Need For New Therapies
Treatments for these diseases typically have been aimed at decreasing inflammation and pain by slowing down tissue damage and reducing complications. Most people with RA have only a partial response to available drugs, and many only respond to drugs for a limited period of time. In the case of lupus, no effective targeted therapies exist for the most severe forms of the disease. Research is needed to better understand the underlying disease process and identify parts of the immune system that aren’t functioning correctly. This insight will help reveal the most promising new biological targets for drug development and match existing drugs to patients with specific molecular profiles who are most likely to benefit.
What Is The Safest Drug For Rheumatoid Arthritis
The safest drug for rheumatoid arthritis is one that gives you the most benefit with the least amount of negative side effects. This varies depending on your health history and the severity of your RA symptoms. Your healthcare provider will work with you to develop a treatment program. The drugs your healthcare provider prescribes will match the seriousness of your condition.
Its important to meet with your healthcare provider regularly. Theyll watch for any side effects and change your treatment, if necessary. Your healthcare provider may order tests to determine how effective your treatment is and if you have any side effects.
Common Autoimmune Disease Symptoms
Despite the varying types of autoimmune disease, many of them share similar symptoms. Common symptoms of autoimmune disease include:
- Abdominal pain or digestive issues
- Recurring fever
Many women say its hard to get diagnosed, something that Orbai agrees with. Its not black or white, she says. Theres usually no single test to diagnose autoimmune disease. You have to have certain symptoms combined with specific blood markers and in some cases, even a tissue biopsy. Its not just one factor.
Diagnosis can also be difficult because these symptoms can come from other common conditions. Orbai says women should seek treatment when they notice new symptoms.
If youve been healthy and suddenly you feel fatigue or joint stiffness, dont downplay that, she says. Telling your doctor helps him or her to look closer at your symptoms and run tests to either identify or rule out autoimmune disease.
You May Like: How Serious Is Rheumatoid Arthritis
Ra And The Autoimmune Attack On Joints
In patients with ACPA and/or RF, autoantibody production and inflammation occurs systemically before it occurs in the joints. Therefore, it is thought that some other factor or trigger is involved in causing the early systemic autoimmune response to move to the synovium , leading to the symptoms characteristic of RA.1
This unknown factor causes leukocyte migration and infiltration into the synovium. As the immune system is activated and the disease progresses, a cascade of inflammatory cell types and immune system chemicals are produced. These immune system cells and the wide range of chemicals they produce play a role in the autoimmune process, which ultimately causes joint destruction.1
How Is Ra Diagnosed
RA is diagnosed by reviewing symptoms, conducting a physical examination, and doing X-rays and lab tests. Its best to diagnose RA earlywithin 6 months of the onset of symptomsso that people with the disease can begin treatment to slow or stop disease progression . Diagnosis and effective treatments, particularly treatment to suppress or control inflammation, can help reduce the damaging effects of RA.
Don’t Miss: Is Grapes Good For Arthritis
What Is An Autoimmune Disease
The immune system is our body’s way of fighting off microorganisms that can make us sick. When functioning normally, the immune system can correctly identify and overcome infections. But sometimes, the immune system incorrectly identifies tissues in the body as dangerous, causing harmful types of inflammation when no actual threat is present. This malfunction can happen spontaneouslywithout a clear causeor it can sometimes occur in reaction to an infection.
Autoimmune illness is becoming more common, according to studies. One well-known autoimmune disease is type 1 diabetes. Other autoimmune diseases you may have heard of include RA, Hashimoto’s autoimmune thyroiditis, Sjögren’s syndrome, celiac disease, ankylosing spondilytis, Graves’ disease, vitiligo, lupus, and psoriasis.
How Is Osteoarthritis Diagnosed
The physician will begin with a complete medical history and a physical examination. During the exam, the doctor will look for an enlarged or bumpy joint, signs of swelling, or decreased range of motion. Your doctor may then order x-rays, which can show a decrease in the cartilage space, new bone formation, or incorrect alignment. In some cases, your doctor may perform an aspiration the removal of fluid from a swollen joint or bursa to exclude infection, gout, or rheumatoid arthritis as possible causes of your joint pain.
Read Also: What Foods Cause Arthritis To Worsen
Rheumatoid Arthritis Is A Widespread Autoimmune Disease That Affects Millions Of People Around The World And Is Not Yet Treatable
A team of scientists from the College of Medicine and Life Sciences, University of Toledo and Department of Internal Medicine, University of Michigan, has developed an experimental vaccine that shows significant promise in preventing rheumatoid arthritis, a disease that is not yet treatable.
