Impacts Of Psoriatic Arthritis In The Knees
PsA tends to be asymmetric, meaning different joints on either side of the body are affected . Symptoms in the knees can be mild and develop slowly or arise suddenly and severely. Arthritis usually follows the appearance of psoriasis on the skin. In addition to pain, swelling, and stiffness in the knee joints, PsA can lead to enthesitis and peripheral arthritis.
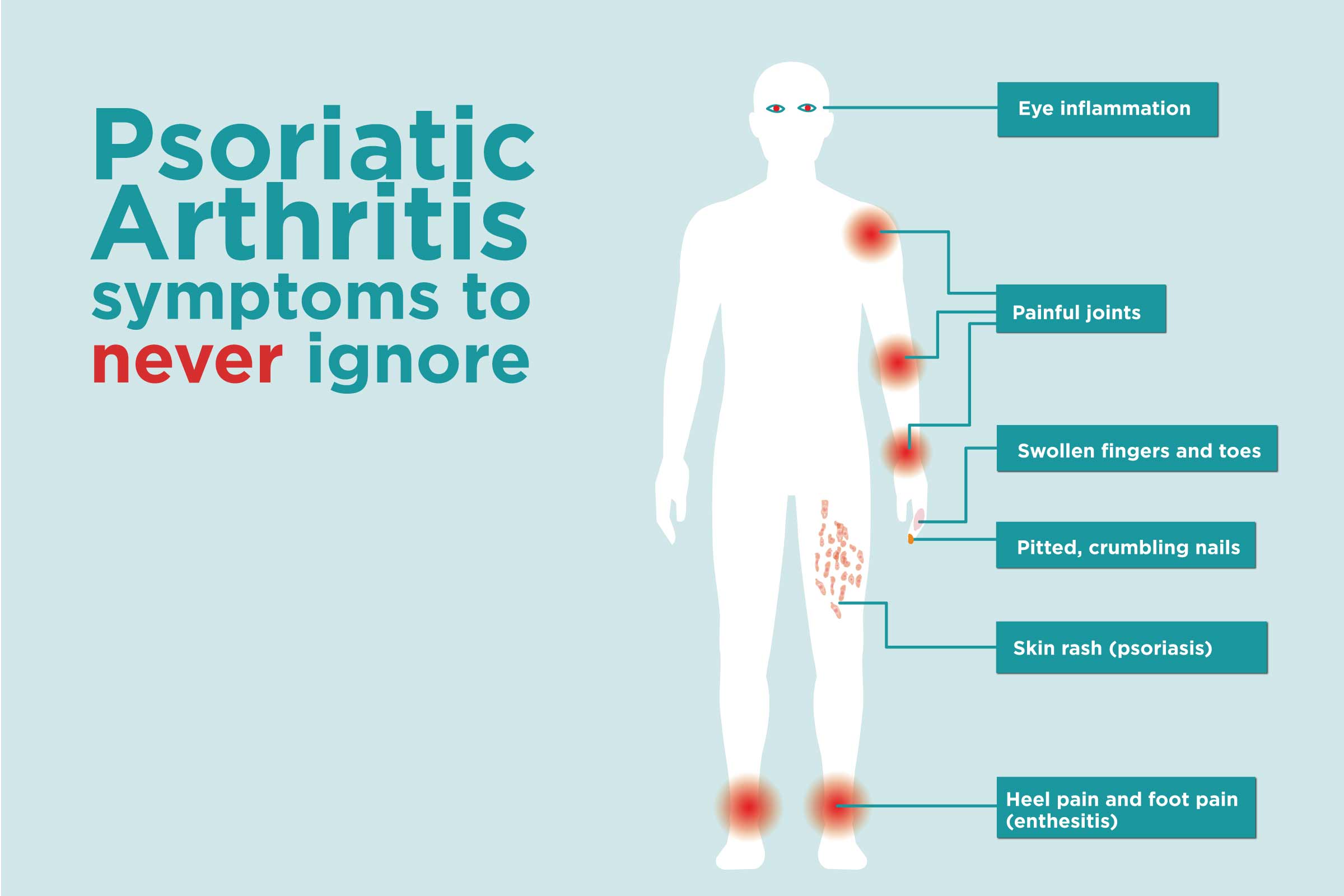
What Are The Symptoms Of Psa
PsA can affect any joint in the body. It can affect one joint or several joints , fingernails, toenails, and tendons where they join onto the bone. Some of the symptoms of PsA include:
- Feeling tired.
- Swollen fingers and toes that look like sausages.
- Stiffness, pain, throbbing, swelling, and tenderness in one or more joints.
- A reduced range of motion.
