Understanding Remission And Minimal Disease Activity
Psoriatic arthritis disease progression is not inevitable. When your PsA is treated with medications that reduce immune system overactivity, you can reduce your disease activity to a point that its no longer causing significant symptoms or increasing the risk of long-term health issues.
In general, going into remission means that you are no longer showing signs of active disease. Decades ago, remission wasnt conceivable for most people with psoriatic arthritis, but thanks to a proliferation in medication treatment options, getting to remission is a possibility for PsA patients today.
However, going into remission does not mean that you will stay there indefinitely. It is common for PsA symptoms to wax and wane. Even if youve been in remission for a long time and your pain starts coming back and you start flaring more, you may need to change your medication for better control, says Dr. Haberman.
You may also hear the phrase minimal disease activity in conjunction with psoriatic arthritis and remission.
Doctors dont have a clear definition of what it means to be in remission in PsA, but they have defined something called minimal disease activity as a treatment target. This is what your doctor may use to determine whether your PsA disease activity is low enough that you have few symptoms and a low risk of long-term damage.
People are considered to be in minimal disease activity when their scores on five out of these seven criteria are low enough.
Treatment Options For Ra And Psa
Because of the differences in disease pathogenesis, clinical manifestations and response to therapy between RA and PsA, treatment strategies may differ. provides a summary of current Food and Drug Administration -approved treatments for RA and PsA. Agents targeting more upstream factors are effective in both PsA and RA, while agents targeting more downstream cytokines are more disease-specific, demonstrating significant efficacy in either RA or PsA , but not in both diseases.
Donât Miss: How Many Mg In Tylenol Arthritis
What If Everything Comes Back Normal
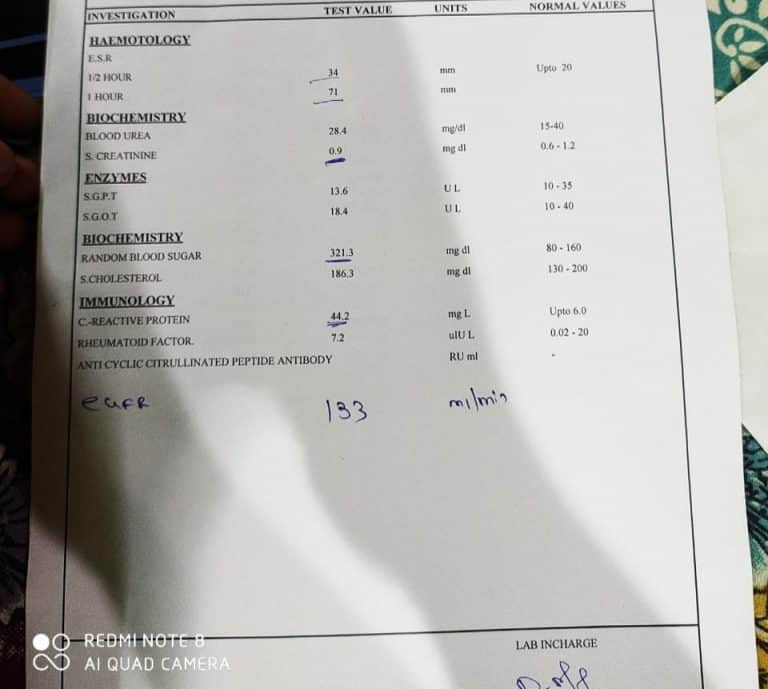
Often patients with PsA will have normal CRP and ESR levels. Similarly, while anti-CCP is typically an RA indicator, anti-CCP can be both negative or positive in PsA.
While bloodwork is certainly part of the diagnostic process, patient history and a physical examination are the most important factors to correctly diagnose PsA.4,9
Read Also: Can You Develop Rheumatoid Arthritis Later In Life
Psoriatic Arthritis Blood Test: Rheumatoid Factor
Rheumatoid factor , a protein produced by the immune system that attacks healthy tissue, is an indication of systemic inflammation.
Although RF is mostly associated with rheumatoid arthritis, it can also occur in a small percentage of people with psoriatic arthritis, says Rubenstein. To distinguish the two conditions, doctors will look at RF levels in the context of other factors, such as a certain pattern of joint involvement and symptoms of psoriasis, which can accompany psoriatic arthritis.
Frequency of Testing This is usually done only at the initial diagnostic appointment, says Rubenstein.
