Small Joint Inflammation: Symptoms In The Fingers Wrists Toes And Ankles
For more than half of RA patients, the first symptoms will occur in one or more of the small joints of the fingers , the wrists, the toes , or the ankles. Symptoms can begin slowly and subtly over a period of weeks or months, worsening over time.
In the majority of patients, this swelling and pain is symmetrical, meaning the same joints are affected on both sides of the body.
But this is not always the case. Its important not to wait to treat until the disease becomes symmetric. Early diagnosis and treatment are key to prevent joint damage even if only one joint on one side of the body is affected, notes Rebecca Manno, MD, a rheumatologist and adjunct assistant professor of medicine at the Johns Hopkins University School of Medicine in Baltimore.
How Your Ra Treatment Plan Prevents Disease Progression
Perhaps the biggest factor that affects how RA progresses is if youre in treatment with a specialist who can put you on medications to slow the disease. Being on a DMARD or biologic therapy for RA is the best way to prevent progression, Dr. Lally says.
Disease-modifying anti-rheumatic drugs are usually the first line in medication. Methotrexate is the anchor drug for rheumatoid arthritis, Dr. Bhatt says. Some patients are scared because methotrexate is also used for cancer chemotherapy so they dont want to take a chemo pill, but those we use for RA are a very small dose with lesser chance of side effects. Your doctor will reassess in a month or so and see if its necessary to add in other drugs.
If after three to six months they have still not responded then we progress to medications called biologics, Dr. Bhatt says. These genetically engineered drugs target the inflammation process specifically, and are usually self-injected or infused via IV in your doctors office or a medical center. There are sub-classes and different types, Dr. Bhatt says. Your doctor will try various medications to see which you respond best to.
What Side Effects Can Occur In The Treatment Of Post
Any medical or surgical treatment can have side effects or risks. NSAIDs can cause stomach irritation, kidney, liver, or other problems. Cortisone can cause elevation of heart rate and blood sugar and should not be given too often. Surgical treatments have risks of infection, damage to surrounding structures, and wearing out or loosening of implants. Also, there is a risk of medical complications such as blood clots, heart attack, stroke, infection, and other problems. Fortunately, all these problems are quite infrequent. Most surgery is very successful in improving pain and function.