- Feeling stiff and tired in the morning.
- Changes in fingernails or toenails, such as the nail separating from the nail bed or becoming pitted .
The symptoms of PsA come and go and are not the same for everyone. A person may have symptoms that affect different parts of his or her body at different times. For example, some people may not have signs of skin and/or nail problems and may have only joint pain and swelling.
Is Ibp A Symptom Of Different Diseases
Once IBP has been determined, it becomes important to identify the root cause of the condition. IBP is associated strongly with, but not diagnostic of, several inflammatory conditions that may have both axial and peripheral pain features . The classic association of IBP symptoms is with axSpA however, IBP may also be present in conjunction with other seronegative spondyloarthropathies such as PsA, enteropathic arthropathy, juvenile idiopathic arthritis, and reactive arthritis . The accuracy of IBP in differentiating patients with axPsA from patients with other causes of back pain has not been fully clarified . AxSpA consists of several inflammatory conditionsan umbrella stateof which the radiographic version is AS. These disease states are all characterized clinically by IBP . Considerable overlap exists between the symptoms of these diseases, which can make differential diagnosis difficult .
Also Check: Is Rheumatoid Arthritis Reversible
The Invisible Pain Of Enthesitis
One of the first things that come to mind when you think about psoriatic arthritis is joint pain and deterioration. But in my experience, what is equally bad, and if not in some ways worse than psoriatic arthritis, is enthesitis.
The pulling and throbbing pain that comes with enthesitis is very difficult to manage, and for me, makes my arm nearly unusable. And yet, it doesnt present like many psoriatic arthritis aches and pains because there isnt any telltale redness or swelling. It doesnt look any different than any other part of my body.
But when I think about how bad the pain that I experience actually is, I feel like I should see the mangled remains of what should be an arm. But I dont. On the outside, it just looks like a regular arm. And even my bloodwork showed no trace of the pain I was experiencing.
What Organs Does Psoriatic Arthritis Affect

Due to widespread inflammation, psoriatic arthritis can affect your internal organs but this occurs only in very rare cases and should not be a major concern. More common symptoms to watch out for beyond joint pain and inflammation are fatigue and anemia, mood changes or depression, high blood pressure/cholesterol, diabetes, and obesity.
You May Like: The Symptoms Of Arthritis
Trying To Find Relief From Enthesitis Pain
As is the case with many psoriatic arthritis symptoms, if you can manage the inflammation, then you can manage the pain. Enthesitis pain usually responds to anti-inflammatory medicines , ice, and plenty of rest.
Regardless, it always comes back to doing your best to manage your immune system and control the levels of inflammation in your body.
Id love to know, have you experienced enthesitis with psoriatic arthritis? Do you believe that it is more prominent than the statistics initially suggest? Most importantly, how are you dealing with it? Share in the comments below!
What Is An Autoimmune Disease
Autoimmune disease happens when the bodys natural defense system cant tell the difference between your own cells and foreign cells, causing the body to mistakenly attack normal cells. There are more than 80 types of autoimmune diseases that affect a wide range of body parts.
According to the classification criteria of the Assessment of SpondyloArthritis international Society , inflammatory back pain typically lasts for three months or more with an insidious or unknown onset, begins in patients at an age younger than 40, improves with exercise but gets worse with rest, and causes increased pain at night.
Mechanical back pain, however, can have an onset at any age, although it is more common in middle-aged and older individuals, can be acute from a specific event that causes an injury, and often feels worse with movement but improves with rest. These symptoms can result from injury or damage to the lower back muscles, tendons, ligaments, discs, joints, or vertebrae.
Recommended Reading: Does Arthritis Hurt All The Time
Psoriatic Arthritis And Back Pain: What You Need To Know
Psoriatic arthritis is a inflammatory type of arthritis that develops in some people with psoriasis, an autoimmune disease that causes skin cells to build up and form scaly plaques. Psoriasis affects 74 million adults in the United States, and about 30% of patients diagnosed with psoriasis develop psoriatic arthritis.
Psoriatic arthritis causes inflammation in many joints of the body because the immune system is attacking its own joints. It commonly affects the lumbar spine, or low back.
Unpredictable Flares Can Make Planning Hard
One of the biggest challenges of dealing with psoriatic arthritis is not being able to anticipate when flares will strike. These unwelcome episodes can affect both your personal and professional life.
In a study presented at the 2018 Annual Perspectives in Rheumatic Diseases Conference, researchers found about 80 percent of participants with psoriatic arthritis said they were partially or totally unemployed due to their condition.
More than half of respondents reported having difficulty spending time with friends.
