Need For New Therapies
Treatments for these diseases typically have been aimed at decreasing inflammation and pain by slowing down tissue damage and reducing complications. Most people with RA have only a partial response to available drugs, and many only respond to drugs for a limited period of time. In the case of lupus, no effective targeted therapies exist for the most severe forms of the disease. Research is needed to better understand the underlying disease process and identify parts of the immune system that aren’t functioning correctly. This insight will help reveal the most promising new biological targets for drug development and match existing drugs to patients with specific molecular profiles who are most likely to benefit.
Treatment Of Oa And Ra
How Osteoarthritis is Treated
Unfortunately, osteoarthritis cannot be reversed or treated. We offer various treatments and pain relievers to help patients with OA manage unpleasant symptoms.
- Intra-articular injections: Injections of corticosteroids, hyaluronic acid, BOTOX® or platelet-rich plasma in the joints can help to relieve pain in the joints. These injections can provide the missing cushion or padding that the cartilage once provided before it degenerated.
- Physical therapy: Because OA weakens the joints and muscles, physical therapy can help to strengthen the affected joints. Similarly, pain management classes can help patients to minimize the symptoms of OA.
- Pain-relieving medications: Various medications can be taken to relieve the symptoms of OA, dull the pain and discomfort, and reduce swelling. These medications include Tylenol® and NSAIDs .
How Rheumatoid Arthritis is Treated
There is unfortunately no treatment to reverse rheumatoid arthritis either. We can provide various medications along with therapy to help patients manage the symptoms of RA.
- Disease-modifying medications: Various medications, known as DMARDs , can be taken to either slow the progression of RA or stop the progression entirely. These treatments can save the joints from further damage.
Getting The Right Diagnosis
If you think you have psoriasis, see your doctor right away. It shouldnât take long to get an answer once youâre there. Usually, all it takes to diagnose psoriasis is a discussion about your medical history and an exam of your skin, scalp, and nails. Some doctors may also take a small sample of skin to examine under a microscope. This test is called a biopsy.
While youâre at the doctor, be sure to speak up if you have any other symptoms besides skin and/or nail problems especially if you have joint issues, including:
- Morning stiffness that improves during the day
- Swelling just above your heel
- Swollen or tender joints
Because psoriasis often goes along with PsA, youâll want to know as soon as possible if you have both. Early diagnosis and treatment of PsA can help prevent permanent damage to your joints.
Read Also: Is Mushroom Good For Rheumatoid Arthritis
Read Also: What Is The Best Painkiller For Rheumatoid Arthritis
What Is Muscle Pain
