Why Does The Immune System Attack The Body
Doctors dont know exactly what causes the immune-system misfire. Yet some people are more likely to get an autoimmune disease than others.
According to a 2014 study, women get autoimmune diseases at a rate of about 2 to 1 compared to men 6.4 percent of women vs. 2.7 percent of men. Often the disease starts during a womans childbearing years .
Some autoimmune diseases are more common in certain ethnic groups. For example, lupus affects more African-American and Hispanic people than Caucasians.
Certain autoimmune diseases, like multiple sclerosis and lupus, run in families. Not every family member will necessarily have the same disease, but they inherit a susceptibility to an autoimmune condition.
Because the incidence of autoimmune diseases is rising, researchers suspect environmental factors like infections and exposure to chemicals or solvents might also be involved.
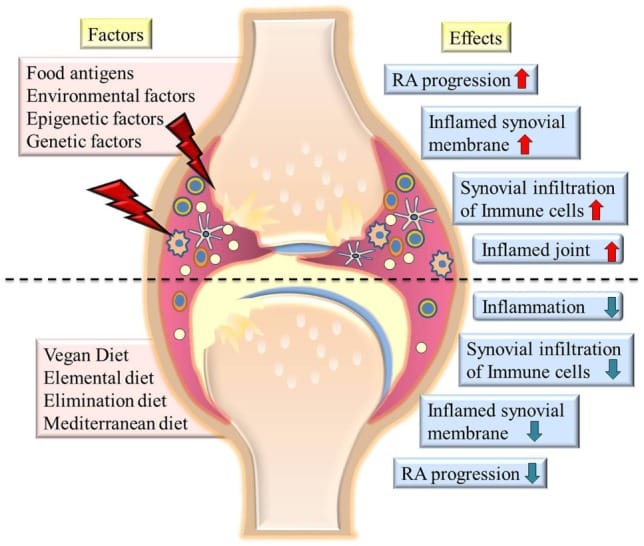
A Western diet is another suspected risk factor for developing an autoimmune disease. Eating high-fat, high-sugar, and highly processed foods is thought to be linked to inflammation, which might set off an immune response. However, this hasnt been proven.
A 2015 study focused on another theory called the hygiene hypothesis. Because of vaccines and antiseptics, children today arent exposed to as many germs as they were in the past. The lack of exposure could make their immune system prone to overreact to harmless substances.
What Are The Early Signs Of Rheumatoid Arthritis
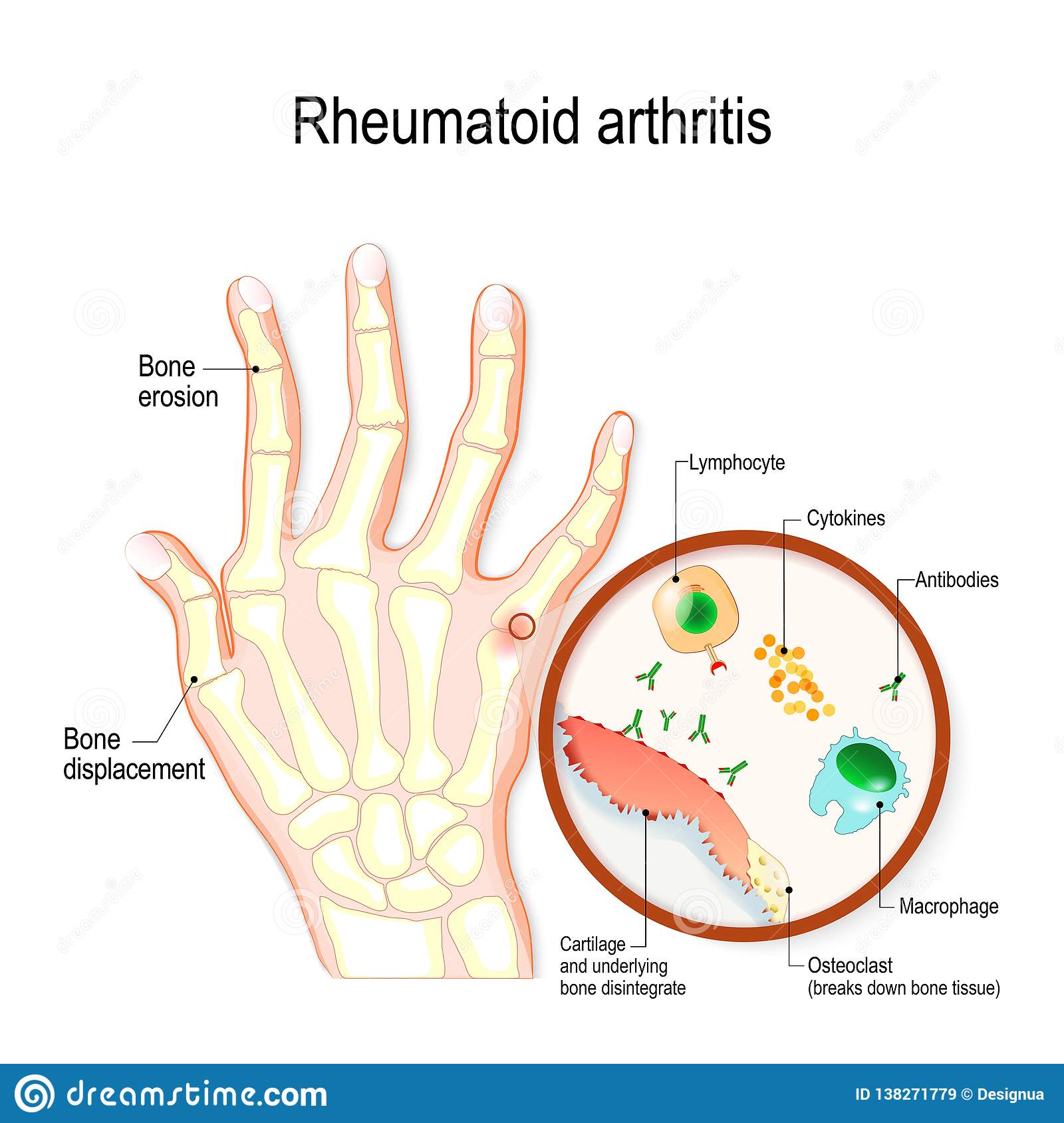
Early signs of rheumatoid arthritis include tenderness or pain in small joints like those in your fingers or toes. Or you might notice pain in a larger joint like your knee or shoulder. These early signs of RA are like an alarm clock set to vibrate. It might not always been enough to get your attention. But the early signs are important because the sooner youre diagnosed with RA, the sooner your treatment can begin. And prompt treatment may mean you are less likely to have permanent, painful joint damage.