What Causes Psoriatic Arthritis
The cause of psoriatic arthritis is unknown. Researchers suspect that it develops from a combination of genetic and environmental factors. They also think that immune system problems, infection, obesity, and physical trauma play a role in determining who will develop the disease. Psoriasis itself is neither infectious nor contagious.
Recent research has shown that people with psoriatic arthritis have an increased level of tumor necrosis factor in their joints and affected skin areas. These increased levels can overwhelm the immune system, making it unable to control the inflammation associated with psoriatic arthritis.
Also Check: Is Shrimp Bad For Arthritis
How Do You Test For Psoriatic Arthritis
No single thing will diagnose psoriatic arthritis, but blood tests, imaging, and other tests can help your doctor. They may want to give you certain tests that check for rheumatoid arthritis, because it can look a lot like psoriatic arthritis.
Considering this, What blood tests show psoriatic arthritis? Blood tests for psoriatic arthritis
- Erythrocyte sedimentation rate .
How do you know if you have psoriatic arthritis? Know the Signs
Furthermore, Can a blood test diagnose psoriatic arthritis? There is no single blood test that can check for psoriatic arthritis , a chronic, inflammatory disease of the joints that can also cause a skin disorder called psoriasis. Your doctor will order a series of blood tests to check for different signs of psoriatic arthritis.
What Treatment Is Right For Me
The type of treatment will depend on how severe your symptoms are at the time of diagnosis with the goal being to control the disease to the point of remission and avoid complications. Medications may need to be changed over time to continue to maintain control and avoid disease progression and systemic effects. Some early indicators of more severe disease include onset at a young age, multiple joint involvement, and spinal involvement. Good control of the skin is important in the management of psoriatic arthritis. In many cases, you may be seen by two different types of healthcare providers, one in rheumatology and one in dermatology.
Early diagnosis and treatment can relieve pain and inflammation and help prevent progressive joint involvement and damage. Without treatment psoriatic arthritis can potentially be disabling, cause chronic pain, affect quality of life, and increase risk of heart disease. It is important to update your healthcare provider when you have a change in symptoms or if your medication regimen is no longer effective.
-
Learn about exercises, nutrition, safety tips and more.
Read Also: What Is The Treatment For Arthritis In The Neck
Psoriatic Arthritis Blood Test: Hla
HLA-B27 is a blood test that looks for a genetic marker for psoriatic arthritis a protein called human leukocyte antigen B27 , which is located on the surface of white blood cells. About 20 percent of people with psoriatic arthritis are positive for HBL-B27, according to CreakyJoints.
HLA-B27 is associated with a larger group of autoimmune diseases, called spondyloarthropathies, which includes psoriatic arthritis, Cadet says. These conditions can cause inflammation in the enthesis anywhere in the body but mainly in the spine.
If untreated over a long period, this inflammation may cause the destruction of cartilage, muscle spasms, and a decrease in bone mineral density that may lead to osteopenia or osteoporosis.
Frequency of Testing The HLA-B27 test is usually performed only at an initial visit to help establish a diagnosis, says Cadet.
Infectious And Reactive Arthritis
Infectious arthritis is an infection in one of your joints that causes pain or swelling. The infection can be caused by bacteria, viruses, parasites, or fungi. It can start in another part of your body and spread to your joints. This kind of arthritis is often accompanied by a fever and chills.
Reactive arthritis can occur when an infection in one part of your body triggers immune system dysfunction and inflammation in a joint elsewhere in your body. The infection often occurs in your gastrointestinal tract, bladder, or sexual organs.
To diagnose these conditions, your doctor can order tests on samples of your blood, urine, and fluid from inside an affected joint.