I never know, day to day, what Im going to feel like or what my body will be able to do, Donaldson says.
The erratic nature of the disease can make planning problematic.
The hardest part of living with this disease is the unpredictability, Covert agrees. How many naps will I need? Will I even need a nap, or will I be able to get out of bed? Will I be able to walk today? And if so, how long and how far?
You May Like: Rheumatoid Arthritis In Neck And Shoulders
Who Will Be Responsible For My Healthcare
Youre likely to see a team of healthcare professionals.
Your doctor, usually a rheumatologist, will be responsible for your overall care. And a specialist nurse may help monitor your condition and treatments. A skin specialist called a dermatologist may be responsible for the treatment of your psoriasis.
You may also see:
- a physiotherapist, who can advise on exercises to help maintain your mobility
- an occupational therapist, who can help you protect your joints, for example, by using splints for the wrist or knee braces. You may be advised to change the way you do some tasks to reduce the strain on your joints.
- a podiatrist, who can assess your footcare needs and offer advice on special insoles and good supportive footwear.
Loss Of Significant Joint Mobility
For example, you were able to flex your wrist 60 degrees, and two years later, you lost 50 percent of that range of motion. Its possible to feel okay and still experience loss of range of motion, says Dr. Domingues. But the idea is to prevent joint damage and to make you have less pain. If you have less pain and are still progressing, that means your treatment could be working better.
You May Like: Arthritis In Lower Right Side Of Back
What Can I Do Right Now
Join A Community That Understands
MyPsoriasisTeam is the social network for people with psoriasis and psoriatic arthritis. On MyPsoriasisTeam, members of a community of more than 87,000 strong provide each other with support, share their stories, and discuss life with psoriasis and PsA.
Do you experience PsA symptoms in your knees? How do you manage your pain? Join MyPsoriasisTeam today and share your story in the comments below, or start a conversation by posting on your Activities page.
Read Also: Mayo Clinic Joint Pain
When To Get Medical Advice
See a GP if you have persistent pain, swelling or stiffness in your joints even if you have not been diagnosed with psoriasis.
If you’ve been diagnosed with psoriasis, you should have check-ups at least once a year to monitor your condition. Make sure you let the doctor know if you’re experiencing any problems with your joints.
Home Remedies And Self Care
Some home remedies can help you to prevent and relieve hand and nail symptoms of PsA.
For relieving hand and finger joint pain, try:
- Applying ice to hand joints for ten minutes at a time as needed to reduce pain and swelling
- Massaging affected areas
- Wearing hand splints to support and protect wrist, hand and finger joints
- Taking breaks from writing and typing
- Performing hand exercises to stretch and strengthen the muscles and joints of the hand and fingers
For managing nail symptoms:
- Treat nail fungus infections with antifungal creams
- Avoid fake nails as they can injure nail beds
- Trim cuticles, and avoid pulling at the cuticles to avoid injuries and flares
- Keep fingernails trimmed and clean to prevent injuries
- Wear gloves when doing household chores or gardening
- Use clear nail polish in order to notice nail changes quickly
- Dont use nail polish if you have an active nail infection
You May Like: Rheumatoid Arthritis And Lower Back Pain
Types Of Psoriatic Arthritis And Where Psa Shows Up On The Body
Most people will experience psoriatic arthritis in a few joints but there are different types and locations on the body where it may show up.
In fact, you may be told you have a specific type of PsA based on where the inflammation occurs. Some people experience asymmetric symptoms in which joints on one side of the body are affected, such as one wrist or one knee, while others have symmetricsymptoms, involving the same joints on both sides of the body, such as both knees.
The most common types are:
- axial spondyloarthritis which mainly affects your back, including your sacroiliac joints . About 40% of those with PsA joint pain experience spine and sacroiliac joint pain.4
- distal, small joint polyarthritis, especially involving what are called the distal interphalangeal joints thats your first knuckle from the top of the finger. About 50% of people with PsA experience inflammation in the entire finger this is clinically termed dactylitis you may hear people call it sausage digit or sausage finger. Toes may also be affected.
- symmetric, small joint polyarthritis, which affects multiple joints on both sides of your body and can be very similar to rheumatoid arthritis a rheumatologist can help to differentiate
- asymmetric oligoarthritis, meaning a few joints are affected on one side of your body, usually your lower body such as the knee, ankle, or foot.
How Is It Diagnosed What Should I Do Who Should I See
If you feel you may have psoriatic arthritis you should firstly talk to your GP and explain to him your concerns and why you feel you may have psoriatic arthritis.
