Amplification In The Synovium
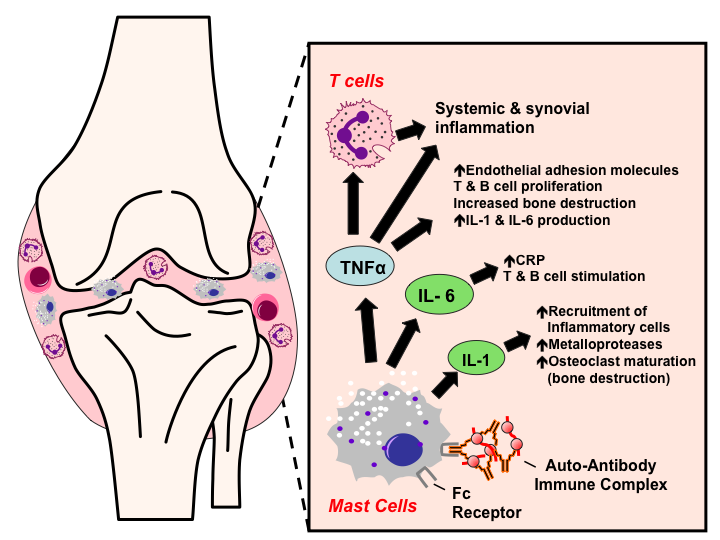
Once the generalized abnormal immune response has become established which may take several years before any symptoms occur plasma cells derived from B lymphocytes produce rheumatoid factors and ACPA of the IgG and IgM classes in large quantities. These activate macrophages through Fc receptor and complement binding, which is part of the intense inflammation in RA. Binding of an autoreactive antibody to the Fc receptors is mediated through the antibody’s N-glycans, which are altered to promote inflammation in people with RA.
This contributes to local inflammation in a joint, specifically the synovium with edema, vasodilation and entry of activated T-cells, mainly CD4 in microscopically nodular aggregates and CD8 in microscopically diffuse infiltrates. Synovial macrophages and dendritic cells function as antigen-presenting cells by expressing MHC class II molecules, which establishes the immune reaction in the tissue.
Where Can People Get Additional Information On Rheumatoid Arthritis
For more information about rheumatoid arthritis as well as living with RA and for support groups, please consider the following:
- National Institute of Arthritis: https://www.niams.nih.gov/health-topics/rheumatoid-arthritis
- National Arthritis and Musculoskeletal and Skin Diseases Clearinghouse
Box AMS
Vitamin D And Fish Oil Supplements May Reduce Risk Of Autoimmune Disease Rheumatoid Arthritis Psoriasis And Thyroid
With a more pronounced effect after two years of supplementation.
Taking daily vitamin D supplements or a combination of vitamin D and omega-3 fish oil appears to carry a lower risk of developing autoimmune disease, with a more pronounced effect after two years, finds a trial of older US adults published by The BMJ today .
The researchers say the clinical importance of these findings is high, given that these are well-tolerated, non-toxic supplements, and that there are no other known effective therapies to reduce rates of autoimmune diseases.
Autoimmune disease happens when the bodys natural defense system mistakenly attacks normal cells. Common conditions include rheumatoid arthritis, psoriasis, and thyroid diseases, which increase with age, particularly among women.
Both vitamin D and omega-3 fatty acids derived from seafood are known to have a beneficial effect on inflammation and immunity, but no large randomized trials have tested whether these supplements can lower the risk of autoimmune disease.
So researchers set out to test the effects of vitamin D and omega-3 fish oil supplements on rates of autoimmune diseases in 25,871 US adults .
When they joined the trial, participants provided information on their age, ethnicity, region of residence, income, education, lifestyle, weight, medical history, diet, and supplement use. Blood levels of vitamin D and omega-3 fatty acids were also measured.
Recommended Reading: Mayo Clinic Arthritis Treatment
F How Do We Document And Evaluate Hiv Infection
Any individual with HIV infection, including one with a diagnosis of acquired immune deficiency syndrome , may be found disabled under 14.11 if his or her impairment meets the criteria in that listing or is medically equivalent to the criteria in that listing.
1. Documentation of HIV infection.
a. Definitive documentation of HIV infection. We may document a diagnosis of HIV infection by positive findings on one or more of the following definitive laboratory tests:
HIV antibody screening test , confirmed by a supplemental HIV antibody test such as the Western blot , an immunofluorescence assay, or an HIV-1/HIV-2 antibody differentiation immunoassay.
HIV nucleic acid detection test .
HIV p24 antigen test.