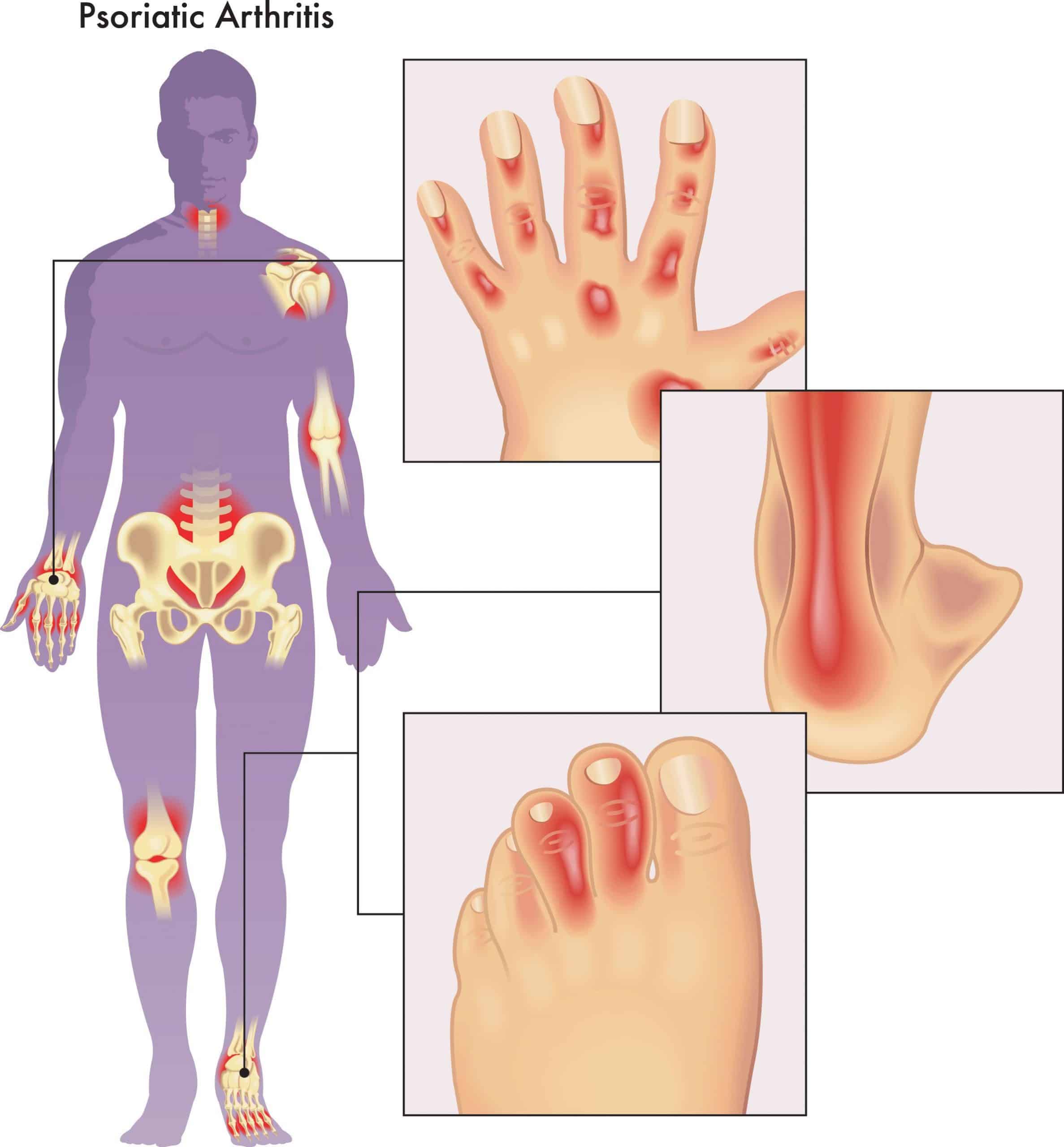
The fingers are most commonly affected with psoriatic arthritis , but this painful condition affects other joints as well. Pink-colored fingers that appear sausage-like, and pitting of the fingernails, may also occur.
The disease may also progress to your spine, causing damage similar to that of ankylosing spondylitis.
If you have psoriasis, theres a chance you could also develop PsA.
Don’t Miss: Is Keto Diet Good For Rheumatoid Arthritis
You Can Have Psoriasis And A Different Kind Of Arthritis That Is Not Psa
People with psoriasis can develop different types of arthritis including rheumatoid arthritis, gout, osteoarthritis, and reactive arthritis so diagnosing PsA involves ruling out those other conditions.
Its often difficult to say in a first visit whether a patient definitely has psoriatic arthritis or another type of arthritis that just co-exists with psoriasis, says Dr. Kumar. PsA can take a long time to diagnose because a patient can delay seeing the doctor, then confirming PsA can require multiple labs and imaging tests.
The good news is that the diagnosis process for psoriatic arthritis is improving. Whereas PsA wasnt even recognized as a distinct condition decades ago , doctors are now better equipped with improved lab tests and imaging studies that help identify this disease so more patients can find relief.
