Treatment Plans For Seronegative Ra
Treatment for seronegative RA is generally the same as seropositive RA, the goal being to relieve pain and slow progression of the disease through:
-
Ibuprofin and other nonsteroidal anti-inflammatory drugs to decrease inflammation
-
Physical therapy and other exercise to help with joint mobility and range of motion
-
Methotrexate and other disease-modifying antirheumatic drugs when anti-inflammatory drugs are not enough
-
Steroidal injections into the joint to reduce inflammation
-
Injection or infusion in a doctors office of biologics, a subset of DMARD that slows the disease
-
JAK inhibitors, another DMARD that blocks the Janus kinase pathways involved in the body’s immune response
In addition to medication and , seronegative RA patients can find relief through:
-
Deep breathing, guided imagery, visualization and other relaxation methods to help train painful muscles to relax
-
Massage, and acupressure
-
Joint replacement surgery to replace severely damaged joints with metal or plastic parts. Hip and knee replacements are most common, but ankle, shoulder, wrist and elbow replacements allow RA patients to resume daily activities once curtailed by and stiffness.
For any diagnosis of RA, its important to work with your doctor to monitor your symptoms and adjust your treatment as necessary. With the right care plan, you can continue to live a full and healthy life with RA.
Family & Personal Medical History
The patients medical history and family history are important factors in helping to reach a RA diagnosis. Studies have shown that the average risk of someone in the general population developing RA is about 1%. However, if there is a family history of the disease, the risk of another family member developing RA increases.
When diagnosing RA doctors ask about the following:
- Patients family members who have or had RA
- Patients existing or past autoimmune disorders
- Patients family members with other autoimmune disorders
- Other medical conditions, illnesses or complications
Depending on each patients unique set of answers, it can help doctors identify factors that lead to a RA diagnosis.
What You Can Do
It leaves doubt in your mind and makes you feel like there has been a misdiagnosis, like maybe you have something curable. Amy
If you have problems getting diagnosed or treated due to negative blood tests, advocate for yourself. Ask your doctor to order both RF and anti-CCP tests. If negative, find information to show your doctor. Ask for a referral to a rheumatologist regardless of test results. If a rheumatologist wont diagnose without positive blood tests, get a second opinion.
Read Also: How To Ease Arthritis Pain In Fingers
Reaching A Ra Diagnosis
Once all of these steps have been conducted, doctors will look at all of the test results and reach a conclusion based on the overall picture. Some doctors take a more symptom based approach to diagnosing RA while others rely on blood tests and medical history to confirm a RA diagnosis.
This is why its possible to be diagnosed with RA but not test positive for antibodies or have a medical history of RA in your family. If the symptoms themselves are consistent with RA, then it can still be diagnosed.
That being said, the main criteria for diagnosing RA do not change. The patient must exhibit symptoms for greater than six weeks, symmetrical symptoms, as well as multiple joints being affected including fingers and hands.
Does This Affect The Medications That Will Work For Me
Whilst the efficacy of most medications for RA is not affected by whether someone is seropositive or seronegative, evidence suggests that patients who are seronegative for both RF and anti-CCP do not respond as well to rituximab as patients who are seropositive for one or both.
-
Rheumatoid arthritis is an auto-immune disease, meaning that the symptoms such as pain and inflammation are caused by the immune system attacking the joints.
Information
Also Check: Is Banana Good For Rheumatoid Arthritis
What Is Seropositive Rheumatoid Arthritis
Patients with a positive result for rheumatoid factor and/or anti-citrullinated peptides antibodies are called seropositive. Being seropositive means that the patient is prone to holds an antibody within their blood, causing an attack on joints and leading to inflammation. These patients can have severe joint deformities, disabilities, and inflammation outside of the joints.