Isolation of HIV in viral culture.
Other tests that are highly specific for detection of HIV and that are consistent with the prevailing state of medical knowledge.
b. We will make every reasonable effort to obtain the results of your laboratory testing. Pursuant to §§ 404.1519f and 416.919f, we will purchase examinations or tests necessary to make a determination in your claim if no other acceptable documentation exists.
c. Other acceptable documentation of HIV infection. We may also document HIV infection without definitive laboratory evidence.
2. Documentation of the manifestations of HIV infection.
c. Other acceptable documentation of manifestations of HIV infection. We may also document manifestations of HIV infection without definitive laboratory evidence.
Ethical Issues Concerning Personalized Prevention

Obvious ethical concerns exist for any type of effort toward personalized prevention. One concern, valid for all studies, observational or interventional, relates to effects, psychological, and/or legal that may occur from notifying an individual that he/she is a high risk for acquiring a serious disease with as yet limited capacity for prevention. Another concern is the risk associated with testing of a drug with potential side-effects in individuals where development of future disease is substantially lower than 100%. The opportunity to prevent disease by modifying environment or lifestyle, addresses to some extent the first concern. The opportunity to treat symptoms, such as arthralgia and bone loss, that may exist in the âpre-RAâ phase with the same therapy as is aimed to prevent arthritis may address the second concern. The main argument, however, remains the wins that may follow from any successful prevention strategy that can be based on the science that requires the contribution from individuals at risk for disease.
Don’t Miss: Rheumatoid Arthritis Thigh Pain
What Are The Treatments
Medicine and lifestyle changes can often control symptoms and slow these diseases.
Medication. Many drugs can now treat RA and other autoimmune disorders. Some are used for pain relief. Others target inflammation. Early treatment with drugs like these may be the best way to prevent joint damage. See your doctor to talk about your options.
Lifestyle choices. While you canât change your genes, you can sometimes change how you live. That can help your treatment work better.
Even if you donât have an autoimmune disease, but you think you might be at risk, these steps may help lower your chances.
E How Do We Document And Evaluate Immune Deficiency Disorders Excluding Hiv Infection
1. General.
a. Immune deficiency disorders can be classified as:
Primary for example, X-linked agammaglobulinemia, thymic hypoplasia , severe combined immunodeficiency , chronic granulomatous disease , C1 esterase inhibitor deficiency.
Acquired for example, medication-related.
b. Primary immune deficiency disorders are seen mainly in children. However, recent advances in the treatment of these disorders have allowed many affected children to survive well into adulthood. Occasionally, these disorders are first diagnosed in adolescence or adulthood.
2. Documentation of immune deficiency disorders. The medical evidence must include documentation of the specific type of immune deficiency. Documentation may be by laboratory evidence or by other generally acceptable methods consistent with the prevailing state of medical knowledge and clinical practice.
3. Immune deficiency disorders treated by stem cell transplantation.
a. Evaluation in the first 12 months. If you undergo stem cell transplantation for your immune deficiency disorder, we will consider you disabled until at least 12 months from the date of the transplant.
b. Evaluation after the 12-month period has elapsed. After the 12-month period has elapsed, we will consider any residuals of your immune deficiency disorder as well as any residual impairment resulting from the treatment, such as complications arising from:
Graft-versus-host disease.
Immunosuppressant therapy, such as frequent infections.
Recommended Reading: Coping With Rheumatoid Arthritis
What Are The Four Stages Of Rheumatoid Arthritis
The American College of Rheumatology has developed a system for classifying rheumatoid arthritis that is primarily based upon the X-ray appearance of the joints. This system helps medical professionals classify the severity of your rheumatoid arthritis with respect to cartilage, ligaments, and bone. The system defines the four stages of RA as follows:
Stage I
- No damage was seen on X-rays, although there may be signs of bone thinning
Stage II
Foods to avoid with RA
There is no special RA diet or diet “cure” for rheumatoid arthritis. However, it is thought that a healthy diet is an important complement to medication in the treatment of rheumatoid arthritis. Research is suggesting that the different kinds of bacteria in our intestines has a big impact on rheumatoid arthritis. Diet is likely important, but we do not know of specific foods or food groups that should be universally avoided by individuals with rheumatoid arthritis.
Diets higher in fish, grains, and vegetables decrease the risk of developing RA. The Western diet, defined as including more processed meats, increases the risk. It is not certain whether this is because of a direct anti-inflammatory effect of the fish, grains, and vegetables or because of changes in the natural bacteria in the gut.
