the average person.
Glucocorticoids, also known as corticosteroids, are sometimes used to help treat RA.
Reduced levels of vitamin D and calcium are also common side effects of prednisone, a glucocorticoid that may be administered orally or via injection. As a result, prednisone use is becoming less common for people with RA.
There are multiple ways to boost your vitamin D intake.
Also Check: Is Coffee Good For Rheumatoid Arthritis
Vitamin D And The Immune System
The classic function of vitamin D is to enhance intestinal absorption of calcium by regulating several calcium transport proteins in the small intestine . However, various cells express the vitamin D receptor and the vitamin D activating enzyme 1hydroxylase. Various cells of the immune system also express the VDR and harbor 1hydroxylase . Thus, cells of the immune system respond to vitamin D and also activate vitamin D in a paracrine or autocrine fashion. The extra-renal 1hydroxylase is not upregulated by PTH, and thus, production of 1,252D3 is dependent on concentrations of the substrate 25D3, and it may be regulated by inflammatory signals, such as lipopolysaccharide and cytokines . Cells of the immune system, which express the VDR and harbor 1hydroxylase, are macrophages, T cells, dendritic cells, monocytes, and B cells . Vitamin D is involved in the regulation of the innate immunity as it enhances the defense system of the organism against microbes and other pathogenic organisms, and it modulates the adaptive immune system through direct effects on T-cell activation and on the phenotype and function of antigen-presenting cells, particularly dendritic cells.
Figure 1.
Vitamin D And Immunity
The multi-modal innate immune system is the bodys first line of defence against pathogens, comprising physical barriers , chemical barriers , complement proteins and cellular responses such as those mediated by macrophage, DC and neutrophils. Vitamin D participates in several of these processes, including the maintenance of barrier function in the intestine, by regulating tight junctions and intestinal epithelial cell apoptosis . However, to date, studies of vitamin D and innate immunity have predominantly explored its impact on antigen-presenting cells, such as macrophages and DC, which participate in the recognition of and response to pathogen-associated molecular patterns via pattern recognition receptors . DNA target sequences for 1,25-2D3-bound to VDR, referred to as vitamin D response elements have been found in multiple genes associated with PRR responses, including the antibacterial proteins NOD2 , hepcidin antimicrobial protein , cathelicidin , B-defensin 2 and TREM-1 . Toll-Like Receptors are an important group of PRR, and 1,25-2D3 has been shown to downregulate TLR2 and TLR4 in monocytes , abrogating over-elaboration of TLR immune responses to PAMPs and damage-associated molecular patterns . In a separate study, methylation of the Vitamin D Receptor gene and single-nucleotide polymorphisms in the VDR were also found to alter VDR-mediated TLR1/2 signalling in monocytes .
You May Like: Is Oats Good For Arthritis
Vitamin D And Raexperimental Evidence
The 25D-1–hydroxylase enzyme is expressed in many cells of the immune system including activated macrophages and dendritic cells. The 1,252D that is produced acts in an autocrine/paracrine manner, resulting in down-regulation of antigen-presenting cells, inhibition of T-cell proliferation and decreased production of Th1 cytokines IL-2, IFN- and TNF-. The VDR has been demonstrated in macrophages, chondrocytes and synoviocytes in rheumatoid synovium and sites of cartilage erosion in RA patients, but not in tissues from control subjects . In the CIA model in rodents, 1,252D supplementation prevents initiation and progression of inflammatory arthritis . Further detail can be found in a recent review article by Arnson et al. .
Upping Your Vitamin D Intake Has Been Shown To Help With Symptoms Of Rheumatoid Arthritis
Vitamin D helps the body absorb calcium, which is essential for building strong bones. Too little of this vital nutrient can lead to having thin, soft and brittle bones, known as osteomalacia in adults and rickets in children.
Studies also have found that a lack of vitamin D is linked to rheumatoid arthritis, an autoimmune disease characterized by swollen, aching joints and numbness and tingling in the hands and feet.
In a study published in the Journal of Clinical Rheumatology, scientists found that vitamin D deficiency not only is highly prevalent in rheumatoid arthritis patients, but its also related to chronic pain and lower mental and physical quality of life scores. Another study revealed that a higher intake of vitamin D and omega-3 fatty acids may be associated with better treatment results in patients with early rheumatoid arthritis.
Read Also: What Effect Does Alcohol Have On Arthritis
Vitamin D Levels And Ra Development
Vitamin D is known to play a key role in the regulation of immune function, and many inflammatory autoimmune diseases, including RA, have been associated with vitamin D deficiency.1,2 A 2012 meta-analysis that assessed the link between vitamin D intake and the development of RA included 3 cohort studies involving 215,757 participants and 874 incident cases of RA.3 The study found an association between total vitamin D intake and RA incidence , without between-study heterogeneity . Individuals in the highest intake group had a 24.2% lower risk of developing RA than those in the lowest intake group. There was also a significant association between vitamin D supplement intake and RA incidence , without between-study heterogeneity, indicating increased RA risk with low vitamin D intake.
Reduce Foods That Cause Inflammation
Many studies indicate a positive effect of an anti-inflammatory diet on disease activity in patients with RA. A non-inflammatory diet controls inflammation and reduces discomfort.
Foods that contain refined carbohydrates, gluten, and red meat are inflammatory and should be avoided or eaten in moderation.
The glycemic index of carbohydrates has a strong influence on systemic inflammation. The higher the glycemic index, the more inflammatory the carbohydrate. Whole grains have a lower glycemic index and are rich in fiber. Fiber decreases carbohydrates absorption and decreases mediators of inflammation therefore, whole-grain carbohydrates should be consumed daily.
However, it is advised that the whole grains consumed are gluten-free. Since gluten, a mixture of hundreds of proteins found in wheat grains triggers an altered immune response in RA. .
A few studies show that a gluten-free, vegan diet followed for one year was associated with anti-inflammatory properties and a significant decrease in RA disease activity .
Also, a high total protein supply has been associated with an increased risk of inflammation in RA patients. Therefore, protein from plant sources such as legumes is the best protein source for people suffering from RA. Legumes have also been shown to have anti-inflammatory properties.
Red meat intake should also be limited ,
The foods with the highest anti-inflammatory properties include:
All of these decrease markers of inflammation
Also Check: Is Cherry Juice Good For Rheumatoid Arthritis