Consequences Of Delay In Ra Diagnosis
It took years and years for me to be diagnosed. No doctor would listen to me. It progressed fast like a tornado. If someone had listened I probably wouldn’t be as bad. Susan
The best method of getting control of RA is by treating the condition early and aggressively. The longer the delay to diagnosis and treatment, the more difficult it may be to achieve remission and prevent damage to the joints.
Also Check: Stopping Arthritis Pain
Are Positive And Seronegative Ra Different
I was lucky to be taken seriously from the start. I went from 0 joints to ALL of them in a few weeks there was no mistaking it for normal or an injury. Rebecca
Current research indicates that seropositive RA tends to be more severe than the seronegative kind, leading to more joint damage. When someone has seropositive RA, family members may also be more likely to develop the condition. Both types appear to respond equally to medication. Of course, there are always exceptions to the trends.
People With Seronegative Ra Often Have Different Symptoms
The conventional wisdom is that seropositive patients have more severe symptoms, but recent studies suggest that the difference between the two forms of the disease may have more to do with the joints affected than with the severity of the RA symptoms. And a report published in June 2016 in BMC Musculoskeletal Disorders found that further research is needed to better understand the long-term outcomes of patients with seronegative RA. My experience has been that while the symptoms are similar, seronegative patients are more difficult to treat, says Vinicius Domingues, MD, a rheumatologist in Daytona Beach, Florida, and a medical adviser to CreakyJoints.
Recommended Reading: How You Get Arthritis
Other Conditions Associated With Seronegative Patients
A seronegative result along with what are thought to be rheumatoid arthritis symptoms could potentially indicate other conditions altogether. Often times when inflammation is present or consistent it means that the seronegative patient may have osteoarthritis instead of rheumatoid arthritis. This is a common confusion.
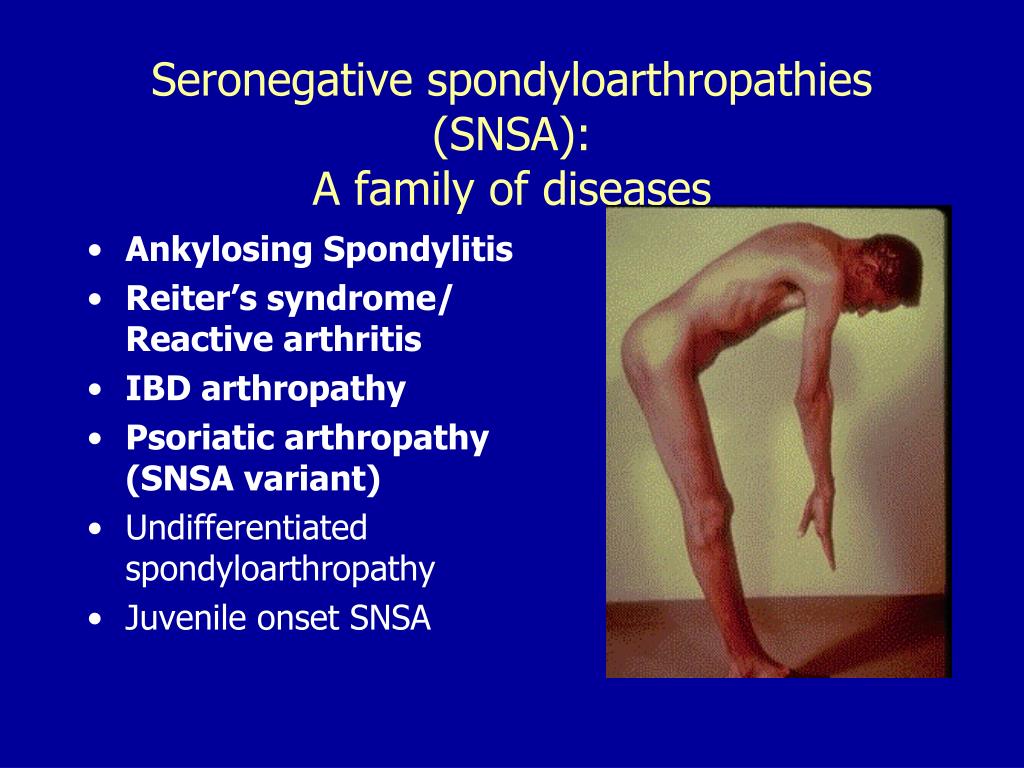
Spondyloarthritis conditions are sometimes associated with seronegative rheumatoid arthritis because they are inflammatory. These are conditions like ankylosing spondylitis, reactive arthritis, as well as psoriatic arthritis.
