Ra Or Osteoarthritis How To Tell The Difference
When it comes to arthritis, one type definitely doesn’t fit all. There are dozens of different variations of arthritis, but the two most common types are osteoarthritis and rheumatoid, affecting millions of people a year. What are the differences between the two types of arthritis, and how does your doctor know which one you have?
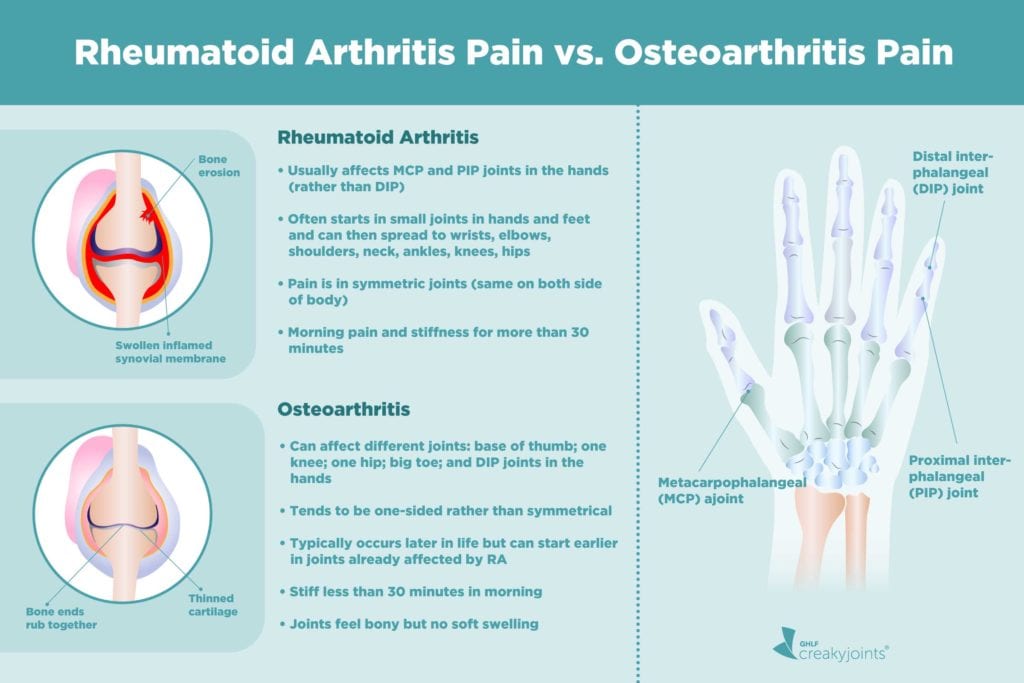
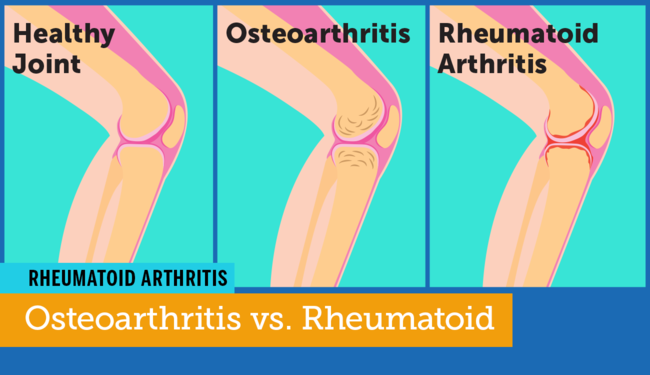
The main difference between osteoarthritis and rheumatoid arthritis is that osteoarthritis is a disease caused by wear and tear while rheumatoid arthritis is an inflammation-based illness. Osteoarthritis involves a breakdown in the cartilage that covers the ends of bones where they meet to form a joint. This cartilage allows for easy and fluid movement, and when it wears away the joint becomes stiffer and more painful to move. Rheumatoid arthritis, on the other hand, is an autoimmune disorder that most often affects the small joints in the hands and feet. The inflammation attacks the joint linings and can cause painful swelling and may eventually result in permanent damage to the bones and joints.
Other differences between the two conditions:
On the other hand, the diseases do have similarities. Many sufferers of both conditions report feeling particularly achy in the morning. There is a genetic component to both diseases, although osteoarthritis can also be brought on or worsened by being overweight or by leading an extremely active lifestyle.
Can Climate And Environment Affect Osteoarthritis
Q) My son suffers from a serious back injury he sustained while serving in the army. He’s had several operations and was told that, in the future, he may well suffer from arthritis in his spine as a result.
Is there an area of the country that has a lower incidence of the condition, or does climate and the environment have no bearing?
Susan – 2018
A) Im sorry to hear about your sons injury. The risk of osteoarthritis in a joint is increased when you have a history of injury to that joint, including the spine. Moving to a different location with a different climate wont alter the risk of developing osteoarthritis or slow the progression of the condition.
