Rheumatoid Arthritis And Osteoarthritis
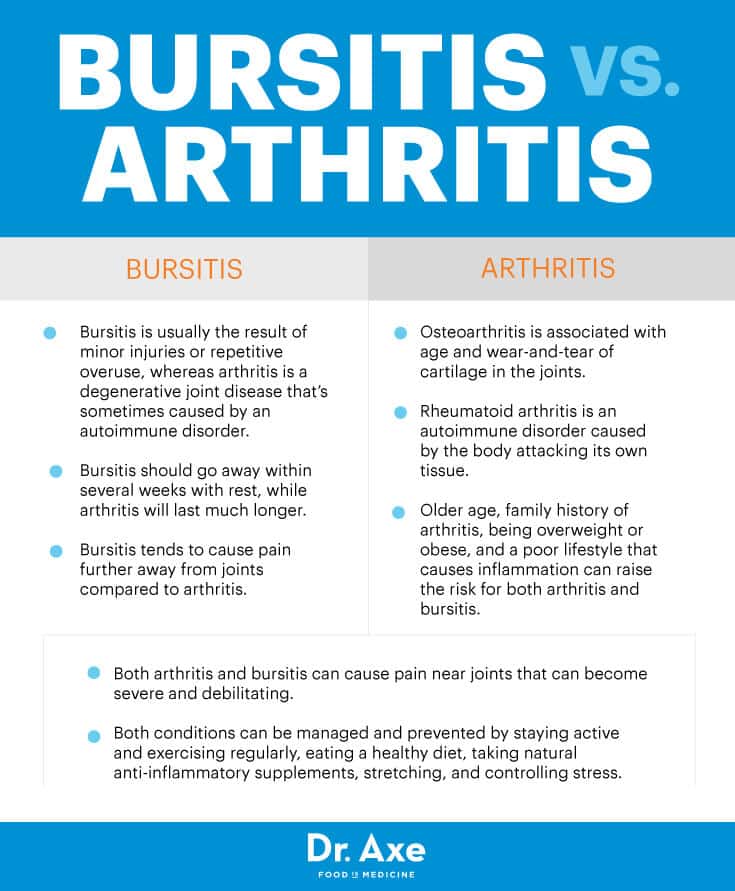
The word arthritis simply means inflammation of the joint. The reasons for that inflammation, however, varies. In the case of osteoarthritis, the cause is wear and tear. RA is an auto-immune condition, meaning that the immune system, normally there to protect us, is attacking healthy the joints.
Until I was diagnosed, I thought that arthritis was just something that old people get.
Until you or someone close to you is diagnosed with rheumatoid arthritis , unfortunately, this is most peoples perception of the disease. This is, at least in part, because many people, including some healthcare professionals, still refer to osteoarthritis as arthritis. So whats the difference?
One third of people over the age of 45 in the UK have sought treatment for osteoarthritis, whereas RA affects a much smaller number, at around 1% of the UK population.
There are also differences between the joints affected by these two conditions. Rheumatoid arthritis tends to affect joints symmetrically, most commonly the small joints of the hands and feet. Multiple joints may be affected, sometimes simultaneously, whereas OA will be isolated to individual joints. Osteoarthritis can affect the lower parts of the spine, and the finger joints closest to the nailbeds, both of which are areas of the body rarely affected in RA. RA can affect different joints at different times, whereas osteoarthritis doesnt come and go, although pain and stiffness can come and go.
What Is The Most Painful Type Of Arthritis
In general, rheumatoid arthritis is more painful than osteoarthritis. RA is more painful for a few reasons including the fact that it presents more symptoms, affects more joints simultaneously and often lasts longer throughout the day.
The most common symptoms of both RA and OA include painful, stiff joints, limited range of motion, warmth and tenderness in affected joints and more intense pain in the morning. However, RA presents additional symptoms apart from OA including fevers, muscle aches and excessive fatigue.
These additional symptoms suggest that RA is more painful since you’re experiencing more overall discomfort.
RA also affects more joints than the average case of OA. Since RA is an autoimmune disease that attacks the cells that make up your joints, it often begins in your smaller joints and eventually begins to effects all of the joints of your body.
On the other hand, OA tends only to affect a few isolated joints that are overused or injured. While OA can certainly progress to affect most of your joints, especially as you age, it’s estimated that RA is more painful overall since most of your joints will be affected.