Delay In Accurate Information
Any time I see any doc other than my rheumatologist or GP I get treated as though my RA is all in my head. Darlyne
Unfortunately, the information that anti-CCP should be the basis for determining seronegative RA has not yet moved past beyond the field of rheumatology. If aware of the concept of seronegative RA, most doctors still understand this as being related to the RF test. In addition, many doctors dont know that it’s possible to have RA if the RF is negative.
Read Also: Are Bananas Good For Rheumatoid Arthritis
A Wide Variety Of Conditions Can Present As Inflammatory Arthritis
The other difficulty is the wide differential diagnosis of polyarthritis . A good history and physical examination combined with a few simple laboratory or radiological investigations should help in excluding most of the conditions that mimic RA. In our patients, the following need to be considered:
-
Postviral arthritisParvovirus arthritis should be considered, since she may have encountered the virus at her school. However, against this diagnosis are the duration of joint symptoms , the fact that she did not have fever, rash or sore throat and the negative parvovirus serology
-
Seronegative spondyloarthritisIn this condition one would expect features such as psoriasis, inflammatory bowel disease or inflammatory back pain and a family history of similar disorders. However, a small proportion of patients with psoriatic arthritis do get arthritis before skin lesions appear.
Box 2Conditions that can present as polyarthritis and mimic RA
Postviral arthritise.g. parvovirus, mumps, rubella, hepatitis B and C
Seronegative spondyloarthritise.g. psoriatic arthritis, inflammatory bowel disease
Connective tissue diseasese.g. systemic lupus erythematosus, scleroderma, vasculitis
Osteoarthritis
Crystal arthritise.g. polyarticular gout, pseudogout
Miscellaneouse.g. sarcoidosis, thyroid disease, infective endocarditis, malignant disease
Box 3Investigations that may help in diagnosing common underlying causes of polyarthritis
Use Of Random Peptide Library And Elisa Test

A dodecamer random peptide library was used to identify possible relevant autoantigens in seronegative RA. An IgG pool derived from the first cohort of 50 patients with seronegative RA was used to screen the peptide library, while a pool of IgGs from 25 healthy donors was used for the pre-screening step . Finally, a set of 17 putative peptides was used to evaluate the binding of individual patients sera
We also analyzed the sera of 25 seropositive RA patients and found that 64% of them recognized the RA-peptide . Statistically significant differences were found in the binding to RA-peptide between the seronegative RA patients and healthy donors sera or between the seropositive RA and healthy donors , but not between seronegative and seropositive patients .
The potential diagnostic value of anti-RA-peptide antibodies in either seronegative or seropositive RA patients was assessed by a receiver operating characteristic curve. The area below the ROC curve was 0.9244 between anti-peptide Abs of seronegative RA patients and healthy donors and 0.8840 between anti-peptide Abs of seropositive RA patients and healthy donors . No significant difference was found in ROC curve between the seronegative and seropositive RA .
In order to validate the binding specificity of RA-peptide, a second study sample of seronegative RA patients was analyzed, as well as a group of patients with other immune-mediated diseases,like SA, PsA, and SSc .
Also Check: Rheumatoid Arthritis Burning Pain
What Do The Test Results Mean
The presence of either of these tests may indicate that RA is present. However, seropositivity is only one criterion of several that makes the diagnosis of RA likely . If the other criteria for the diagnosis are present, then seropositivity is an additional clinching factor. A positive anti-CCP test is marginally stronger than positive RF test for the diagnosis.