The study, published in the journal Proceedings of the National Academy of Sciences, mark a significant advance in the research of rheumatoid arthritis and autoimmune illnesses in general.
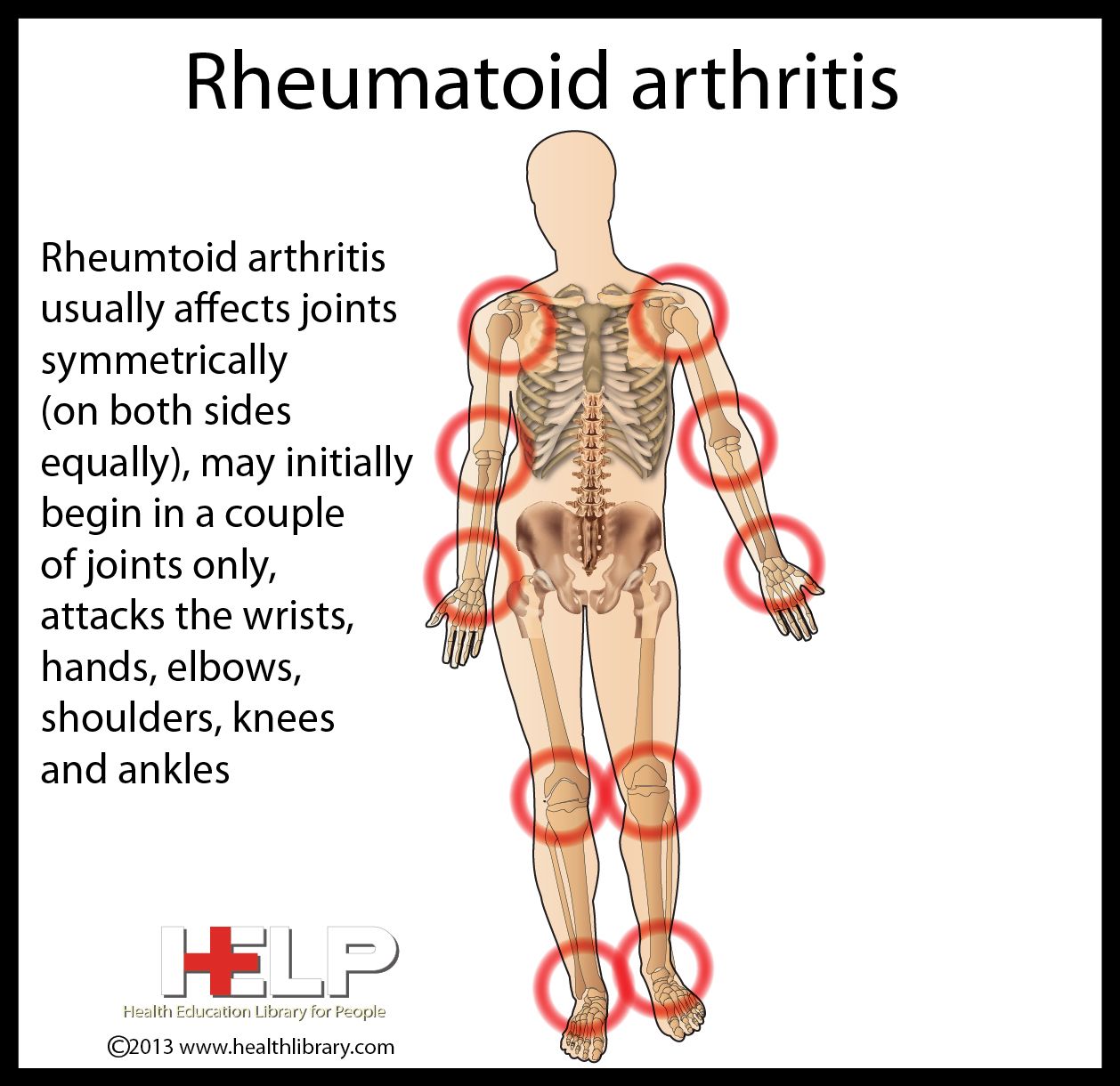
Rheumatoid arthritis, one of the most prevalent autoimmune illnesses, develops when the bodys immune system assaults and destroys healthy tissue, most notably the lining of joints in the hands, wrists, ankles, and knees.
According to some estimates, rheumatoid arthritis affects up to 1% of the global population.