After surgery, you can expect some discomfort. You may need to use a sling, crutches, a cane, or a walker temporarily. You can expect your pain relief and function to gradually improve over months after surgery.
Don’t Miss: Is Rheumatoid Arthritis Curable
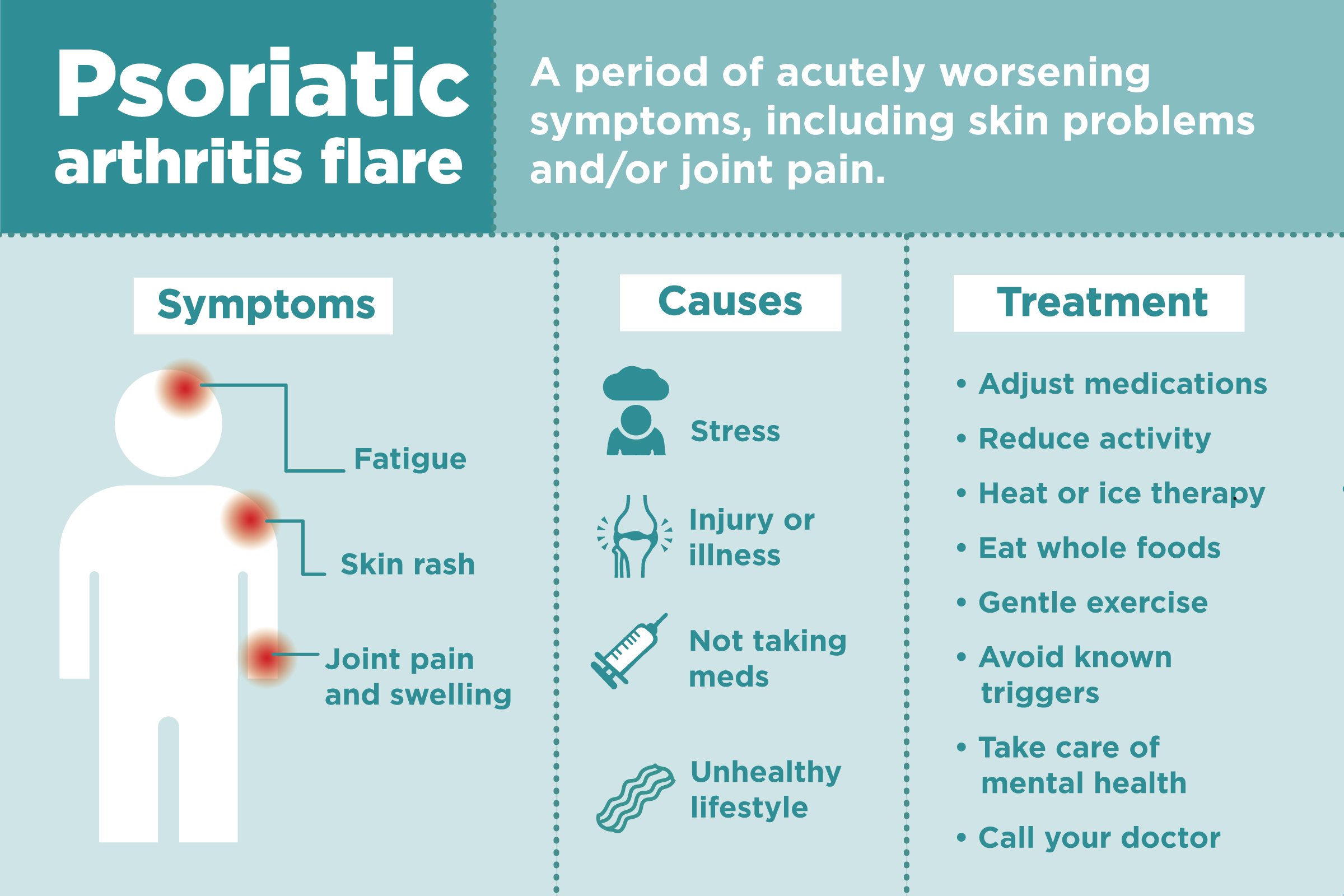
How Do I Know If I Have Osteoarthritis
Unlike other types of arthritis, the pain from osteoarthritis usually develops gradually over many months or years. Often it increases with activities that put stress on the joint, such as running or prolonged walking. Pain and joint swelling tend to increase slowly over time. Sometimes, especially in more advanced disease, a sensation of crunching or grinding may be noticed in affected joints. Prolonged morning stiffness is not a prominent symptom in OA as compared to inflammatory arthritides, such as rheumatoid or psoriatic arthritis. Osteoarthritis does not usually cause fevers, weight loss, or very hot and red joints. These features suggest some other condition or type of arthritis.
Your healthcare provider can typically diagnose osteoarthritis by obtaining a complete history of your symptoms and examining your joints. X-rays may be helpful to make sure there is no other reason for the pain. Magnetic resonance imaging is generally not needed except in unusual circumstances or in cases when the cartilage or surrounding ligament tear is suspected. There are no blood tests that diagnose osteoarthritis. If a joint is particularly swollen, a doctor may need to drain fluid from that joint. Tests can be performed on the fluid to look for clues for other types of arthritis, such as gout.
Signs Your Ra Is Progressing
How can you tell your RA is getting worse? There’s no easy way, but some general signs include:
- Flares that are intense or last a long time
- Diagnosis at a young age, which means the disease has more time to become active in your body
- Rheumatoid nodules — bumps under your skin, often around your elbows
- Active inflammation that shows up in tests of joint fluid or blood
- Damage on X-rays when you were diagnosed
- High levels of rheumatoid factor or citrulline antibody in blood tests
Also Check: Is Banana Good For Arthritis
How Your Treatment Changes As Ra Progresses
Early stage. A key focus is to control the inflammation. Thatâs especially critical in the early phase of the disease to prevent joint damage. You may get:
- A disease-modifying antirheumatic drug , such as methotrexate
- Nonsteroidal anti-inflammatory drugs , such as aspirin and ibuprofen, for pain
Quitting smoking and losing any extra weight also can help slow your RA.