And lastly, although both RA and OA symptoms are more intense in the morning before your joints get a chance to loosen up, OA symptoms tend to improve within 30 minutes whereas RA symptoms tend to take longer to feel better. This is a third reason why it’s assumed that RA is more painful than OA.
What Are The Complications Of Ra
Rheumatoid arthritis has many physical and social consequences and can lower quality of life. It can cause pain, disability, and premature death.
- Premature heart disease. People with RA are also at a higher risk for developing other chronic diseases such as heart disease and diabetes. To prevent people with RA from developing heart disease, treatment of RA also focuses on reducing heart disease risk factors. For example, doctors will advise patients with RA to stop smoking and lose weight.
- Obesity. People with RA who are obese have an increased risk of developing heart disease risk factors such as high blood pressure and high cholesterol. Being obese also increases risk of developing chronic conditions such as heart disease and diabetes. Finally, people with RA who are obese experience fewer benefits from their medical treatment compared with those with RA who are not obese.
- Employment. RA can make work difficult. Adults with RA are less likely to be employed than those who do not have RA. As the disease gets worse, many people with RA find they cannot do as much as they used to. Work loss among people with RA is highest among people whose jobs are physically demanding. Work loss is lower among those in jobs with few physical demands, or in jobs where they have influence over the job pace and activities.
Don’t Miss: How To Tell What Type Of Arthritis You Have
What Causes Rheumatoid Arthritis
The specific causes of rheumatoid arthritis have yet to be identified. This is true despite decades of medical research.
However, while we dont know specifically what brings about RA and the symptoms it is known to create such as joint pain, stiffness, fatigue, and low-grade fever we do know that it is the result of an autoimmune disorder which ultimately affects the joints.
In fact, oftentimes the pain in the joints is so severe that the people suffering from RA are advised to take a nonsteroidal anti-inflammatory drug such as aspirin, ibuprofen, or naproxen or some other type of anti-rheumatic drug to help ease the pain in the joints created by RA.
Whats the connection between RA and the joints? Specifically, how does this disease impact the joints in the human body, creating pain as a primary symptom?
Also Check: What Is The Best Home Remedy For Rheumatoid Arthritis
Possible Additional Arthritis Symptoms

RA Fever, fatigue, hot rash, or joint swelling may occur. With RA, there is systemic inflammation. The eyes, lungs, and heart or circulatory system can also be affected by this inflammation, as well as the mouth and the skin with rheumatoid nodules. Patients with RA generally have a team of physicians to oversee their treatment of all this different systemic involvement.
RELATED: Rheumatoid Arthritis and You: What RA Can Do to All Parts of Your Body
OA The symptoms are focused on the specific joint that are involved. Pain can be achy or sharp in nature and there may be radiating pain. OA symptoms can vary greatly among patients.
OA can make movement and exercise difficult at times. However, those are the exact things that are needed to assist with OA. If one does not exercise, that can contribute to obesity, which in turn contributes to load, systemic factors, and pain at various levels. The association between obesity and pain is well established, including its bidirectional nature, according to a study published in the April 1, 2021, issue of Osteoarthritis and Cartilage. According to the Arthritis Foundation, losing 1 pound of weight resulted in 4 pounds of pressure being removed from the knees. In other words, losing just 10 pounds would relieve 40 pounds of pressure from your knees.
You May Like: What Supplements Are Best For Rheumatoid Arthritis
Statement Of Literature Search
For the development of this narrative review, publications were identified by a series of searches on PubMed between September 2020 and July 2021. Search terms included AND AND AND AND . Publications that detailed the characteristic clinical manifestations, comorbidities, pathogenesis, biomarkers, treatment recommendations, and differential diagnosis for PsA, RA, and OA were included. References that were determined to be irrelevant on the basis of the authors judgment were excluded from consideration. Relevant references that were cited within the publications included in this review and articles previously known by authors were considered on the basis of the criteria. This review is based on studies that were previously completed and does not contain any novel studies with human participants that were conducted by any of the authors.
Dont Suffer From Back Pain Alone: Treatments For Ra
If you have debilitating back pain, you should consult with a physician to rule out any other causes. However, if RA is the source of your pain, you may be able to alleviate it through treatment. If you have RA back pain, you may want to consider taking home medications and physical therapy. In addition to your RA, you may also be suffering from sciatica it is important to seek medical attention if you find yourself in this situation.