Muscle pain, myalgia, is described as an ache, a dull feeling of pain in the muscles. It may involve different groups of muscles like the upper part of the arms or thighs or the upper and lower groups of muscles in the arms and legs. Muscle pain can also lead to weakness. Patients can describe difficulties combing their hair, still in a pot, or getting out of the chair.
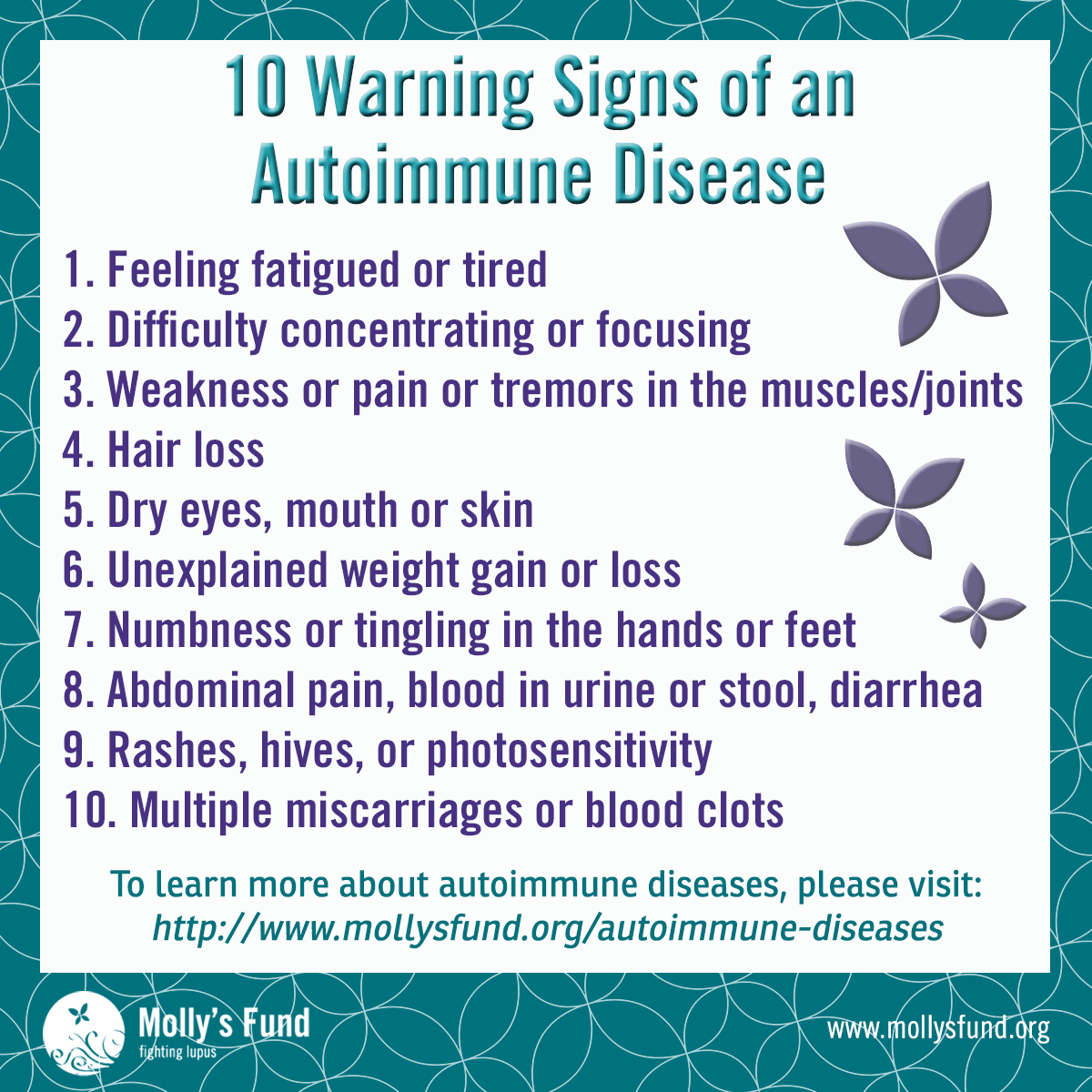
Symptoms Of Autoimmune Diseases
Most autoimmune diseases cause inflammation, which produces redness, heat, pain, and swelling.
Many autoimmune diseases affect more than one part of the body. The symptoms you have will depend on the body part affected, such as:
- Joints, which can cause joint pain, stiffness, and loss of function.
- Thyroid, which might cause you to be tired, gain weight, or have muscle aches.
- Skin, which can cause rashes, blisters, and color changes.
Read Also: Are Weighted Blankets Good For Arthritis
How Is Osteoarthritis Diagnosed
The physician will begin with a complete medical history and a physical examination. During the exam, the doctor will look for an enlarged or bumpy joint, signs of swelling, or decreased range of motion. Your doctor may then order x-rays, which can show a decrease in the cartilage space, new bone formation, or incorrect alignment. In some cases, your doctor may perform an aspiration the removal of fluid from a swollen joint or bursa to exclude infection, gout, or rheumatoid arthritis as possible causes of your joint pain.
What Are The Treatments
Medicine and lifestyle changes can often control symptoms and slow these diseases.
Medication. Many drugs can now treat RA and other autoimmune disorders. Some are used for pain relief. Others target inflammation. Early treatment with drugs like these may be the best way to prevent joint damage. See your doctor to talk about your options.
Lifestyle choices. While you canât change your genes, you can sometimes change how you live. That can help your treatment work better.
Even if you donât have an autoimmune disease, but you think you might be at risk, these steps may help lower your chances.
You May Like: What Food To Eat When You Have Arthritis
Rheumatoid Arthritis And Osteoarthritis
Rheumatoid arthritis and osteoarthritis are both types of arthritis. Both require medication that can help the disease, but the medication have side effects such as affecting the heart, kidney, lungs, and the skin. Neither rheumatoid arthritis and osteoarthritis have any known cures. According to the website healthline.com, Both types of arthritis are more common in women than men. Osteoarthritis and Rheumatoid arthritis are more prevalent in older adults, but RA can develop at any age. Rheumatoid
Is Reiters The Same As Reactive Arthritis
Reactive arthritis, also called Reiters syndrome, is the most common type of inflammatory polyarthritis in young men. It is sometimes the first manifestation of human immunodeficiency virus infection. An HLA-B27 genotype is a predisposing factor in over two thirds of patients with reactive arthritis.