What Are The Symptoms Of Psoriatic Arthritis
The symptoms of psoriatic arthritis may be gradual and subtle in some patients in others, they may be sudden and dramatic. It may be mild, affecting only one joint or can be severe, affecting multiple joints. Not all patients experience all symptoms.
The most common symptoms of psoriatic arthritis are:
Joint symptoms
- Pain or aching, tenderness, and/or swelling in one or more joints – most commonly hands, feet, wrists, ankles, knees.
- Joint stiffness most notable in the morning or with prolonged inactivity such as sitting for a long time.
- Reduced range of motion in affected joints.
- Pain or stiffness in the lower back.
- Tenderness, pain, or swelling where tendons and ligaments attach to the bone , such as the Achilles tendon of the heel.
- Swelling of an entire finger or toe with a sausage-like appearance .
Skin symptoms
- Silver or gray scaly spots on the scalp, elbows, knees, and/or the lower spine.
- Small, round spots called papules that are raised and sometimes scaly on the arms, legs and torso.
- Pitting of the nails.
- Detachment or lifting of fingernails or toenails.
Other symptoms
Also Check: What Foods Can Help With Arthritis
Racial Disparities In Psa
Serious racial disparities exist when it comes to psoriatic arthritis severity and treatment. For example, Black people tend to have more severe:
- Skin involvement
- Psychological impact
- Impaired quality of life
Despite that, theyâre less likely than White people to be put on immunosuppressant drugsâthe preferred treatment for PsA.
Studies suggest psoriatic arthritis is diagnosed less often in:
- People of Asian descent
Disparities mean a higher disease burden and lower quality of life for people with PsA who are in these groups.
Some studies show implicit, often unconscious biases against people of color throughout the healthcare community. This is believed to negatively affect treatment decisions and outcomes.
Some facilities have found that poverty plays a role. But when comparing Black and White people of the same socioeconomic status, outcomes remained worse for Black people.
Researchers have called for more investigation into these disparities and their impact, as well as better education for eliminating bias.
Early Stages Of Psoriatic Arthritis
Recognizing the signs of psoriatic arthritis can be tricky since symptoms differ from patient to patient. For example, one person can experience psoriasis skin involvement and peripheral arthritis, another may experience axial disease , and someone else could have a combination of all three.
Whats more, especially during early disease, you may confuse your symptoms with other conditions. People can mistake enthesitis, inflammation of the entheses for tennis elbow or dactylitis for an infection, explains Dr. Mikulik.
If you have psoriasis and are having pain in your tendon and musculature and you think maybe Ive been too active lately, that may be the first sign of PsA, says Dr. Haberman. Doctors commonly hear people chalk up their symptoms to overuse, such as getting more exercise than usual or doing work around the house.
If you experience any of the following signs of early psoriatic arthritis its important to see your doctor as soon as possible:
Also Check: How To Relieve Arthritis Pain In Fingers
Recommended Reading: How To Heal Arthritis Naturally
Rheumatoid Factor Blood Test
Rheumatoid factor is a type of protein known as an autoantibody. Because RF targets the bodys own healthy tissues, elevated levels of the substance in the blood often indicate the presence of an autoimmune disease.
As its name suggests, a rheumatoid factor blood test is often used to screen for rheumatoid arthritis . During this test, your doctor will draw a small sample of blood usually from a vein in your arm and send it off for laboratory testing. Lab technicians will assess the levels of rheumatoid factor in your blood.
Positive RF test results indicate that your body is producing more rheumatoid factor antibodies than it normally would. Generally, the normal range for RF is between 0 IU/mL and 15 IU/mL. Mild elevation in the upper teens and 20s isnt usually a cause for concern. However, significantly higher rheumatoid factor results may indicate unusual autoimmune activity.
While doctors frequently order rheumatoid factor blood tests to confirm RA, the test can also indicate other RF-elevating diseases, such as cancer, Sjogrens syndrome, systemic lupus erythematosus , and sarcoidosis. That said, the test isnt perfect. According to the The United Kingdoms National Health Service, about one in 20 people without RA still receive positive RF results. Some may have one of the diseases mentioned above, while others may be healthy and simply have a high rheumatoid factor.
How To Prepare
Getting blood work usually is straightforward, but there are a few steps you can take to make sure the experience goes as smoothly as possible. If you’re allowed to drink water, keep yourself as hydrated as possible prior to the blood draw.