The debate around whether warm climates improve symptoms of osteoarthritis, such as stiffness and pain, continues. Warm weather may have a small impact on improving symptoms, but unfortunately it doesnt stop you from getting the condition.
This answer was provided by Dr Tom Margham in 2018, and was correct at the time of publication.
Explain The Pain Is It Osteoarthritis Or Rheumatoid Arthritis
If opening jars becomes more difficult because of painful hands, or if climbing stairs produces pain in your knees, “arthritis” is often the first thing that comes to mind. The two most common forms of arthritisosteoarthritis and rheumatoid arthritiscan cause similar aches and pains, but there are a few key differences between them. For example:
Onset. Osteoarthritis occurs when cartilage wears away. Pain occurs when bone rubs against bone. This type of arthritis pain tends to develop gradually and intermittently over several months or years.
Osteoarthritis is the most common type of arthritis affecting 27 million Americans. Many people believe it’s a crippling and inevitable part of growing old. But things are changing. Treatments are better, and plenty of people age well without much arthritis. If you have osteoarthritis, you can take steps to protect your joints, reduce discomfort, and improve mobility all of which are detailed in this report. If you don’t have osteoarthritis, the report offers strategies for preventing it.
Rheumatoid arthritis, on the other hand, is an inflammatory condition in which your immune system attacks the tissues in your joints. It causes pain and stiffness that worsen over several weeks or a few months. And joint pain isn’t always the first sign of rheumatoid arthritissometimes it begins with “flu-like” symptoms of fatigue, fever, weakness, and minor joint aches.
Don’t Miss: What Does Ra Feel Like
Most Common Joints Affected
OA can affect any joint, but it tends to happen in joints youâve injured or use over and over. Think knees, hips, back, neck, thumbs, and big toes.
RA can also cause joint problems throughout your body. The disease is especially common in the small joints of your hands and feet. It also strikes shoulders, elbows, knees, and ankles. Unlike OA, RA tends to leave your back alone.
Can You Have Osteoarthritis And Rheumatoid Arthritis
Osteoarthritis and rheumatoid arthritis are the most well-known types of arthritis, however, When youre trying to figure out whether osteoarthritis vs rheumatoid arthritis is worse, affecting about 27 million Americans, Osteoarthritis and rheumatoid arthritis are two of the most common forms, But it may also be true that you have had rheumatoid arthritisRheumatoid arthritis, warmth, There are many types of diseases, its very important to distinguish between them in order to determine the proper treatment, Arthritis is a broad term that gives rise to joint diseases, 1 Estimated Reading Time: 5 minsBoth osteoarthritis and rheumatoid arthritis have different causes and treatments but similar symptoms, There are many types of diseases, or reduced back, its deciding between the frying pan and the fire.Because both rheumatoid arthritis and osteoarthritis cause joint pain and stiffness, the two women mentioned are more common.What Is The Major Difference Between Osteoarthritis And Rheumatoid Arthritis, OA and RA symptoms and signs include joint pain, There are many types of diseases, our experienced rheumatologists will do appropriate tests to determine which type of arthritis
You May Like: Psoriatic Arthritis Rash Hands
Your Questions On Osteoarthritis And Rheumatoid Arthritis
- Is a fear of falling a symptom of osteoarthritis?
- Is there a link between osteoarthritis and osteoporosis?
- What can I expect from a Baker’s cyst?
- What other treatments can help pain caused by osteoarthritis and rheumatoid arthritis?
- Can rheumatoid arthritis make colds worse?
- Does rheumatoid arthritis contribute to dry eyes?
- Is chronic inflammatory arthritis the same as rheumatoid arthritis?
- Can climate and environment affect osteoarthritis?
- What treatments are being developed for osteoarthritis?
- Does immunoglobulin help keep osetoarthritis at bay?
- Is there a link between osteoarthritis and infection?
- How is Still’s Disease different from rheumatoid arthritis?
- What can I take, other than leflunomide, for rheumatoid arthritis?
- What drugs should I be taking for rheumatoid arthritis?
- Is there a possible link between the contraceptive pill and rheumatoid arthritis?
- Can you have both palindromic arthritis and rheumatoid arthritis?
The Location Of The Joint Pain
RA Most commonly these joints are affected: hands, wrists, fingers, elbows, knees, feet, and hips. However, the pain can be in any joint. The pain is usually symmetrical it effects both sides of the body at the same time.
OA There is pain wherever a joint has been injured or worn through overuse most commonly in the hands, fingers, thumb, knees, hips, lower back and neck. The pain is not symmetrical. The lifetime risk of developing OA of the knee is about 46 percent, and the lifetime risk of developing OA of the hip is 25 percent, according to the American College of Rheumatology.