Moderate stage. This is when you may have trouble with regular daily activities because of pain. You also may tire more easily. There are several options. Your doctor may have you try combining methotrexate with two other DMARD medications, sulfasalazine and hydroxychloroquine. Another option is a stronger form of DMARDs, called biologic DMARDs, including:
- Tofacitinib
- Upadacitinib
If a certain joint is particularly inflamed, your doctor may give the joint steroid shots. Once your pain is under control, itâs important to exercise to keep ahead of your RA. You also may need physical therapy.
Severe stage. If a TNF inhibitor fails to improve your symptoms, your doctor may recommend you try a different TNF inhibitor or a different class of biologic. If you donât respond to one, you may respond to another.
Surgery is a last-resort treatment for very severe RA. That includes when your joints are deformed and damaged and limit your mobility. The three most common surgeries for RA are:
Do All Osteoarthritis Patients Get Worse
Osteoarthritis is viewed by most people as a gradual wearing out of the joints you could say it’s slowly progressive. The most current research, though, indicates that not all osteoarthritis patients worsen some actually stabilize.
Rapidly progressive joint damage is not common in osteoarthritis. Although about 40 percent of older people have X-ray evidence revealing significant osteoarthritis in their hips and knees, less than 5 percent undergo joint replacement surgery. Based on this fact alone, osteoarthritis does not continue to worsen for most patients.
Read Also: Acute Arthritis Attack
Treatment For Advanced Osteoarthritis
In its early stages, physical therapy, regular exercise, weight loss, and assistive devices can help you manage OA.
You can use these lifestyle changes alongside over-the-counter and home remedies to manage pain and inflammation, such as:
- nonsteroidal anti-inflammatory drugs
- topical creams and ointments containing NSAIDs or capsaicin
- heat or cold pads
Acupuncture may help, but theres not enough research evidence to confirm its effectiveness.
Experts no longer recommend massage therapy as a treatment for OA. However, it may help relieve stress and anxiety, which are common with conditions that involve chronic pain.
Vitamin E Protects The Subchondral Vascular System Which May Reduce The Necrosis And Remodeling Of Osteoarthritis
There is evidence indicating that impaired microvascular blood flow, which may arise due to various combinations of pro-coagulant factors, can result in symptomatic osteoarthritis . While the survival of articular chondrocytes depends largely on the diffusion of nutrients from the synovial fluid, the osteocytes in subchondral bone obtain nourishment from a well-developed capillary plexus . In cases of osteoarthritis, synovial and subchondral vascular engorgement results in necrosis and the gradual remodeling of tissue . Vitamin E, along with a network of cellular antioxidant mediators, including catalases and superoxide dismutase, plays a role in the elimination of lipid-soluble free radicals through its action as a free radical scavenger . Furthermore, vitamin E is involved in the regulation of certain cellular events, such as the cell cycle progression of vascular smooth muscle cells, the expression of adhesion molecules, the deposition of extracellular matrix and aggregation of platelets . In addition, it attenuates capillary endothelial swelling in ischemic and remote muscle . It has also been reported that vitamin E protects vascular walls from damage by limiting cell proliferation, and by assisting in the stabilization of a fibrous cap through its effects on components of the extracellular matrix .