Recommended Reading: How Does Rheumatoid Arthritis Affect The Immune System
Accommodations And Medical Leave
Under the Americans with Disabilities Act and the Family Medical Leave Act , there are certain job protections people with RA might have.
Under the ADA, you may be able to ask for reasonable workplace accommodations that make it easier to do your job. These accommodations need to be essential for performing the job in the same manner as a person without a disability.
This may include things like an ergonomic keyboard or desk chair, a sit-stand desk, extra breaks to stretch, talk-to-type software for your computer, or a modified work schedule. Of course, accommodations must be reasonable and should not cause undue hardship to the employer.
Under FMLA, people with RA and other chronic illnesses can take up to three months of unpaid leave per year if they are unable to work due to their health. This leave doesnt have to been taken all at once and can be intermittent as needed for short periods.
For example, a person with rheumatoid arthritis may take intermittent leave for two or three days to manage a disease flare-up. Intermittent leave can also be used for medical appointments or appointments for treatments related to RA.
Your employers human relations department is the best position to explain how ADA accommodations work and your intermittent leave options under FMLA.
You May Like: Are Dates Good For Rheumatoid Arthritis
What Benefits Can I Claim With Rheumatoid Arthritis
If the SSA determines that you are eligible for benefits, they will add you to a payment program.
The amount payable will depend on individual factors such as your work history, your age, and the date of your disabilitys onset.
Certain members of your family may also be eligible to receive benefits without the need for work credits. This can include paying benefits to your spouse, children, or dependent parents.
Additional benefits may be available depending on your individual circumstances or if you are able to return to work. These can include any expenses incurred to assist you at work, health insurance with Medicare, and financial support when returning to work.
Benefits from SSI may also be payable in addition to any other federal benefits you receive.
Find a complete overview of available employment supports with the SSA here.
Also Check: Does Ice Help Arthritis Pain
What Tests Rule Out Rheumatoid Arthritis
X-rays may be recommended by your doctor to help track the progression of rheumatoid arthritis over time in your joints. Magnetic resonance imaging and ultrasound can be used by your doctor to determine the severity of the disease in your body.
What Is Seronegative Rheumatoid Arthritis?
Although the condition of having no form of rheumatoid arthritis is considered normal, the condition of having no form of rheumatoid arthritis is considered severe. Even if their blood tests show no signs of rheumatoid factor or CCP, there are some obvious symptoms of seronegative arthritis.
What Are The Markers For Rheumatoid Arthritis
In patients with RA, there are several clinically useful markers, in addition to rheumatoid factors , anti-cyclic citrullinated peptide antibodies, erythrocyte sedimentation rate , and C-reactive protein .
The Seriousness Of Ra Cannot Be Understated
It can cause a variety of side effects, including intense joint pain and general pain throughout the body. When your RA flares, you may feel pressure, burning, or sharp pains. When people with RA feel few to no symptoms, they may experience periods of remission. RA can affect the entire body, causing fatigue, poor joint function, and breathing issues. If you are experiencing significant pain or discomfort while wearing your RA mask, you should see a doctor as a condition that requires ongoing treatment.
Don’t Miss: How Long Does An Arthritis Flare Up Last
Is Rheumatism The Same As Rheumatoid Arthritis
As youre realizing by now, while these two terms are often lumped together, they shouldn’t be. RA is just one of many rheumatologic diseases, historically referred to as rheumatism. RA is an autoimmune inflammatory condition that causes pain and swelling in the joints and fever, fatigue, and brain fog. The condition can be marked by flaresincreased disease activity after a period of low or no symptoms.
Other Conditions And Joint Pain
Other forms of arthritis, and other conditions, can also cause joint pain. Examples include:
- fibromyalgia syndrome, a condition in which your brain processes pain in your muscles and joints in a way that amplifies your perception of the pain
- scleroderma, an autoimmune condition in which inflammation and hardening in your skin connective tissues can lead to organ damage and joint pain
Read Also: What Helps With Arthritis In The Fingers
Treatment Of Oa And Ra
How Osteoarthritis is Treated
Unfortunately, osteoarthritis cannot be reversed or treated. We offer various treatments and pain relievers to help patients with OA manage unpleasant symptoms.
- Intra-articular injections: Injections of corticosteroids, hyaluronic acid, BOTOX® or platelet-rich plasma in the joints can help to relieve pain in the joints. These injections can provide the missing cushion or padding that the cartilage once provided before it degenerated.