Also Check: Is Krill Oil Good For Rheumatoid Arthritis
Whats The Age Of Onset For Rheumatoid Arthritis
RA usually starts to develop between the ages of 30 and 60. But anyone can develop rheumatoid arthritis. In children and young adults usually between the ages of 16 and 40 its called young-onset rheumatoid arthritis . In people who develop symptoms after they turn 60, its called later-onset rheumatoid arthritis .
Work And Psoriatic Arthritis
Having psoriatic arthritis may make some aspects of working life more challenging. But, if youre on the right treatment, its certainly possible to continue working.
Help and support is available, and you have rights and options.
The Government scheme Access to Work is a grant that can pay for equipment to help you with activities such as answering the phone, going to meetings, and getting to and from work.
The 2010 Equality Act, and the Disability Discrimination Act in Northern Ireland makes it unlawful for employers to treat anyone with a disability less favourably than anyone else.
Psoriatic arthritis can be classed as a disability if it:
- makes daily tasks difficult
- lasts for more than 12 months.
Your employer may need to make adjustments to your working environment, so you can do your job comfortably and safely.
You might be able to change some aspects of your job or working arrangements, or train for a different role.
In order to get the support youre entitled to, youll need to tell your employer about your condition. Your manager or HR department might be a good place to start.
Other available support might include:
- your workplace occupational health department, if there is one
- an occupational therapist. You could be referred to one by your GP or you could see one privately
- disability employment advisors, or other staff, at your local JobCentre Plus
- a Citizens Advice bureau particularly if you feel youre not getting the support youre entitled to.
You May Like: What Foods To Eat To Help Arthritis
What Are The Symptoms Of Inflammatory Arthritis
The most common symptoms of inflammatory arthritis are:
- Joint pain and stiffness after periods of rest or inactivity, particularly in the morning
- Swelling, redness and/or a feeling of warmth in the affected joints
- Inflammation of other areas in the body, such as the skin or internal organs like the lungs and heart
People with inflammatory arthritis generally experience alternating periods of flares of highly intense symptoms with periods of inactivity.
How Is Ra Treated
RA can be effectively treated and managed with medication and self-management strategies. Treatment for RA usually includes the use of medications that slow disease and prevent joint deformity, called disease-modifying antirheumatic drugs biological response modifiers are medications that are an effective second-line treatment. In addition to medications, people can manage their RA with self-management strategies proven to reduce pain and disability, allowing them to pursue the activities important to them. People with RA can relieve pain and improve joint function by learning to use five simple and effective arthritis management strategies.
Don’t Miss: How Do You Permanently Treat Rheumatoid Arthritis
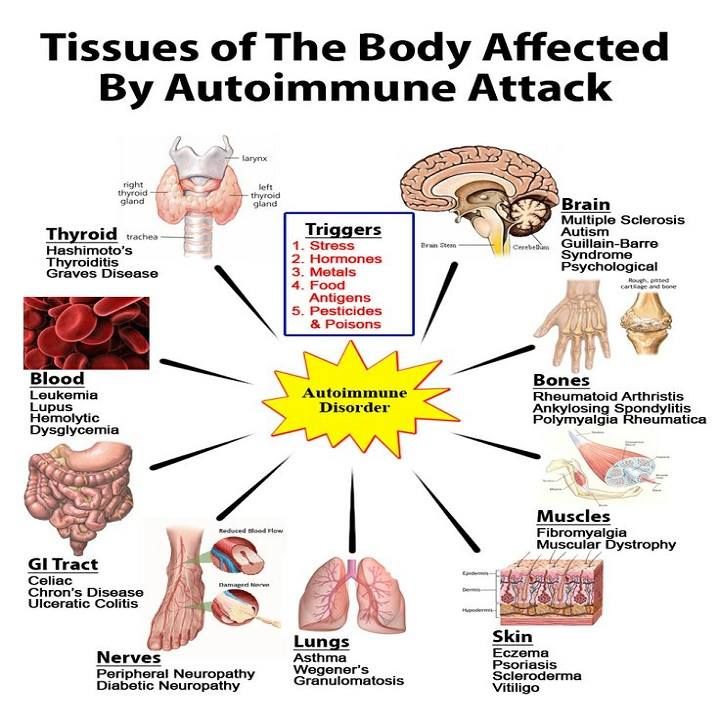
What Causes Autoimmune Diseases
No one is sure why autoimmune diseases happen. But you can’t catch them from other people.