You may be lucky in that your GP spots all the early warning clues to your aches and pains, and diagnoses you correctly for prompt treatment options. However, there are still many people who are diagnosed much later due to lack of knowledge. This is not a criticism, but merely that GPs have to have such a wide knowledge of many conditions and with psoriatic arthritis, it is not always as simple or obvious to diagnose.
A review of your medical history by your GP, symptoms, and blood tests to rule out certain other conditions are needed. Absence of rheumatoid factor in the blood often helps to distinguish psoriatic arthritis from rheumatoid arthritis.
Pitting of the finger nails, discolouration of the nail due to abnormalities in the growth of the tissue in the nail bed are always a certain clue of psoriatic arthritis presence. People with psoriatic arthritis almost always have nail involvement.
Don’t Miss: Signs Of Arthritis In Arm
Psa Affects People Differently
No people with PsA are affected the same. Some people with the condition might only have peripheral joint disease where only their hands, wrists, knees, and other large joints are affected. The research shows that peripheral joint disease in PsA is quite common and often symmetrical and polyarticular .
Others with PsA might have only spine involvement. Still others will be affected by joint and spine inflammation.
Many people with PsA have skin involvement while others dont have any skin symptoms or psoriasis. It is more common to have skin symptoms with PsA, but there are people with PsA who dont have skin symptoms. In up to 80% of people with PsA, skin disease usually precedes joint disease.
Other effects of PsA include:
- Axial disease: Also called psoriatic spondylitis, a subtype of PsA that affects the spine and joints of the pelvis
- Enthesitis: Inflammation of the entheses, the sites where tendons or ligaments insert into the bone
- Dactylitis: Diffuse swelling of a finger or toe, described as “sausage-like”
- Nail psoriasis: Changes to nails, including thickened nails, nail pitting , discoloration, nailbed separation, and nail shape changes
Not everyone with PsA will experience all the possible effects of the condition. Each person will experience a different combination of symptoms and severity.
Medical Writing And Editorial Assistance
The authors thank Kheng Bekdache, PhD, and Eric Deutsch, PhD, CMPP, of Health Interactions, Inc, Hamilton, NJ, USA, for providing medical writing support/editorial support, which was funded by Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA, in accordance with Good Publication Practice guidelines .
Read Also: Topical Arthritis Treatments
Why Your Mental Health Matters When Living With Psoriatic Arthritis
Living with a chronic condition that requires life-long management to ease pain and reduce disease progression can take its toll on a persons mental and emotional reserves. Anxiety and depression are both prevalent in people with psoriatic arthritis, with data showing 1 in 3 patients with at least mild anxiety and 1 in 5 with at least mild depression.
Not only do anxiety and depression interfere with your quality of life, but they also are linked to greater disease activity.13 So it is important to recognize any mental or emotional challenges you may be feeling and seek help.
Will Drug Treatments For Psoriatic Arthritis Make My Psoriasis Worse

Some drug treatments may make psoriasis worse, but then again, some can also make it better too. Before you start any treatments offered, discuss this both with your dermatologist and rheumatologist. DONT FORGET to politely request that both consultants let each other know of your treatment regimes, this helps both of them evaluate your treatment and any side effects that you may be likely to experience. Some people find that when their psoriasis is bad their arthritis is also bad and as one improves, so does the other. This most often occurs when the skin and joint disease start simultaneously. Some of the arthritis treatments also help the skin and this is can help the doctors decide which is the best drug to use.
Recommended Reading: Get Rid Of Arthritis
What Tests Will I Be Required To Take During My Diagnosis And Treatments
A full case history will be taken, urine and blood tests requested, x-rays, sometimes specialist x-rays, images and scans may also be requested, plus a full examination of your affected parts i.e. back, hands, feet etc.
In summary points to remember when seeing your doctor:
Ask about your medicines:
What Are The Symptoms Of Psoriasis
There are different types of psoriasis. The most common is chronic plaque psoriasis. This causes patches of red, raised skin, with white and silvery flakes.
It can occur anywhere on the skin, but most commonly at the elbows, knees, back, buttocks and scalp.
Psoriasis can cause small round dents in finger and toe nails, this is known as pitting. Nails can also change colour, become thicker and the nail may lift away from your finger.
Don’t Miss: Rheumatoid Arthritis Pain Worse At Night
Follow Your Treatment Plan
Perhaps the most important thing you can do is talk to your doctor about how foot pain is limiting you. Your healthcare provider will help you find the right medications to control joint pain associated with psoriatic arthritis.
Foot pain is often an unfortunate reality for people who have psoriatic arthritis, but it doesnt have to overwhelm you, says Dr. Rosian. We have a variety of different medications to treat pain and swelling and prevent permanent joint damage in your feet.