Foods that fight RA inflammation
Supplements for RA
Exercises and home remedies for RA
How Do Mrna Vaccines Work
Oftentimes, vaccines contain a weakened, live version of a virus, a dead version of a virus, or a part of a virus so that the body can recognize and react. When the body sees these parts of vaccines, it makes antibodies against them. These antibodies can then be used as protection in the future if a person is ever exposed to that particular virus. This is what can potentially give a person immunity.
An mRNA vaccine is different from past vaccines in that it only carries instructions . These instructions, the mRNA, go into our bodys cells and tell the cell to start making a specific protein. In the case of the COVID-19 vaccine, cells are told to make a protein on the COVID-19 virus particle called the spike protein. The spike protein helps COVID-19 get into the body and start infecting cells.
When we start making this foreign protein, our bodies react and make antibodies, just like they would in other vaccines. The difference is, the mRNA vaccines only deliver the instructions and not any part of the actual virus. This makes it impossible to develop COVID-19 from the vaccine or for parts of the mRNA to get into our cells permanently. If a person who is vaccinated is exposed to COVID-19 later on, these antibodies can reactivate and protect them from the virus before getting sick. Even if a person does still get COVID-19, the antibodies may help prevent severe illness from developing.3-7
Recommended Reading: Arthritis At 30 Symptoms
What Are The Symptoms Of Inflammatory Arthritis
The most common symptoms of inflammatory arthritis are:
- Joint pain and stiffness after periods of rest or inactivity, particularly in the morning
- Swelling, redness and/or a feeling of warmth in the affected joints
- Inflammation of other areas in the body, such as the skin or internal organs like the lungs and heart
People with inflammatory arthritis generally experience alternating periods of “flares” of highly intense symptoms with periods of inactivity.
How Are Autoimmune Diseases Diagnosed
Doctors often have a hard time diagnosing autoimmune diseases. There’s usually not a specific test to show whether you have a certain autoimmune disease. And the symptoms can be confusing. That’s because many autoimmune diseases have similar symptoms. And some symptoms, such as muscle aches, are common in many other illnesses. So it can take a long time and some visits to different types of doctors to get a diagnosis.
To help your doctor find out if an autoimmune disease is causing your symptoms,:
- Learn about the health conditions in your family history. What health problems did your grandparents, aunts, uncles, and cousins have? Write down what you learn and share it with your doctor.
- Keep track of your symptoms, including how long they last and what makes them better or worse. Share your notes with your doctor.
- See a specialist who deals with the symptoms that bother you most. For example, if you have rash, see a dermatologist .
Read Also: Does Arthritis Cause Redness
What Are Newer Rheumatoid Arthritis Medications And Side Effects
Newer “second-line” drugs for the treatment of rheumatoid arthritis include the following:
Each of these medicines can increase the risk for infections, and the development of any infections should be reported to the doctor when taking these newer second-line drugs.
While biologic drugs are often combined with DMARDs in the treatment of RA, they are generally not used with other biologics due to the risk of serious infections. Similarly, JAK inhibitor medication is not used with traditional biologic medicines.
What Is Niehs Doing
Unraveling the genetic and environmental underpinnings of autoimmune disease is a focus at NIEHS and the National Toxicology Program . Progress happens through multiple research efforts, such as:
Fact Sheets
This content is available to use on your website.
Recommended Reading: Mayo Clinic On Arthritis
Tumor Necrosis Factor Inhibitors
Tumor necrosis factor alpha is a pro-inflammatory cytokine produced by macrophages and lymphocytes. It is found in large quantities in the rheumatoid joint and is produced locally in the joint by synovial macrophages and lymphocytes infiltrating the joint synovium. TNF is one of the critical cytokines that mediate joint damage and destruction due to its activities on many cells in the joint as well as effects on other organs and body systems. TNF antagonists were the first of the biological DMARDS to be approved for the treatment of RA. These drugs began to enter the market for rheumatoid arthritis in 1999 and are now considered a part the ACR recommendations for treatment of RA. There are currently five TNF inhibitors FDA approved for the treatment of RA etanercept , infliximab , adalimumab , certolizumab pegol , and golimumab . Etanercept is a soluble TNF receptor-Fc immunoglobulin fusion construct infliximab, adalimumab, and golimumab are monoclonal antibodies and certolizumab pegol is an anti-TNF antigen binding domain-polyethylene glycol construct. While differing in structure, the efficacy and safety of the drugs is similar across the class in reducing the signs and symptoms of RA, as well as in slowing or halting radiographic damage, when used either as monotherapy or in combination with methotrexate.