Osteoarthritis: Causes Risk Factors And Treatment
Osteoarthritis is the most common form of arthritis in the United States, affecting roughly 12 percent of Americans aged 25 74. Its a chronic joint disease that breaks down cartilage in the neck, lower back, knees, hips, shoulders, and/or fingers. Common symptoms are pain, stiffness, and limited joint movement.
Read Also: What Are The Various Types Of Arthritis
Who Should Diagnose And Treat Ra
A doctor or a team of doctors who specialize in care of RA patients should diagnose and treat RA. This is especially important because the signs and symptoms of RA are not specific and can look like signs and symptoms of other inflammatory joint diseases. Doctors who specialize in arthritis are called rheumatologists, and they can make the correct diagnosis. To find a provider near you, visit the database of rheumatologistsexternal icon on the American College of Rheumatology website.
Is Osteoarthritis A Chronic Inflammatory Condition
The development of chronic inflammation in OA following joint trauma or overuse can be understood as a vicious, self-perpetuating cycle of local tissue damage, inflammation, and repair, such that the OA joint has been likened to a chronic wound .
Why do you get inflammation with osteoarthritis?
It was thought that the inflammation is caused by cartilage fragments that break off and irritate the synovium . However, MRIs taken during the early stages of osteoarthritis sometimes detect synovitis inflammation even though the joint cartilage still appears normal.
Is the pain of osteoarthritis an autoimmune disease?
Even most of them can become chronic and incurable but many of them are treatable. Osteoarthritis is not an autoimmune disease! Joint pain and stiffness are very common in OA. Even in severe case, it can cause swelling in the affected joint. But the symptoms of OA also can be found in other forms of arthritis.