Seronegative Ra: What Are The Symptoms Of Seronegative Ra
Seronegative rheumatoid arthritis is the diagnosis of rheumatoid arthritis without the presence of certain antibodies in the patients blood. It is one of two main types of rheumatoid arthritis diagnoses.
In most cases of rheumatoid arthritis, the patient tests positive for rheumatoid factor and/or anti-citrullinated peptides antibodies. These indicate that the patient is seropositive and that they possess the antibodies that cause an attack on joints and lead to inflammation. These patients tend to have a more severe disease course with more joint deformities, x-ray damage, disability and inflammation outside of the joints.
You May Like: Hand Inflammation Treatment
Rheumatoid Arthritis Can Be Both A Visible And Invisible Chronic Illness
There are a variety of experiences and hidden symptoms that may be experienced by people living with rheumatoid arthritis. Living with RA can sometimes feel like having a visible and invisible illness depending on the symptoms experienced at any given time. This has been hard to navigate and explain what Im going through when it impacts how I am able to show up in my relationships or different roles in my life.
Clinical Diagnosis Of Inflammatory Arthritis Is Not Always Straightforward
The history of swelling in joints, early morning stiffness lasting > 30 minutes, systemic symptoms such as tiredness combined with objective evidence of synovitis would favour a diagnosis of inflammatory arthritis . However, reality can be more complex:
-
Objective signs may be lacking or have been suppressed by anti-inflammatory medication
-
Joint swelling can be difficult to identify in obese patients
-
The sensation that joints are swollen may be reported even by some patients with fibromyalgia
-
Osteoarthritis as well as RA can cause morning stiffness, though in osteoarthritis it usually lasts less than 30 minutes
-
Inflammatory markers such as the ESR or C-reactive protein are normal in about 60% of patients with early RA
-
In a patient with preceding osteoarthritis, radiographic changes can be misleading, especially if those suggestive of inflammatory arthritis have not yet developed.
Read Also: Rheumatoid Arthritis And Lower Back Pain
Symptoms Of Seronegative Rheumatoid Arthritis
Seronegative rheumatoid arthritis patients must possess a distinct set of symptoms in order to be diagnosed. This is because the lack of antibodies in the blood makes it more difficult to reach a rheumatoid arthritis diagnosis.
Some of the most important symptoms in diagnosing seronegative rheumatoid arthritis include:
- Joint pain, stiffness specifically in the hands but also in knees, elbows, hips, feet and ankles
- Joint swelling and redness
- Morning stiffness lasting longer than 30 minutes
- Fatigue
- Eye redness
Though this is not an exhaustive list, the majority of these will support a rheumatoid arthritis diagnosis. If we compare these symptoms to seropositive rheumatoid arthritis symptoms, there are many similarities. However, many patients see these symptoms evolve and change over time.
It is thought that seropositive patients experience a more severe disease course than seronegative patients. But studies have also shown that in some patient cases, the progression is comparable and sometimes is there is little difference. This is where it becomes complicated in trying to classify rheumatoid arthritis into sub-types and to reach a solid diagnosis.
There are some symptoms that are thought to be rheumatoid arthritis in seronegative patients, but later turn out to be other conditions. These cases mainly involve differences in the types of joints and areas affected as well as the levels of inflammation.
The Rheumatoid Arthritis Diagnosis And Treatment Journey Can Be Different For Each Patient
For me, this was and continues to be the case because the symptoms, treatment, and complications connected to RA within my body interact with my other medical conditions, creating an overlap of symptoms and contradictions that can be hard to pull apart to gain clarity. Advocating for my rheumatologist, neurologist, and primary care physicians to be in communication with each other has been helpful, especially when things get complex and confusing beyond just me.