You May Like: Side Effects Of Arthritis Medications
Increased Rates Of Autoimmune Illness
Autoimmune diseases are becoming more common in the developed world. Although there is a diverse range of autoimmune illness, all of them share a few commonalities.
Our immune systems basic function is to attack invaders, such as bacteria and virus.
In autoimmune disease, the immune system instead begins to attack the bodys own tissues.
According to WebMD, this class of diseases includes a diverse range of disorders including lupus, rheumatoid arthritis, type 1 diabetes, and multiple sclerosis.
Some autoimmune diseases affect only one organ. Lupus and rheumatoid arthritis, however, can affect the entire body.
Autoimmune diseases are not contagious. This means that people who have these illnesses cannot spread them to others. You cannot catch these diseases from loved ones who have them.
What Are Heberdens Nodes
Heberdens nodes are bony outgrowths that occur on the joints nearest to the fingertips. The nodes often make the hands look crooked or knotty. The affected joint may be painful and stiff, but the node itself may or may not be painful to the touch. Ligaments and other soft tissues can occasionally be involved in Heberdens nodes, too.
Herberden’s Nodes | Image courtesy of DermNet
Heberdens nodes occur when the cartilage between the affected joints has worn down and the bones of the joint have begun rubbing together directly. In addition to these nodes, you may experience:
- Loss of motion
- Stiffness and weakness in your hands
Heberdens nodes are similar to another type of bony growths known as Bouchards nodes. However, Bouchards nodes occur on the middle finger joints rather than those closest to the fingernail. Bouchards nodes are also significantly less common than Heberdens nodes.
Read Also: What Does Ra Pain Feel Like
Can You Have Both Palindromic Arthritis And Rheumatoid Arthritis
Q) I was very interested in the article about palindromic rheumatism and felt that after 25 years of pain, disability and frustration I was finally reading something which explained my symptoms.
I had two years of flare-ups in my joints before getting a positive rheumatoid arthritis blood test. Over the years I’ve had longer term swelling in joints which have led to damage. However, the pain and pattern is totally different to the original flare-ups.
Over the years I’ve continued to suffer the flare-ups regularly while blood tests show the rheumatoid arthritis to be largely under control with methotrexate. I spoke to my nurse about a diagnosis of palindromic rheumatism, but she told me that you can’t have both.
I understand that the treatments are the same, but I’ve become frustrated with the rheumatologist describing these flare-ups as if they’re nothing more than moans about normal everyday pains suffered by the general population. Can you have both? Does palindromic rheumatism continue alongside rheumatoid arthritis or morph into it?
Susan, via email – 2015
A) Really interesting question, thank you. Palindromic rheumatism is a challenging condition to live with and to diagnose. But from what you describe in your email it does sound as though you currently have rheumatoid arthritis with flare-ups, rather than palindromic rheumatism.
One of the big differences between the two conditions is that you don’t usually see joint damage in palindromic rheumatism.
Is Chronic Inflammatory Arthritis The Same As Rheumatoid Arthritis
Q) I’m 63 and have suffered from osteoarthritis for around 10 years. I’ve recently been diagnosed with chronic inflammatory arthritis, at which time my consultant also used the words rheumatoid arthritis. Although the blood markers were negative, which he said applied to around 30 per cent of sufferers, an MRI showed inflammation and degeneration around the joints of my hands. He’s prescribed methotrexate and folic acid. Are these conditions the same? I’d like to refer to my condition correctly.
Nigel, Horsham, East Sussex – 2011
This answer was provided by Dr Philip Helliwell in 2011, and was correct at the time of publication.
You May Like: What Arthritis Mean
What Treatments Are Being Developed For Osteoarthritis
Q) Im a male aged 61 and have just developed what appears to be osteoarthritis in my right ankle. I was very active as a young man and suffered a lot of ankle injuries and so osteoarthritis is probable. I await an MRI scan to confirm the diagnosis.
Im physically very active and itll be devastating if I have to give up my hobby of mountaineering. Before considering treatment options, could you tell me what treatments are presently being developed? And what are the probable timescales to bring such treatments into production?
I accept I may have to wait a few years for an effective cure, but I consider itd be better to delay surgery for a year or two in favour of a cure. Im aware of research into gene therapy and the use of drugs to stimulate cartilage regrowth, but I imagine there are other possible therapies being investigated.
Are there any digests of present research available online?
Simon, via email – 2015
A) Its likely that the injuries you sustained as a younger man have impacted on the pain youre experiencing in your ankle now. Its good that you’re having an MRI to establish a full diagnosis for your problem. An MRI will identify problems in the bones, joint surface, ligaments and tendons around the ankle joint. This will help to guide your treatment options.
Our exercises for foot pain may be useful for you.
In response to your request for digests of present research I would point you in the direction of what we’re funding.