What does auto immune mean in inflammatory arthritis?
This is the meaning of auto-immunity . Different kinds of inflammatory arthritis reflect a set of auto-immune diseases where the body cannot distinguish between its own healthy cells and tissues and a foreign substance. turned on ones self.
Is there an autoimmune disease associated with OA?
The good news, OA has nothing to do with the function of your body immune system. But there is also a kind of arthritis associated with autoimmune disorder this type is called rheumatoid arthritis .
You May Like: What Can You Do To Help Arthritis In Your Knees
Current Opinions For Vaccination Of Patients With Airds
Patients with AIRDs exhibit reduced vaccine efficacy with the potential for side effects. The current opinions for administering vaccines to patients with rheumatic diseases are described as follows:
The EULAR notes that, as of February 2022, there are insufficient data on the COVID-19 vaccine status in patients with rheumatic diseases and those receiving immunosuppressive treatment however, several vaccines can be safely administered as we lack evidence to discourage their use, especially in patients with RMD. Precautions include administering the vaccine when the disease is stable or before the start of treatment if the patient is receiving immunosuppressive drugs intermittently. The organization also suggests that immunosuppressive drugs other than rituximab should not be discontinued to facilitate vaccination. Furthermore, a single vaccination schedule, which includes a third dose at least one month after the second dose, is recommended to prevent weakening of vaccine efficacy owing to long-term use of rituximab, cyclophosphamide, MMF, abatacept, or prednisone at a dose of 10 mg/day in most countries.
Both the EULAR and the ACR have taken positions recommending vaccination for patients with AIRD, and clinicians should consider these comments when deciding whether to vaccinate a patient.
Medications To Manage Symptoms
Some drugs can help relieve symptoms and slow the diseases progression.
Nonsteroidal anti-inflammatory drugs are available from pharmacies over the counter . Examples include Motrin, Advil, and Aleve. Long-term use and high doses can lead to side effects, including:
- high blood pressure
- kidney and liver problems
Corticosteroids reduce pain and inflammation and may help slow joint damage, but they cannot cure RA. If NSAIDs do not work, a doctor may inject a steroid into the joint. Relief is usually rapid, but the effect is variable. It can last a few weeks or months, depending on the severity of the symptoms.
Corticosteroids can help with acute symptoms or short-term flare-ups. However, a doctor will limit these injections to no more than three times per year because of their impact on the soft tissue structures around the joints. More frequent injections can potentially damage these structures or cause them to tear off from where they attach to bone.
Learn more about steroid injections here.
Recommended Reading: What Is Arthritis In The Knee Called
What Is Niehs Doing
Unraveling the genetic and environmental underpinnings of autoimmune disease is a focus at NIEHS and the National Toxicology Program . Progress happens through multiple research efforts, such as:
Fact Sheets
This content is available to use on your website.
Recommended Reading: Mayo Clinic On Arthritis
How Is Ra Treated
RA can be effectively treated and managed with medication and self-management strategies. Treatment for RA usually includes the use of medications that slow disease and prevent joint deformity, called disease-modifying antirheumatic drugs biological response modifiers are medications that are an effective second-line treatment. In addition to medications, people can manage their RA with self-management strategies proven to reduce pain and disability, allowing them to pursue the activities important to them. People with RA can relieve pain and improve joint function by learning to use five simple and effective arthritis management strategies.
Recommended Reading: Is Cosamin Good For Arthritis
What Medications Treat Rheumatoid Arthritis
Early treatment with certain drugs can improve your long-term outcome. Combinations of drugs may be more effective than, and appear to be as safe as, single-drug therapy.
There are many medications to decrease joint pain, swelling and inflammation, and to prevent or slow down the disease. Medications that treat rheumatoid arthritis include:
Non-steroidal anti-inflammatory drugs
Biologics tend to work rapidly within two to six weeks. Your provider may prescribe them alone or in combination with a DMARD like methotrexate.
History Of Inflammation And Autoimmune Disease
Around150 years ago, research on multiple sclerosis cast doubt on the reputation of inflammation. The inflammatory response hadlong been viewed as an important component of the bodys defense against infection and a healing mechanism for damaged tissue . But when a French neurologistreported the presence of inflammation in areas of multiple sclerosis lesions in the central nervous system, the evidence suggested it might actually cause harm.