You May Like: Can You Get Rid Of Arthritis
How Does Ankylosing Spondylitis Progress
Despite the three stages described above, it is important to note that not all people with AS will have this progression. One study found that 1 in 4 patients with AS do not show progression seen on x-rays.4 Some factors that have been associated with more progressive or severe disease include gender and an early age when symptoms begin. Men are more likely to have more severe disease. In women, AS is more likely to be associated with a later onset, milder symptoms, and have symptoms affecting other parts of the body than the spine, such as inflammation in the eyes and arthritis in the peripheral joints. While AS symptoms may be milder in women than in men, studies have found that women with AS have symptoms that affect their day-to-day lives more.2
Treatment For Hip Arthritis
There is no cure for any type of arthritis, including hip arthritis, but there may be more ways to treat the pain and other symptoms than you would imagine.
For most patients with mild hip arthritis, early stages of treatment can include:
- Rest and ice.
- Anti-inflammatory medications .
- Acetaminophen .
You May Like: Rheumatoid Arthritis Over The Counter Medications
What Is ‘sudden Arthritis’ Exactly
The term sudden arthritis refers to inflammation and swelling in the joints with a quick onset, Nicole M. Cotter, MD, a physician board-certified in rheumatology and integrative medicine at UCHealth Yampa Valley Medical Center, tells LIVESTRONG.com.
According to the CDC, the primary symptoms of arthritis in general are:
- Redness andstiffness in the joints
Some additional symptoms, such as fever and fatigue, can also occur with arthritis.
There are a few possible explanations when the condition seems to appear out of the blue.
Early Signs Of Ankylosing Spondylitis

In most people with AS, symptoms begin in the low back and sacroiliac joints. This can cause pain and stiffness in the low back or hips, and the pain is usually worse after periods of inactivity, such as in the morning after a night’s sleep. Symptoms usually improve with activity. Early symptoms can also include fatigue, a mild fever, or loss of appetite.5,6
In addition to the sacroiliac joints, many people with AS have inflammation in the locations where the ligaments and tendons attach to the bone. This inflammation is called enthesitis and can cause “hot spots” of tenderness along the spine or along the back of the heel.5,6
Not everyone has the same early symptoms, though, and women with AS may have different symptoms, such as pain and stiffness in the neck rather than the lower back. In a small percentage of people with AS, symptoms may begin in a peripheral joint, such as the hip, knee, shoulder, or elbow.5
You May Like: Signs Of Rheumatoid Arthritis In Fingers
Early Detection And Diagnosis
As with most diseases, early detection and diagnosis are crucial for being able to treat symptoms, manage pain, and slow progression. An early diagnosis of RA can help you and your team of physicians and specialists put together an individualized treatment plan so that you can continue living a high quality of life.
Early on, you will want to discuss your case with a rheumatologist or RA specialist who can provide you with the treatment you need to delay the diseases progression. Generally, early diagnosis treatment is aggressive and targeted to properly manage the disease and prevent it from progressing.
If your RA was diagnosed in the early stage when symptoms first appeared, your chances of achieving longer periods of remission typically increase drastically. Thats not to say you wont experience flare-ups. Early diagnosis simply helps manage the disease and cannot guarantee the complete elimination of symptoms.
Some People Experience Fatigue And Other Flu
Up to a third of patients have more systemic symptoms before or along with joint pain and inflammation. This can include fatigue, muscle pain, mood changes, and low-grade fever. As the digital arthritis community CreakyJoints puts it, “Some patients describe the symptoms of RA as being ‘flu-like’ that general yucky feeling you get when you are on the verge of getting sick.”
Although these symptoms can be an early sign of RA, because they overlap with other illnesses, RA usually isn’t the first thing the doctor considers, especially without joint pain.
Other symptoms many don’t realize can also indicate RA include rashes, easily bruising, itchy and dry eyes, and sharp chest pain brought on my irritation of the costosternal joints, which connect the ribs to the breastbone.
You May Like: Aching Arms And Hands Rheumatoid Arthritis
Who Is Affected By Osteoarthritis
Approximately 80% of older adults, ages 55 years and older, have evidence of osteoarthritis on X-ray. Of these, an estimated 60% experience symptoms. It is estimated that 240 million adults worldwide have symptomatic osteoarthritis, including more than 30 million U.S. adults. Post-menopausal women have an increased incidence of knee osteoarthritis compared to men.