Don’t Miss: Ra Back Pain
How Being Seronegative Affects Ra
As with people who are seropositive, RA isnt predictable for those who are seronegative. But because it can be harder to diagnose seronegative RA, it can take longer to get treated for it. That delay might make it less likely that youll go into remission, which is when you have very few signs of the disease.
People who start treatment within the first 2 years of symptoms are more likely to go into remission than those who dont.
Seronegative Ra Is Sometimes Linked To Having Higher Levels Of Inflammation Than Seropositive
In a European study of 234 people who had both types of rheumatoid arthritis and had experienced symptoms for less than two years, those with seronegative RA showed higher levels of inflammation and more affected joints, according to research published in January 2017 in Annals of the Rheumatic Diseases.
Recommended Reading: How To Help Arthritis In Your Hands
Can Seropositive Change To Seronegative And Vice Versa
In the RA literature, viewpoints differ on the possibility of seroconversion, that is seronegative becoming positive or vice versa. Some indicate that seropositive can convert to negative during treatment, while reviews of studies seem to indicate that seroconversion from positive to negative is rare. Its also rare for someone who is seronegative to become positive.
The Presence Or Absence Of Rf Or Acpa Doesnt Make Or Break An Ra Diagnosis
Testing for rheumatoid factor in people suspected of having RA was popularized in the 1960s, and experts still dont fully understand the exact link between these factors and the development of the disease. RF can be positive in multiple diseases, such as hepatitis C, endocarditis, and multiple myeloma.
Rheumatoid factor clearly plays a role in how serious rheumatoid arthritis can be, says John J. Cush, MD, a professor of internal medicine and rheumatology at UT Southwestern Medical Center in Dallas. A different blood test checks for ACPA, which may be more closely linked to the development of the disease than RF. A study published in the journal Autoimmunity Reviews in July 2016 found that ACPA antibodies represent an independent risk factor for developing RA. Having ACPA suggests theres a genetic risk factor for the disease, but its not necessary for either antibody to be present in the blood for a diagnosis of seronegative RA.
RELATED:6 Things About Rheumatoid Arthritis That Are Difficult to Explain or Understand
Read Also: What Are Usually The First Signs Of Rheumatoid Arthritis
Does A Positive Rheumatoid Factor Or Anti
A positive RF or anti-CCP test does not mean that you have RA. Other features must be present such as symptoms of pain and swelling in the joints, involvement of many joints with inflammation, morning stiffness in the joints for longer than 45 min, x-ray evidence of the characteristic bone damage in the joints and extra-articular features of RA , such as nodules. Other blood tests commonly used prior to diagnosis include ESR and CRP, which measure the amount of inflammation in the joints. For more information on blood tests, please see our article: Laboratory tests used in the diagnosis and monitoring of rheumatoid arthritis.
All About Seronegative Rheumatoid Arthritis
What is it? When doctors diagnose rheumatoid arthritis, one of the things they do a blood test and look for whats called the rheumatoid factor and anti-CPP antibodies . Patients who test positive to these definitely have RA. However, some patients are full of the symptoms of RA but they test negative. This is called seronegative, and patients who test positive are called seropositive. This still means that a patient has RA, and being seronegative is not considered a separate type of arthritis .
How it differs from seropositive RA? Overall, it doesnt. I still have all the same symptoms that a seropositive patient does: chronic inflammation, morning stiffness, fatigue, joint pain, etc. In the past, doctors might believe that seronegative patients do not have a case as serious as someone who is seropositive, but that is no longer considered the case . What is especially interesting is that a 2016 study found that seronegative RA patients might in fact have higher inflammation levels than seropositive .
Additionally, some researches contend that a potential difference between seronegative and seropositive patients might be the joints affected . This refers to which joints are affected, so seropositive patients might have different affected joints than seronegative ones. Regardless, seronegative patients still need as aggressive treatments as seropositive ones.
Read Also: What Can I Take Over The Counter For Arthritis Pain