This idea was reinforced in the 1980s when a team of British scientists found aslew of inflammation-inducing molecules called cytokines in the joints of patientssuffering from rheumatoid arthritis . The group went on to make a convincing case that inflammation was a driver, not a bystander, of disease. They showed that antibodies that blocked one type of cytokines TNF alpha dampened other cytokine levels in the joint tissues growing in the lab, and provided patients in clinical trials with almost immediate symptom relief. The work led to the development of infliximab as atargetedtherapy for rheumatoid arthritis, as well as ulcerative colitis, psoriasis, and other autoimmune diseases.
Recommended Reading: Is My Knee Pain Arthritis
What Can I Do To Prevent Osteoarthritis
Maintaining a healthy lifestyle may help prevent osteoarthritis. Eating nutritious foods, maintaining a healthy weight throughout your life, and exercising regularly to strengthen muscles that protect the joints are three very important methods that may reduce your risk of developing osteoarthritis.
Autoimmune Disease And Stress: Is There A Link
- By Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing
A new study has raised the possibility that stress may cause autoimmune disease, such as lupus or rheumatoid arthritis, because it found a higher incidence of autoimmune diseases among people who were previously diagnosed with stress-related disorders.
I have patients who heard about this research and are saying, I knew it!
But before we accept a potential link between stress and autoimmune disease, lets look at some details of the study and consider how we define the terms autoimmune disease,stress, and stress-related disorder.
Read Also: Who To See For Arthritis
What Are The Symptoms Of Rheumatoid Arthritis
Rheumatoid arthritis affects everyone differently. In some people, joint symptoms develop over several years. In other people, rheumatoid arthritis symptoms progress rapidly. Many people have time with symptoms and then time with no symptoms .
Symptoms of rheumatoid arthritis include:
- Pain, swelling, stiffness and tenderness in more than one joint.
- Stiffness, especially in the morning or after sitting for long periods.
- Pain and stiffness in the same joints on both sides of your body.
F How Do We Document And Evaluate Hiv Infection
Any individual with HIV infection, including one with a diagnosis of acquired immune deficiency syndrome , may be found disabled under 14.11 if his or her impairment meets the criteria in that listing or is medically equivalent to the criteria in that listing.
1. Documentation of HIV infection.
a. Definitive documentation of HIV infection. We may document a diagnosis of HIV infection by positive findings on one or more of the following definitive laboratory tests:
HIV antibody screening test , confirmed by a supplemental HIV antibody test such as the Western blot , an immunofluorescence assay, or an HIV-1/HIV-2 antibody differentiation immunoassay.
HIV nucleic acid detection test .
HIV p24 antigen test.
Isolation of HIV in viral culture.
Other tests that are highly specific for detection of HIV and that are consistent with the prevailing state of medical knowledge.
b. We will make every reasonable effort to obtain the results of your laboratory testing. Pursuant to §§ 404.1519f and 416.919f, we will purchase examinations or tests necessary to make a determination in your claim if no other acceptable documentation exists.
c. Other acceptable documentation of HIV infection. We may also document HIV infection without definitive laboratory evidence.
2. Documentation of the manifestations of HIV infection.
c. Other acceptable documentation of manifestations of HIV infection. We may also document manifestations of HIV infection without definitive laboratory evidence.
You May Like: What Type Of Mattress Is Best For Arthritis
Deterrence And Patient Education
Patients with crystalline arthropathies such as gout require education regarding diet and lifestyle modification which can help manage gout. Patients with chronic inflammatory arthropathies frequently need long-term immunosuppressive medications. They need counseling about the potential benefits and adverse effects of these medications and the necessity for regular monitoring laboratory workups. Finally, they should also understand the importance of regular exercises.