Some of the most common factors to consider before getting blood work include:
- Verifying if you need to fast for any of the tests ordered
- Reviewing with your physician your medications, including any vitamins, supplements, herbs, and drugs, in case they can affect test outcomes
- Thoroughly reading your patient care instructions
- If you struggle with medical, needle, or blood phobias, asking your doctor for advice on coping strategies and whether you can bring a support person to the clinic
- Asking questions or if theres anything else you should be aware of before leaving your appointment
Unless you are told to do so, dont make major dietary changes before getting blood work. Doing so could compromise the quality of the results, including by affecting comparisons between past and current results.
Recommended Reading: How Do You Develop Rheumatoid Arthritis
Why Have An X
X-rays and MRIs can show signs or features of psoriatic arthritis. These include:
- Asymmetric joint involvement, with joint changes on one side, as opposed to symmetrical, or both-sided, joint involvement with rheumatoid arthritis
- Distal joint involvement, including changes in the joints closest to the nail of the fingers or toes
- Entheseal involvement, meaning “insertion” in Greek, “entheseal” here refers to any attachment site like a tendon or ligament to a bone
- Asymmetrical spinal involvement, a curvature to one side of the spine, as opposed to the symmetrical involvement in the autoimmune disease ankylosing spondylitis
- Pencil-in-cup deformity, when the finger looks like a sharpened pencil and the adjacent bone has been worn down into a cup-like shape
Inflammation And Other Forms Of Arthritis
Some infections can lead to joint destruction and this occurs much quicker than with other forms of arthritis. It is crucial to rule out an infection when arthritis affects a single joint.
Gout: A common and painful condition that affects the joints and tendons. Small crystals of uric acid form in and around the joint which causes inflammation, pain and swelling. An attack of gout usually comes on very quickly, often overnight. The joint becomes red, swollen and painful. It often affects one joint at a time, such as the big toe.
Inflammation: A localised physical condition in which part of the body becomes reddened, swollen, hot, and often painful. Inflammation is a common symptom of arthritis, and is the cause and the result of all forms of arthritis.
This info sheet was reviewed and updated by Prof. Susanna Proudman, Medical Director, Arthritis Australia and Dr Stephen Adelstein, Pathology Awareness Australia ambassador.
Donât Miss: Whatâs The Difference Between Gout And Arthritis
Also Check: What Vitamin Supplement Is Good For Arthritis
Differences Of Ra And Psa
RA is an autoimmune systemic inflammatory disease characterised by synovitis, bony erosions and cartilage damage. PsA is a heterogeneous autoimmune systemic disease with diverse clinical and radiographic manifestations. The presence of psoriasis precedes the development of PsA in 85% of patients, and PsA typically develops about 10 years after the onset of psoriasis. Other common clinical features of PsA include synovitis with subsequent osteolysis and/or joint fusion of peripheral joints, axial involvement, sacroiliitis, and extra-articular manifestations, including nail dystrophy, enthesitis and dactylitis not all are present in every patient. Key clinical, serological and radiographic differences between RA and PsA are summarised in .
Clinical, serological and radiographic characteristics of PsA and RA
Treatments For The Arthritis
Non-steroidal anti-inflammatory drugs
NSAIDs, or non-steroidal anti-inflammatory drugs, can reduce pain, but they might not be enough to treat symptoms of psoriatic arthritis for everyone.
Some people find that NSAIDs work well at first but become less effective after afew weeks. If this happens, itmight help to try a different NSAID.
There are about 20 different NSAIDs available, including ibuprofen, etoricoxib, etodolac and naproxen.
Like all drugs, NSAIDs can have side effects. Your doctor will reduce the risk ofthese, by prescribing the lowest effective dose for the shortest possible period of time.
NSAIDs can sometimes cause digestive problems, such as stomach upsets, indigestion or damage to the lining of the stomach. You may also be prescribed a drug called a proton pump inhibitor , such as omeprazole or lansoprazole, to help protect the stomach.
For some people, NSAIDs can increase the risk of heart attacks or strokes. Although this increased risk is small, your doctor will be cautious about prescribing NSAIDs ifthere are other factors that may increase your overall risk, for example, smoking, circulation problems, high blood pressure, high cholesterol, or diabetes.
Some people have found that taking NSAIDs made their psoriasis worse. Tell your doctor if this happens to you.
Steroid treatment
Steroid injections into a joint can reduce pain and swelling, but the effects do wear off after a few months.
Disease-modifying anti-rheumatic drugs
Don’t Miss: What Foods Are Anti Inflammatory For Arthritis