In spite of its high prevalence, there is no cure and we dont entirely know what brings it on. This is true of nearly all autoimmune diseases, which makes treating or preventing them so difficult, said Dr. Ritu Chakravarti, the study lead author from UToledo College of Medicine and Life Sciences.
If we can successfully get this vaccine into the clinic, it would be revolutionary.
Chakravarti has spent years researching a protein known as 14-3-3 zeta and its role in immunological pathologies such as aortic aneurysms and interleukin-17, a cytokine linked to autoimmune illnesses.
The study team had previously identified the protein as a potential cause for rheumatoid arthritis.
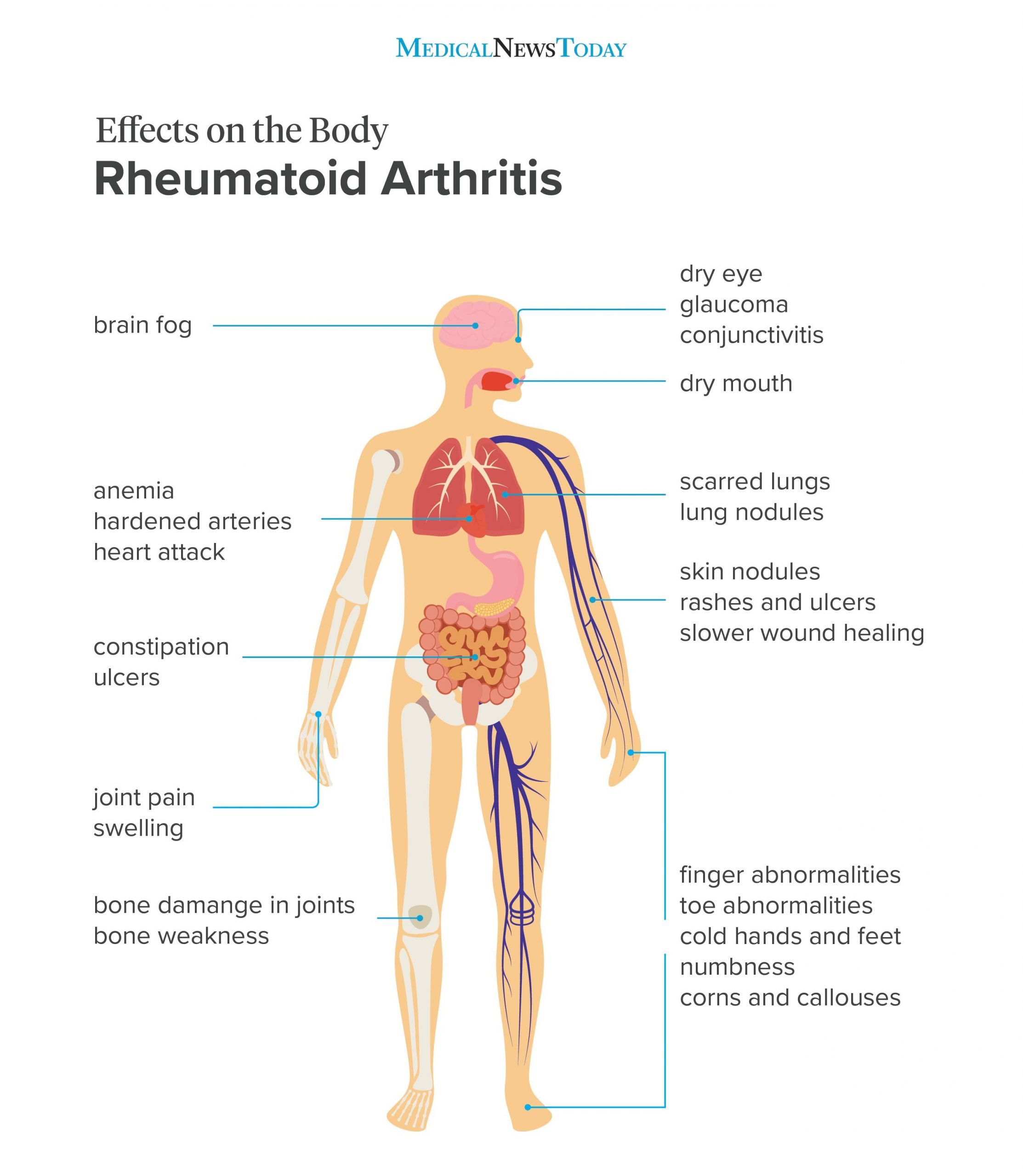
How Does It Affect Your Body
Immune system cells move from the blood into your joints and the tissue that lines them. This is called the synovium. Once the cells arrive, they create inflammation. This makes your joint swell as fluid builds up inside it. Your joints become painful, swollen, and warm to the touch.