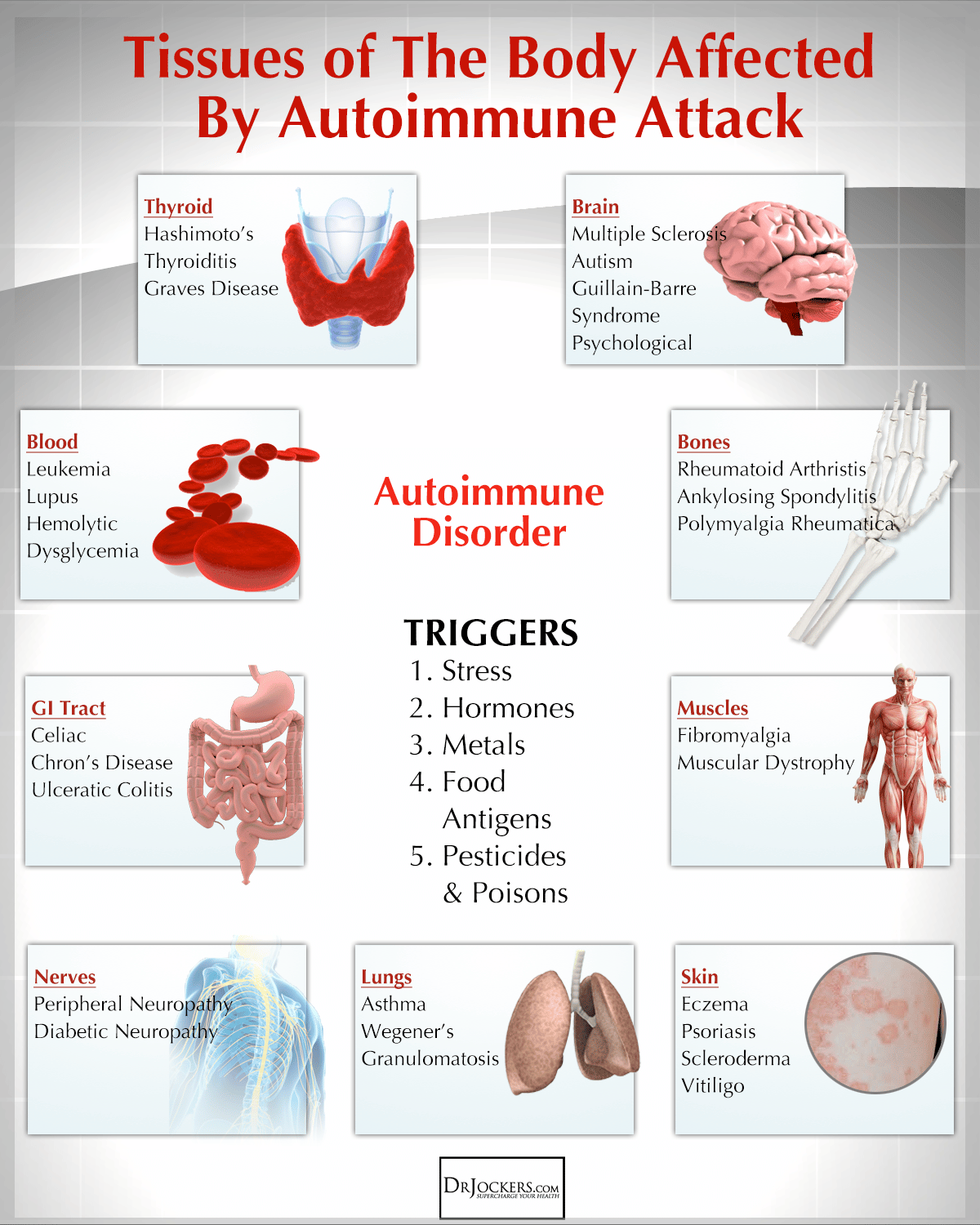
Most Common Autoimmune Diseases
1. Rheumatoid Arthritis Rheumatoid arthritis is a chronic inflammation of the lining of the joints, leading to pain and swelling typically in the hands and feet. It can affect anyone, but is most prevalent in women over 40. Rheumatoid arthritis can sometimes affect other organs as well, such as skin, eyes, lungs and blood vessels. As with all autoimmune disorders, treatment focuses on managing pain and minimizing bone erosion and joint damage.
We have more in-depth information on Rheumatoid Arthritis here.