Chronic Joint Pain In The Knees Elbows Hips And Shoulders
Some RA patients may also experience inflammation in the joints of the knees, elbows, and hips. One or both shoulders might also become swollen, lessening range of motion so lifting or reaching becomes painful.
Rheumatoid arthritis typically does not affect the lower back, though a person may experience back pain if they are having difficulty moving other joints or walking, says Manno.
In a small percentage of people, the joint swelling can come and go, sometimes moving around to different joints and even disappearing for a time, a condition known as palindromic rheumatism. But in the vast majority of people, the joint swelling persists and worsens until its treated with medication. With treatment, the majority of people can achieve a significant lessening of symptoms or possibly even remission.
You May Like: Rash Psoriatic Arthritis
When To Call Your Doctor
Dr. Cotter urges anyone who experiences sudden symptoms of arthritis to seek medical attention immediately. If left untreated, these symptoms could lead to long-term problems in the joint.
“It is not normal for a joint to suddenly swell, and getting the correct diagnosis is of the utmost importance,” she says. “Early diagnosis and intervention will mean a better outcome.”
Any persistent issues warrant a call to your doctor as well, she says. For example, if you have joint pain without swelling or joint swelling without pain that persists, you should see your doctor for an evaluation.
Proper Oseteoarthritis Treatment Includes Exercise
There’s no cure for osteoarthritis, but there is a lot you can do to slow its progression, reduce pain, and maintain or improve function. Losing weight can be particularly helpful if you’re overweight or obese. You can often relieve pain with over-the-counter analgesics such as acetaminophen and nonsteroidal anti-inflammatory drugs , including ibuprofen and aspirin. The use of canes, splints, or braces may be necessary to protect a joint from further injury.
But if there’s one osteoarthritis treatment an individual with osteoarthritis should do every day, it’s exercise. Regular exercise strengthens muscles and improves flexibility and balance. It not only helps ease pain and stiffness but also improves overall health. It’s also good for your mood and for staving off other conditions prevalent in older age.
Exercise as an integral part of prevention and treatment of osteoarthritis, especially in people ages 65 and over. After reviewing the evidence, the group also concluded that moderate-intensity exercise does not as some have feared increase the risk for osteoarthritis.
Research suggests that older women may be able to prevent osteoarthritis pain by getting as little as one to two hours of moderately intense physical activity each week. Lack of exercise may contribute directly to osteoarthritis, especially by causing the atrophy of supportive and shock-absorbing muscles, such as those surrounding the knee.
Also Check: Remedy For Arthritis In Fingers
How Long Will It Take To Recover From Osteoarthritis & How Long Does The Symptoms Last
Osteoarthritis is one of the most widespread conditions in many of the North American countries, especially in the United States. Men and women are affected in equal numbers however women are most like to encounter this problem at an earlier age when compared to men.
This is a lasting and advancing condition identified by loss of the cartilage that conceals and shields the edges of the muscles and bones at the meeting of a joint. In the absence of this defensive layer, bone inflames another bone, resulting in soreness and irritation. This eventually leads to pain and rigidity in the joint causing discomfort in the areas around it.
Taking Control Of Osteoarthritis
It is important to understand that two joints that show the same cartilage loss on x-ray may behave very differently in terms of discomfort and limited function. The weak, stiff joint will be more painful and disabling than a joint with preserved strength and motion. And of course, additional factors such as body weight, other joint involvement and general health are also very important in determining the level of disability and quality of life. Patients who embark on a conservative course of treatment for arthritis are taking control of their condition and seeking the best possible outcome.
Certainly the place to begin is cultivating good general health, including cardiovascular conditioning. Dr. Jones also places a strong emphasis on maintaining a healthy body weight. “This is particularly important in individuals with arthritis of the hip, knee and low back, in whom excess pounds place a tremendous strain on the joint.”
Read Also: Stiff Neck Rheumatoid Arthritis