- Physical therapy: Because OA weakens the joints and muscles, physical therapy can help to strengthen the affected joints. Similarly, pain management classes can help patients to minimize the symptoms of OA.
- Pain-relieving medications: Various medications can be taken to relieve the symptoms of OA, dull the pain and discomfort, and reduce swelling. These medications include Tylenol® and NSAIDs .
How Rheumatoid Arthritis is Treated
There is unfortunately no treatment to reverse rheumatoid arthritis either. We can provide various medications along with therapy to help patients manage the symptoms of RA.
- Disease-modifying medications: Various medications, known as DMARDs , can be taken to either slow the progression of RA or stop the progression entirely. These treatments can save the joints from further damage.
The Difference Between Rheumatoid Arthritis And A Herniated Disc
There are many possible causes of the pain in your joints and back, and it can be difficult to determine the source without a professional evaluation. However, two of the most common possibilities are rheumatoid arthritis and a herniated disc. Both conditions can cause similar symptoms, so how can you tell the difference?
At Johns Hopkins Arthritis Center, we are dedicated to providing excellent education to both patients and healthcare providers. It is part of the Johns Hopkins Health System, and it was established in 1998. RA and a herniation may be present in your discs. You are fortunate to have a physician who can provide you with an accurate picture of the mind of the person he saw you with.
The cervical region , which is located near the joints, is another area that can be affected by rheumatoid arthritis. Because Rheumatoid arthritis of the spine does not result from wear and tear, it is classified as inflammatory arthritis.
You May Like: What Helps Lower Back Arthritis
Risk Factors For Rheumatoid Arthritis And What You Can Do About Them
You can take measures to help prevent this autoimmune disease. Heres what you need to know.
RA Risk Factors You Cant Control
- Age. Conventional wisdom has it that the chance of RA increases with age. But experts say RA that develops after age 60 called late-onset RA is different from RA in younger people. Also, the risk as you get older may not be as great as originally thought current research shows that RA antibodies develop many years before symptoms appear.
- Biological sex. RA is far more common in people born female than those born male. The disparity is often blamed on hormones, mainly because RA can get better or worse as hormones shift. Yet studies about the relationship between RA and sex hormones show mixed results. Newer theories focus on womens more robust immune response to infections, which generates more antibodies, and on differences in the innate immune system.
- Your genes. Hundreds of gene variants, especially a genetic marker called the shared epitope, are associated with RA, but their exact role isnt clear. Many people who have these gene variants never develop RA, while others who dont have them get arthritis or other autoimmune diseases. Genes may influence the progression of RA or response to treatment, but by themselves arent enough to cause disease.
Environmental Risk FactorsLifestyle Risk Factors
Get Involved
- 1355 Peachtree St NE Suite 600
- Atlanta, GA 30309
Affected Joints In Ra
RA usually begins in the smaller joints. Youre likely to have pain, stiffness, and swelling in the finger joints. As RA progresses, symptoms can develop in larger joints such as knees, shoulders, and ankles.
RA is a symmetrical disease. That means youll experience symptoms on both sides of your body at the same time.
Also Check: How To Stop Arthritis Flare Ups
Differences Between Osteoarthritis And Rheumatoid Arthritis
Arthritis is the inflammation of joints. It is not a single disease. There are over 100 types of arthritis. Some similar symptoms of arthritis in general include joint stiffness and joint pain. These symptoms make it difficult to move around and perform everyday tasks. Lets take a look at the two most common types of arthritis, their differences, and how arthritis doctors treat them.
Can You Tell Which Condition You Have
Joint swelling in arthritis may also cause compression of the nerves in the hand or wrist, which can then cause numbness, tingling, and pain. Your healthcare provider will perform a few specific tests to pinpoint the problem.
- Reduced muscle mass in the fleshy part of the hand at the base of the thumb
- A positive Tinel’s Sign, or a burning or tingling sensation when the median nerve is tapped lightly
- A positive Phalen’s sign, a test that assesses for pain when your arms are held vertically and your wrists are flexed 90 degrees for 60 seconds
- Weakness or poor dexterity with pinching movements
- Pain that is worse at night or wakes your from your sleep
- Asymmetric patterns of joint involvement
- Swelling of other joints outside of the hands and wrists
- Systemic involvement with inflammatory arthritis, including fevers, malaise, or rash
- Antibodies or inflammatory markers present in blood testing
- Pain that goes away after a few hours in the morning
Also Check: What Does Tylenol Arthritis Look Like