2. Juvenile Rheumatoid Arthritis Juvenile rheumatoid arthritis is the most common form of arthritis in children under 16. Symptoms usually include pain and swelling in the joints, and can vary from moderate to severe. In some cases, symptoms will subside over time while others can persist well into adulthood.
We have more in-depth information on juvenile rheumatoid arthritis here.
3. Systemic Lupus Erythematosus Lupus can be difficult to diagnose because it shares symptoms with many other disorders. The inflammation resulting from lupus can affect many different areas of the body, from the lungs, heart, joints, skin, kidneys, and brain. Like rheumatoid arthritis, lupus is more prevalent in women and can sometimes be identified by a butterfly-shaped rash on the face, along with photosensitivity, fatigue and fever, joint pain, and other skin lesions that worsen under sun exposure.
We have more in-depth information on lupus here.
You May Like: What Are The Symptoms Of Arthritis In Your Fingers
Study Cohort And Ethics
A total of 20 IgG4-RD patients were enrolled at Peking Union Medical College Hospital between 2020 and 2022 in our study. The diagnosis of IgG4-RD was established according to the 2019 American College of Rheumatology/European League Against Rheumatism classification criteria and the 2011 comprehensive diagnostic criteria for IgG4-RD . Peripheral blood samples were obtained from IgG4-RD patients and age-, sex-, and ethnicity-matched healthy blood donors. Salivary gland tissues were obtained from individuals examined for a possible IgG4-RD diagnosis. The biopsy specimens that showed no inflammation and negative serology were considered as case controls. Demographic and clinical characteristics of the study participants are presented in Supplementary Table . The diagnostic score was calculated according to the 2019 American College of Rheumatology/European League Against Rheumatism classification criteria for IgG4-RD. Disease activity was assessed on the basis of the IgG4-RD responder index .
This study was approved by the Ethics Board of Peking Union Medical College Hospital . All participants signed a written informed consent.
How Can Rheumatoid Arthritis Be Managed
The specific causes of rheumatoid arthritis are unknown, but there are a number of factors associated with an increased risk of developing the disease including family history, smoking, increased age and occupational exposures.Footnote 4Footnote 5 While there is no cure for rheumatoid arthritis, there are treatment options which aim to alleviate joint symptoms and improve function. Individuals often work with a rheumatologist to develop a treatment plan to prevent further joint damage. Medication is often prescribed as a first line of therapy and is key to controlling disease and preventing damage. Other ways to manage include physical therapy, occupational therapy and education.Footnote 6 Individuals with rheumatoid arthritis who are diagnosed and treated early are less likely to experience long-term joint damage and functional impairments.
Also Check: Why Do People Get Rheumatoid Arthritis
Starting And Raising A Family
If you are taking medicines for rheumatoid arthritis, let your healthcare team know if you want to start a family or if you are worried about becoming pregnant while on medication.
Some medications, such as methotrexate, leflunomide and biological treatments, should not be taken by men or women while they are trying for a baby. The doctors and nurses will work with you to ensure your rheumatoid arthritis is controlled while you are trying to get pregnant.
Babies and young children are physically and mentally demanding for any parent, but particularly so if you have rheumatoid arthritis. If you are struggling to cope, it may help to talk to other people in the same situation as you. You may also be able to get additional support from your health visitor or occupational therapist to help you manage your young family.
Overview Of Autoinflammatory Diseases
Your immune system is the network of cells and tissues throughout your body that work together to defend you from viruses, bacteria, and infection. It tries to identify, kill, and eliminate the invaders that might hurt you.
Parts of the immune system include:
- Acquired immune system, which develops as you grow. Invaders provoke your body into producing antibodies so that your body remembers those invaders. Your body can then fight them if they come back.
- Innate immune system, which uses white blood cells instead of antibodies to destroy invaders.
Also Check: What To Do For Arthritis Pain In Thumb
Symptoms Of Autoimmune Diseases
Most autoimmune diseases cause inflammation, which produces redness, heat, pain, and swelling.
Many autoimmune diseases affect more than one part of the body. The symptoms you have will depend on the body part affected, such as:
- Joints, which can cause joint pain, stiffness, and loss of function.
- Thyroid, which might cause you to be tired, gain weight, or have muscle aches.
- Skin, which can cause rashes, blisters, and color changes.