Autoimmune diseases do tend to run in families, which means that certain genes may make some people more likely to develop a problem. Viruses, certain chemicals, and other things in the environment may trigger an autoimmune disease if you already have the genes for it.
About International Foundation For Autoimmune Arthritis
The International Foundation for Autoimmune Arthritis, formerly known as the International Autoimmune Arthritis Movement, is a 501 organization, committed to eliminating the adversity caused by autoimmune arthritis by uniting resources that will raise global awareness, providing wellness education and support, and promoting patient-centered research that will improve the quality of life for those affected by these diseases. The term autoimmune arthritis refers to a group of conditions in which the primary joint disorder has an autoimmune component. Due to the inflammatory nature of these conditions, they also may affect the connective tissues, soft tissues and organs.
Recommended Reading: What Is Good For Arthritis In Your Knees
Polymyalgia Rheumatica Vs Rheumatoid Arthritis
This autoimmune disease is challenging to diagnose for two reasons. First, its symptoms overlap with many other inflammatory and autoimmune conditions. Second, it can cause a variety of symptoms, and an individual may experience just a few symptoms that are not considered typical to the disease.
How is it similar to RA? Polymyalgia rheumatica joint pain is often symmetrical 1Clifford A and Hoffman GS. Polymyalgia Rheumatica and Giant Cell Arteritis. Cleveland Clinic. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/rheumatology/polymyalgia-rheumatica-and-giant-cell-arteritis/#bib6. Published June 2014. Accessed March 24, 2016. and most noticeable after getting out of bed in the morning. In one study, researchers found inflammation of joints lininga condition called synovitis, a classic sign of RAin 23% of polymyalgia rheumatica cases.2Cutolo M, Cimmino A, Sulli A. Polymyalgia rheumatica vs late-onset rheumatoid arthritis. Rheumatology 48 : 93-95. http://rheumatology.oxfordjournals.org/content/48/2/93.full. Accessed March 24, 2016.
People with polymyalgia rheumatica also may feel like they have the flu, have a fever, feel weak, or experience weight loss.
See Rheumatoid Arthritis Treatment
Is Psoriasis Arthritis An Autoimmune Disease
NYU Langone specialists are experienced in diagnosing and managing psoriatic arthritis, which is considered an autoimmune disease. This means that the immune system mistakenly attacks healthy tissues in the body. In psoriatic arthritis, the immune system attacks the joints, the spine, and the places where tendons attach muscles to bones.
Psoriatic arthritis affects about 30% of people who have psoriasis, an autoimmune condition that affects the skin.
Psoriatic arthritis is a common complication of psoriasis, affecting almost one third of people who have this autoimmune disorder. If you have PsA, your symptoms are more like rheumatoid arthritis which is another autoimmune disorder rather than osteoarthritis , which is a wear-and-tear disease.
Role of interleukin-12 in psoriasis decoded Psoriasis is a chronic inflammatory autoimmune disease.
of chronic inflammatory bowel diseases and psoriatic arthritis, says Burkhard Becher.
30 aug. 2019.
Psoriasis is an autoimmune skin disorder characterized by red patches covered with thick silvery scales. The most common form of psoriasis is.
PsA is an autoimmune disease, meaning it occurs when the bodys immune system mistakenly attacks healthy tissue, in this case the joints and skin. The faulty.
Enthesitis-related arthritis and a family history of autoimmune disease are key risk factors.
with anti-TNF-alpha and the paradoxical psoriasis in RA treated with anti-TNF-alpha may have.
6 aug. 2021.
Also Check: How Do X Rays Show Arthritis
You May Like: What To Use For Arthritis Knee Pain
What Are The Treatments For Autoimmune Diseases
The treatment depends on the disease. In most cases, the goal of treatment is to suppress your immune system, and ease swelling, redness, and pain from inflammation. Your doctor may give you corticosteroids or other medicines to help you feel better. For some diseases, you may need treatment for the rest of your life.
What Is The Difference Between Osteoarthritis And Inflammatory Arthritis
The major distinction between OA and IA is that:
- Osteoarthritis is caused by physical use wear and tear of a joint over time .
- Inflammatory arthritis is a chronic autoimmune disease in which your immune system misidentifies your own body tissues as harmful germs or pathogens and attacks them. The result is inflammation of the affected tissues in and around joints.
Because OA involves physical wear on joints in the body, it usually appears in people after the age of 50. The older you get, the more likely you are to get osteoarthritis.