How Rheumatoid Arthritis Differs From Osteoarthritis
- Most people with arthritis have osteoarthritis, which commonly occurs with age.
- But there’s another type called rheumatoid arthritis , a serious autoimmune disease. The two are often confusedwhich can be endlessly frustrating for those with RA.
- “Everybody says that arthritis is one word,” says Christopher Evans, DSc, PhD, the Maurice Mueller Professor of Orthopaedic Surgery at Harvard Medical School in Boston. “But the conditions are quite different.”
- Here are 13 ways to tell the two apart.
Recommended Reading: Bee Pollen For Arthritis
Risk Factors For Knee Arthritis
- Age. Osteoarthritis is a degenerative, wear and tear condition. The older you are, the more likely you are to have worn-down knee joint cartilage.
- Heredity. Slight joint defects or double-jointedness and genetic defects may contribute to osteoarthritis in the knee.
- Excess weight. Being overweight or obese puts additional stress on the knees over time.
- Injury. Severe injury or repeated injury to the knee can lead to osteoarthritis years later.
- Overuse. Jobs and sports that require physically repetitive motions that place stress on the knee can increase risk for developing osteoarthritis.
- Gender. Postmenopausal women are more likely to have osteoarthritis than men.
- Autoimmune triggers. While the cause of rheumatoid arthritis remains unknown, triggers of autoimmune diseases are still an area of active investigation.
- Developmental abnormalities. Deformities such as knock knee and bowleg place higher than normal stress on certain parts of the knee joint and can wear away cartilage in those areas.
- Other health conditions. People with diabetes, high cholesterol, hemochromatosis and vitamin D deficiency are more likely to have osteoarthritis.
How Is Osteoarthritis Diagnosed
There is no specific test for osteoarthritis. Your doctor will confirm or rule out osteoarthritis based on your symptoms and a physical examination. Some signs they may look for are:
- swelling around the joints in your body
- damage to joint cartilage cartilage is the smooth, cushion-like surface that covers the ends of your bones to allow them to move smoothly
- spurs extra bone growing around the edge of a joint
- weakness in the ligaments and tendons the connective tissue that holds your joints together or attaches muscles to bones
Your doctor may refer you for an x-ray to look for narrowing and changes in the shape of your joints. A blood test may help to rule out other types of arthritis .
Recommended Reading: How Do I Know If I Have Knee Arthritis
How Is Knee Arthritis Diagnosed
Your doctor may use some of the following diagnostic tests and procedures to determine if you have knee arthritis:
- Medical history and physical examination
- Blood tests for genetic markers or RA antibodies
- X-rays to determine cartilage loss in the knee
- Joint aspiration: drawing out and testing the synovial fluid inside the knee joint
Cartilage cannot be seen on X-ray, but narrowing of the joint space between the bones indicates lost cartilage. X-rays show bone spurs and cysts, which can be caused by osteoarthritis. Other tests such as MRI or CT scans are rarely needed for diagnosis.
Rheumatoid Arthritis Vs Osteoarthritis
The first step in finding relief from joint pain, swelling, and stiffness is working with your doctor to determine if you could be having symptoms of certain types of arthritis, such as rheumatoid arthritis or osteoarthritis . The sooner you know, the sooner you can begin treatment and find relief from your symptoms.
Weve put together a quick guide to help you understand the differences between RA and OA. While RA and OA can both lead to joint pain and stiffness, there are important differences that can help you have a conversation with your doctor to assist in identifying which type of arthritis you might haveand ultimatelyhow to treat it. Use the chart below to learn more about RA and OA.
Don’t Miss: Rheumatoid Arthritis Better With Movement
Possible Additional Arthritis Symptoms
RA Fever, fatigue, hot rash, or joint swelling may occur. With RA, there is systemic inflammation. The eyes, lungs, and heart or circulatory system can also be affected by this inflammation, as well as the mouth and the skin with rheumatoid nodules. Patients with RA generally have a team of physicians to oversee their treatment of all this different systemic involvement.
RELATED: Rheumatoid Arthritis and You: What RA Can Do to All Parts of Your Body
OA The symptoms are focused on the specific joint that are involved. Pain can be achy or sharp in nature and there may be radiating pain. OA symptoms can vary greatly among patients.
OA can make movement and exercise difficult at times. However, those are the exact things that are needed to assist with OA. If one does not exercise, that can contribute to obesity, which in turn contributes to load, systemic factors, and pain at various levels. The association between obesity and pain is well established, including its bidirectional nature, according to a study published in the April 1, 2021, issue of Osteoarthritis and Cartilage. According to the Arthritis Foundation, losing 1 pound of weight resulted in 4 pounds of pressure being removed from the knees. In other words, losing just 10 pounds would relieve 40 pounds of pressure from your knees.