Over time, the inflammation wears down the cartilage, a cushy layer of tissue that covers the ends of your bones. As you lose cartilage, the space between your bones narrows. As time goes on, they could rub against each other or move out of place. The cells that cause inflammation also make substances that damage your bones.
The inflammation in RA can spread and affect organs and systems throughout your body, from your eyes to your heart, lungs, kidneys, blood vessels, and even your skin.
Don’t Miss: Does Cracking Knuckles Cause Arthritis
Rheumatoid Arthritis Vs Osteoarthritis
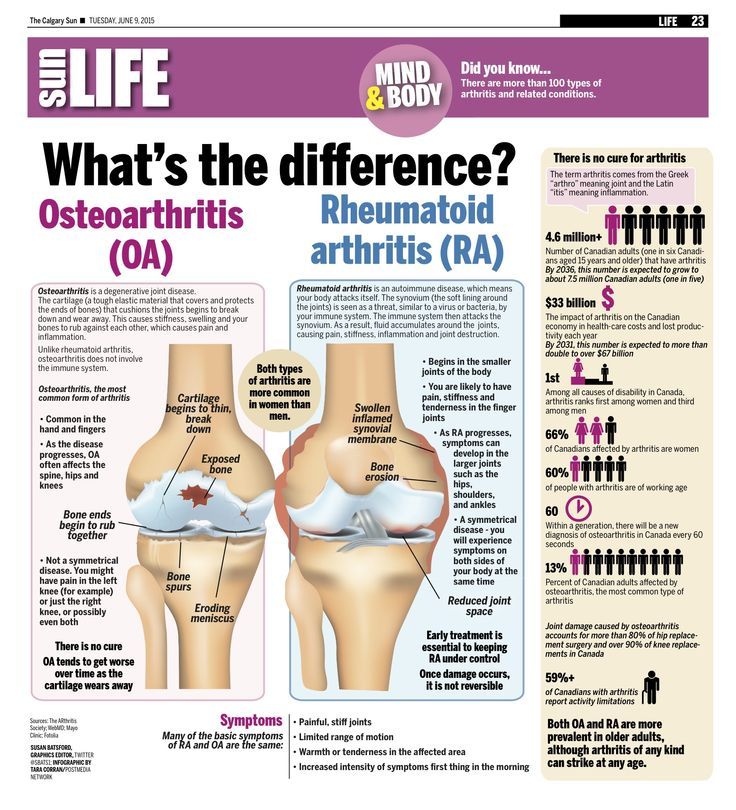
RA is an autoimmune disease that causes inflammation in the joints, leading to pain, stiffness, and swelling. Osteoarthritis leads to many of the same symptoms as RA but is due to the typical wear and tear of the joints.
While RA usually affects the same joints on both sides of the body, osteoarthritis may only affect one side.
Although other symptoms can help a person figure out if they are experiencing RA or osteoarthritis, only a doctor can diagnose these conditions.
It may be difficult for a doctor to diagnose RA in its early stages, as it can resemble other conditions.
The CDC recommends getting a diagnosis within 6 months of the onset of symptoms so that treatment can begin as soon as possible.
A doctor will look at the persons clinical signs of inflammation and ask how long the person has experienced them and how severe their symptoms are. They will also perform a physical examination to check for swelling, functional limitations, or other unusual presentations.
They also may recommend some tests, including:
Preclinical Autoimmune Disease: A Comparison Of Rheumatoid Arthritis Systemic Lupus Erythematosus Multiple Sclerosis And Type 1 Diabetes
- 1Department of Rheumatology and Clinical Immunology, Amsterdam Rheumatology and Immunology Centre, Amsterdam University Medical Centers, University of Amsterdam, Amsterdam, Netherlands
- 2Department of Experimental Immunology, Amsterdam University Medical Centers, University of Amsterdam, Amsterdam, Netherlands
- 3Amsterdam Rheumatology Center, Amsterdam, Netherlands
- 4Department of Neurology, MS Center Amsterdam, Amsterdam University Medical Center , Vrije Universiteit Amsterdam, Amsterdam Neuroscience, Amsterdam, Netherlands
- 5Department of Endocrinology and Metabolism, Amsterdam University Medical Centers, University of Amsterdam, Amsterdam, Netherlands
- 6Amsterdam Rheumatology and Immunology Center, Reade, Amsterdam, Netherlands
Read Also: How To Treat Arthritis In Elbow
Lifestyle And Environmental Factors
Although genetic factors play an important role in risk of autoimmunity, genetic predisposition is able to explain only up to 50% of the risk of developing RA and T1D, leaving half of the patients without any known genetic marker . Numerous studies have investigated the role of environmental factors in disease development including lifestyle factors, comorbidities, external agent exposure and bacterial and viral infections .