What Are Autoimmune Diseases
Your immune system protects you from disease and infection by attacking germs that get into your body, such as viruses and bacteria. Your immune system can tell that the germs aren’t part of you, so it destroys them. If you have an autoimmune disease, your immune system attacks the healthy cells of your organs and tissues by mistake.
There are more than 80 types of autoimmune diseases. They can affect almost any part of your body. For example, alopecia areata is an autoimmune disease of the skin that causes hair loss. Autoimmune hepatitis affects the liver. In type 1 diabetes, the immune system attacks the pancreas. And in rheumatoid arthritis, the immune system can attack many parts of the body, including the joints, lungs, and eyes.
Also Check: How To Ease Arthritis
Signs And Symptoms Of Autoimmune Disease
Autoimmune diseases can develop from a variety of factors with no known definitive causes for the onset of the disease. Some suspected sources are:
- Bacterial or viral infection
- Chemical toxins
- Environmental pollutants
When the immune system determines that healthy cells are foreign, it begins to produce antibodies to fight off the healthy cells it believes to be the source of an illness or infection. When an autoimmune disease is suspected, a rheumatologist will administer tests to determine what antibodies are being produced. There are more than 80 potential autoimmune diseases and some of the most common areas affect can be:
- Joints and muscles
- Blood vessels
- Connective tissue
When faced with symptoms or an autoimmune disease diagnosis, it is very important to seek treatment from an experienced rheumatologist to find the best plan to manage symptoms. Dr. Susan Baker, MD specializes in Rheumatology and Internal Medicine in Beverly Hills, and offers patients everything from arthritis treatment to Lupus.
What Is The Prognosis For Rheumatoid Arthritis Patients
- With early, aggressive treatment, the outlook for those affected by rheumatoid arthritis can be very good.
- The overall attitude regarding the ability to control the disease has changed tremendously since the turn of the century. Doctors now strive to eradicate any signs of active disease while preventing flare-ups.
- The disease can be controlled and a cooperative effort by the doctor and patient can lead to optimal health.
- Rheumatoid arthritis causes disability and can increase mortality and decrease life expectancy to lead to an early death.
- Patients have a less favorable outlook when they have deformity, disability, ongoing uncontrolled joint inflammation, and/or rheumatoid disease affecting other organs of the body.
- Overall, rheumatoid arthritis tends to be potentially more damaging when rheumatoid factor or citrulline antibody is shown by blood testing. Life expectancy improves with earlier treatment and monitoring.
- Finally, minimizing emotional stress can help improve the overall health of people with rheumatoid arthritis. Support and extracurricular groups provide those with rheumatoid arthritis time to discuss their problems with others and learn more about their illness.
Is there a cure for RA?
No, rheumatoid arthritis is not a curable disease at this time. As the science of genetics and disease, as well as autoimmunity, evolve, it is very likely that cures for rheumatoid arthritis will become available.
Don’t Miss: Mild Psoriatic Arthritis Rash
How Can Rheumatoid Arthritis Be Managed
The specific causes of rheumatoid arthritis are unknown, but there are a number of factors associated with an increased risk of developing the disease including family history, smoking, increased age and occupational exposures.Footnote 4Footnote 5 While there is no cure for rheumatoid arthritis, there are treatment options which aim to alleviate joint symptoms and improve function. Individuals often work with a rheumatologist to develop a treatment plan to prevent further joint damage. Medication is often prescribed as a first line of therapy and is key to controlling disease and preventing damage. Other ways to manage include physical therapy, occupational therapy and education.Footnote 6 Individuals with rheumatoid arthritis who are diagnosed and treated early are less likely to experience long-term joint damage and functional impairments.
What Is The Difference Between Osteoarthritis And Inflammatory Arthritis
The major distinction between OA and IA is that:
- Osteoarthritis is caused by physical use wear and tear of a joint over time .
- Inflammatory arthritis is a chronic autoimmune disease in which your immune system misidentifies your own body tissues as harmful germs or pathogens and attacks them. The result is inflammation of the affected tissues in and around joints.
Because OA involves physical wear on joints in the body, it usually appears in people after the age of 50. The older you get, the more likely you are to get osteoarthritis.
Since inflammatory arthritis is a chronic disease, it affects people of all ages, often striking people in their peak working and child-rearing age. IA diseases can often be diagnosed in patients as young as age 20 or 30. Less commonly, kids and teens may be diagnosed with a form of childhood arthritis, such as . IA is more common in females than in males, and it is not understood why.
Don’t Miss: What Does Arthritis Do To The Body