Since inflammatory arthritis is a chronic disease, it affects people of all ages, often striking people in their peak working and child-rearing age. IA diseases can often be diagnosed in patients as young as age 20 or 30. Less commonly, kids and teens may be diagnosed with a form of childhood arthritis, such as . IA is more common in females than in males, and it is not understood why.
Recommended Reading: What Do You Do If You Have Arthritis
Ethical Issues Concerning Personalized Prevention
Obvious ethical concerns exist for any type of effort toward personalized prevention. One concern, valid for all studies, observational or interventional, relates to effects, psychological, and/or legal that may occur from notifying an individual that he/she is a high risk for acquiring a serious disease with as yet limited capacity for prevention. Another concern is the risk associated with testing of a drug with potential side-effects in individuals where development of future disease is substantially lower than 100%. The opportunity to prevent disease by modifying environment or lifestyle, addresses to some extent the first concern. The opportunity to treat symptoms, such as arthralgia and bone loss, that may exist in the âpre-RAâ phase with the same therapy as is aimed to prevent arthritis may address the second concern. The main argument, however, remains the wins that may follow from any successful prevention strategy that can be based on the science that requires the contribution from individuals at risk for disease.
What Are The Four Stages Of Rheumatoid Arthritis
The American College of Rheumatology has developed a system for classifying rheumatoid arthritis that is primarily based upon the X-ray appearance of the joints. This system helps medical professionals classify the severity of your rheumatoid arthritis with respect to cartilage, ligaments, and bone. The system defines the four stages of RA as follows:
Stage I
- No damage was seen on X-rays, although there may be signs of bone thinning
Stage II
Foods to avoid with RA
There is no special RA diet or dietcure for rheumatoid arthritis. However, it is thought that a healthy diet is an important complement to medication in the treatment of rheumatoid arthritis. Research is suggesting that the different kinds of bacteria in our intestines has a big impact on rheumatoid arthritis. Diet is likely important, but we do not know of specific foods or food groups that should be universally avoided by individuals with rheumatoid arthritis.
Diets higher in fish, grains, and vegetables decrease the risk of developing RA. The Western diet, defined as including more processed meats, increases the risk. It is not certain whether this is because of a direct anti-inflammatory effect of the fish, grains, and vegetables or because of changes in the natural bacteria in the gut.
Foods that fight RA inflammation
Supplements for RA
Exercises and home remedies for RA
Recommended Reading: What’s The Worst Arthritis You Can Have