Smoking is one of the most prominent environmental risk factors, and has a role in RA, SLE, and MS . Although no association has been described between smoking and T1D, this is more likely due to the young age of T1D onset. Smoking causes citrulline autoimmunity in the lung in genetically susceptible individuals and also triggers the production of RF , explaining an association between smoking and seropositive RA. In SLE, smoking is a risk factor for anti-dsDNA production , while in MS smoking induces an increased axonal demyelination and disruption of the blood-brain barrier, in parallel with an immunomodulatory effect mediated by increasing both nitric oxide levels and its metabolites . Both in RA and MS, but not in SLE, smoking has a dose-response relation with disease risk . After smoking cessation, the increased risk for RA and SLE remains present for several years .
Coexisting Diseases And Conditions
Hypertension, chronic obstructive pulmonary disease, diabetes, hypothyroidism, malignancies, systemic lupus erythematosus, psoriatic arthritis, Sjorgrens syndrome, alopecia areata, antiphospholipid syndrome, autoimmune hepatitis, autoimmune inner ear disease, ankylosing spondylitis, and osteoporosis.
Don’t Miss: What To Do For Arthritis In Wrist
What Causes Rheumatoid Arthritis
The exact cause of rheumatoid arthritis is unknown. Researchers think its caused by a combination of genetics, hormones and environmental factors.
Normally, your immune system protects your body from disease. With rheumatoid arthritis, something triggers your immune system to attack your joints. An infection, smoking or physical or emotional stress may be triggering.
Is rheumatoid arthritis genetic?
Scientists have studied many genes as potential risk factors for RA. Certain genetic variations and non-genetic factors contribute to your risk of developing rheumatoid arthritis. Non-genetic factors include sex and exposure to irritants and pollutants.
People born with variations in the human leukocyte antigen genes are more likely to develop rheumatoid arthritis. HLA genes help your immune system tell the difference between proteins your body makes and proteins from invaders like viruses and bacteria.
How Is Juvenile Idiopathic Arthritis Diagnosed
Diagnosing JIA may be difficult. There is no single test to confirm the disease. Your childs healthcare provider will take your childs health history and do a physical exam. Your child’s provider will ask about your child’s symptoms, and any recent illness. JIA is based on symptoms of inflammation that have occurred for 6 weeks or more.
Tests may also be done. These include blood tests such as:
Your child may also have imaging tests. These can show how much damage the bones have. The tests may include:
- X-rays. This test uses a small amount of radiation to make images of organs, bones, and other tissues.
- CT scan. This uses a series of X-rays and a computer to make detailed images of bones, muscles, fat, and organs. CT scans are more detailed than regular X-rays.
- MRI. This test uses large magnets and a computer to make detailed pictures of organs and structures in the body.
- Bone scan. This uses a small amount of radiation to highlight the bones in a scanner.
Other tests may include:
- Urine tests. These look for blood or protein in the urine. This can mean the kidneys are not working normally.
- Joint aspiration . A small sample of the synovial fluid is taken from a joint. It’s tested to see if crystals, bacteria, or viruses are present.
- Full eye exam done by an ophthalmologist
Don’t Miss: What To Do For Arthritis In Hip
Does Rheumatoid Arthritis Cause Fatigue
Everyones experience of rheumatoid arthritis is a little different. But many people with RA say that fatigue is among the worst symptoms of the disease.
Living with chronic pain can be exhausting. And fatigue can make it more difficult to manage your pain. Its important to pay attention to your body and take breaks before you get too tired.
What are rheumatoid arthritis flare symptoms?
The symptoms of a rheumatoid arthritis flare arent much different from the symptoms of rheumatoid arthritis. But people with RA have ups and downs. A flare is a time when you have significant symptoms after feeling better for a while. With treatment, youll likely have periods of time when you feel better. Then, stress, changes in weather, certain foods or infections trigger a period of increased disease activity.
Although you cant prevent flares altogether, there are steps you can take to help you manage them. It might help to write your symptoms down every day in a journal, along with whats going on in your life. Share this journal with your rheumatologist, who may help you identify triggers. Then you can work to manage those triggers.
What Is The Difference Between Rheumatoid Arthritis And Osteoarthritis
Rheumatoid arthritis and osteoarthritis both cause joint pain, stiffness, and limited range of motion, but the two diseases are distinct in their root cause and treatment.
Rheumatoid arthritis is an autoimmune condition where a persons own immune system attacks their joints, causing inflammation. Rheumatoid arthritis typically affects many joints simultaneously, especially in the hands, wrists, and feet, and is treated with medications to suppress the immune response.
Osteoarthritis is not an autoimmune disease, and although the exact causes are not known, multiple risk factors have been identified. In a healthy joint, cartilage provides cushioning and a smooth joint surface for motion. In an osteoarthritic joint, as cartilage is irreversibly destroyed and bone abnormalities develop, movement becomes painful and more difficult.
Recommended Reading: How Do You Use Turmeric For Arthritis
Signs And Symptoms Of Autoimmune Disease
Autoimmune diseases can develop from a variety of factors with no known definitive causes for the onset of the disease. Some suspected sources are:
- Bacterial or viral infection
- Chemical toxins
- Environmental pollutants
When the immune system determines that healthy cells are foreign, it begins to produce antibodies to fight off the healthy cells it believes to be the source of an illness or infection. When an autoimmune disease is suspected, a rheumatologist will administer tests to determine what antibodies are being produced. There are more than 80 potential autoimmune diseases and some of the most common areas affect can be:
- Joints and muscles
- Connective tissue
When faced with symptoms or an autoimmune disease diagnosis, it is very important to seek treatment from an experienced rheumatologist to find the best plan to manage symptoms. Dr. Susan Baker, MD specializes in Rheumatology and Internal Medicine in Beverly Hills, and offers patients everything from arthritis treatment to Lupus.
Dont Miss: Is Broccoli Good For Arthritis
What Are The Symptoms Of Juvenile Idiopathic Arthritis
Symptoms may appear during episodes . Or they may be ongoing . Each childs symptoms can vary. Symptoms may include:
- Swollen, stiff, and painful joints in the knees, hands, feet, ankles, shoulders, elbows, or other joints, often in the morning or after a nap
- Eye inflammation
- High fever and rash
- Swollen lymph nodes
These symptoms can seem like other health conditions. Make sure your child sees his or her healthcare provider for a diagnosis.
You May Like: Can You Have Psoriatic Arthritis And Rheumatoid Arthritis
How Is Rheumatoid Arthritis Diagnosed
Your healthcare provider may refer you to a physician who specializes in arthritis . Rheumatologists diagnose people with rheumatoid arthritis based on a combination of several factors. Theyll do a physical exam and ask you about your medical history and symptoms. Your rheumatologist will order blood tests and imaging tests.
The blood tests look for inflammation and blood proteins that are signs of rheumatoid arthritis. These may include:
- Erythrocyte sedimentation rate or sed rate confirms inflammation in your joints.
- C-reactive protein .
- About 80% of people with RA test positive for rheumatoid factor .
- About 60% to 70% of people living with rheumatoid arthritis have antibodies to cyclic citrullinated peptides .
Your rheumatologist may order imaging tests to look for signs that your joints are wearing away. Rheumatoid arthritis can cause the ends of the bones within your joints to wear down. The imaging tests may include:
In some cases, your provider may watch how you do over time before making a definitive diagnosis of rheumatoid arthritis.
Prevalence And Types Of Autoimmune Diseases
There are more than 80 types of autoimmune diseases. Symptoms depend on which part of the body is affected. There are autoimmune disorders that target specific types of tissue . Other autoimmune diseases may target a specific organ. Any organ can be involved. Characteristics that are typically associated with the autoimmune disease include inflammation, pain, muscle aches, fatigue, and a low-grade fever. Inflammation is usually the first sign of an autoimmune disease.
Autoimmune diseases affect more than 23.5 million Americans, according to the U.S. Department of Health and Human Services. While some autoimmune diseases are rare, a number of the conditions are common. Autoimmune diseases can affect anyone but it is believed that some people have a genetic predisposition for developing an autoimmune disease under certain circumstances . People at greater risk for developing an autoimmune disease include:
- Women of childbearing age
- People who have a family history of autoimmune disease
- People who have certain environmental exposures that could act as the trigger
- People of a particular race or ethnicity
Many types of arthritis are considered autoimmune diseases, including:
- Ankylosing spondylitis
Recommended Reading: Are Black Beans Bad For Arthritis