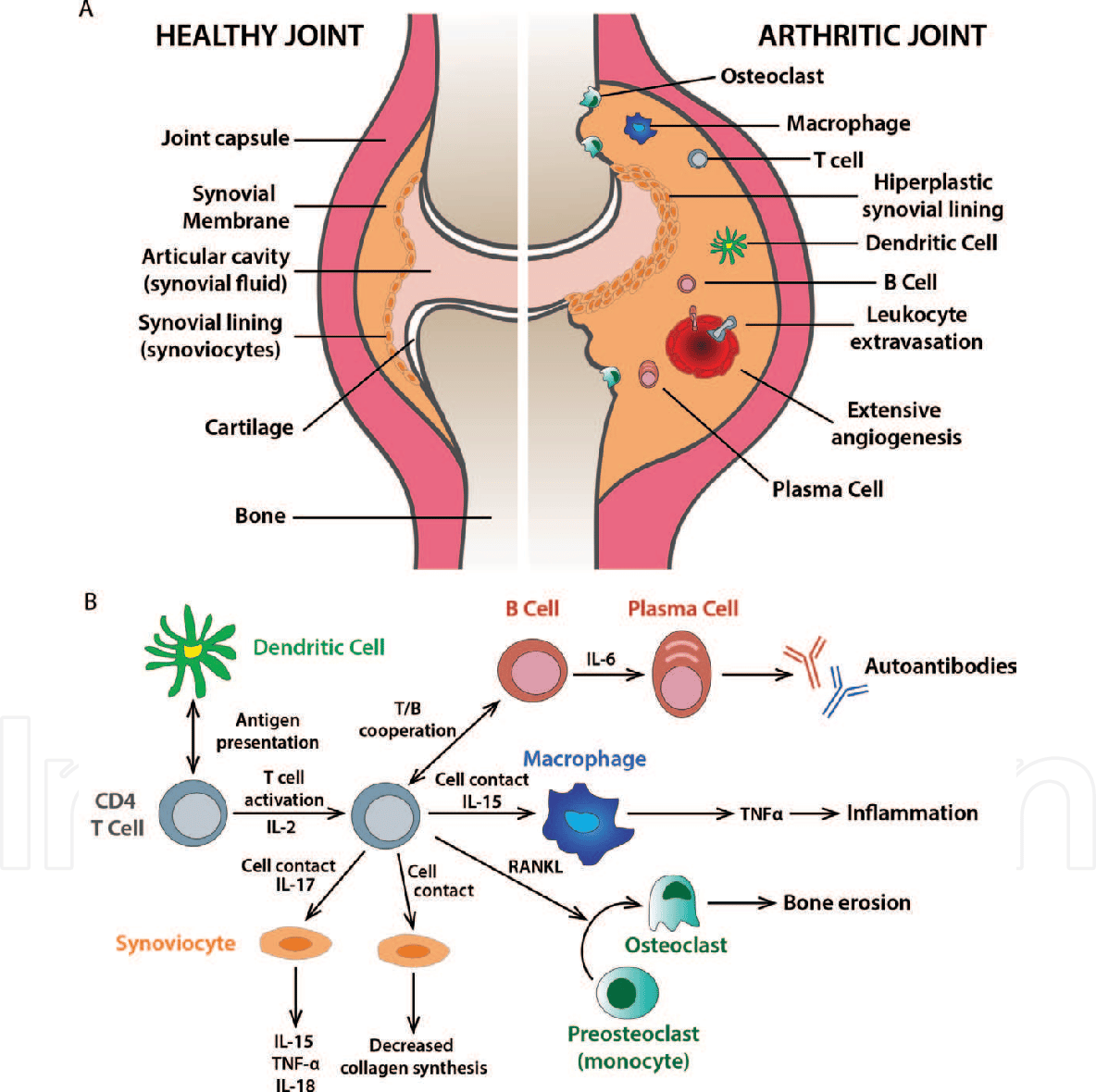
Amplification In The Synovium
Once the generalized abnormal immune response has become established which may take several years before any symptoms occur plasma cells derived from B lymphocytes produce rheumatoid factors and ACPA of the IgG and IgM classes in large quantities. These activate macrophages through Fc receptor and complement binding, which is part of the intense inflammation in RA. Binding of an autoreactive antibody to the Fc receptors is mediated through the antibodys N-glycans, which are altered to promote inflammation in people with RA.
This contributes to local inflammation in a joint, specifically the synovium with edema, vasodilation and entry of activated T-cells, mainly CD4 in microscopically nodular aggregates and CD8 in microscopically diffuse infiltrates. Synovial macrophages and dendritic cells function as antigen-presenting cells by expressing MHC class II molecules, which establishes the immune reaction in the tissue.
Can You Have Both Fibromyalgia And Chronic Fatigue Syndrome
Overview: Chronic Fatigue Syndrome and fibromyalgia are now widely recognized as real illnesses, not psychological problems. Diagnostic criteria have been established for both and a diagnosis of either condition qualifies a person to receive disability payments. Both CFS and fibromyalgia are common.
You May Like: Which Treatment Is Best For Rheumatoid Arthritis
Vitamin D And Fish Oil Supplements May Reduce Risk Of Autoimmune Disease Rheumatoid Arthritis Psoriasis And Thyroid
With a more pronounced effect after two years of supplementation.
Taking daily vitamin D supplements or a combination of vitamin D and omega-3 fish oil appears to carry a lower risk of developing autoimmune disease, with a more pronounced effect after two years, finds a trial of older US adults published by The BMJ today .
The researchers say the clinical importance of these findings is high, given that these are well-tolerated, non-toxic supplements, and that there are no other known effective therapies to reduce rates of autoimmune diseases.
Autoimmune disease happens when the bodys natural defense system mistakenly attacks normal cells. Common conditions include rheumatoid arthritis, psoriasis, and thyroid diseases, which increase with age, particularly among women.
Both vitamin D and omega-3 fatty acids derived from seafood are known to have a beneficial effect on inflammation and immunity, but no large randomized trials have tested whether these supplements can lower the risk of autoimmune disease.
So researchers set out to test the effects of vitamin D and omega-3 fish oil supplements on rates of autoimmune diseases in 25,871 US adults .
When they joined the trial, participants provided information on their age, ethnicity, region of residence, income, education, lifestyle, weight, medical history, diet, and supplement use. Blood levels of vitamin D and omega-3 fatty acids were also measured.
Recommended Reading: Mayo Clinic Arthritis Treatment