Stomach Pain Or Indigestion
RA and medicines used to treat it are linked to mouth and stomach ulcers, stomach bleeding, acid reflux, diarrhea, and constipation. Painful diverticulitis and colitis are also possible if you have RA.
RA drugs like NSAIDs often cause ulcers or an upset stomach.
Belly pain is sometimes a sign of a rare RA complication called rheumatoid vasculitis when inflammation spreads to your blood vessels. Weight loss and lack of appetite are other symptoms. Vasculitis is serious, so see a doctor right away. Learn more about vasculitis symptoms and types.
What Is Rheumatoid Arthritis
Rheumatoid arthritis is a chronic inflammatory disorder that can affect your joints and other body systems. It occurs when your immune system attacks your bodys tissues instead of those of outside invaders.
Outside of the joints, rheumatoid arthritis can affect the skin, eyes, lungs, heart, kidneys, salivary glands, nerve tissue, bone marrow, and blood vessels. It presents itself mainly in the form of swollen, tender, or stiff joints as well as fatigue, fever, or loss of appetite.
Ra And Periodontal Disease: What’s The Link
Rheumatoid arthritis and gum disease are seemingly unrelated conditions. But research shows that the two have certain bacteria in common. These germs â including P. gingivalis and Aggregatibacter actinomycetemcomitans â can trigger both periodontal disease and the inflammation found in RA.
One study found that if you have RA, you are twice as likely to have gum disease as those without it. Another study found that 65% of people with RA also had gum disease, compared to only 28% of people without RA. In both studies, experts found that the severity of periodontal disease was also worse in people with RA.
Recommended Reading: How Does Rheumatoid Arthritis Affect Your Skin
What Should People With Rheumatoid Arthritis Do About Oral Health
Patients with rheumatoid arthritis should try to reduce bacteria and tooth decay in the mouth by eating healthier foods, especially those with a lower sugar content. Make a regular dental appointment to address any concerns. If you are having trouble with caring for your teeth due to stiffness and joint pain, consult a rheumatologist to create a proper care plan.
May 29, 2009. Case Western Reserve University. Treating Gum Disease Helps Rheumatoid Arthritis Sufferers Summary: Not yet convinced about keeping your teeth healthy, heres another reason. People who suffer from gum disease and also have a severe form of rheumatoid arthritis, reduced their arthritic pain, number of swollen joints and the degree of morning stiffness when they cured their dental problems.
Infection Of The Pulp Of A Tooth
Infection of the pulp of the tooth is one of the causes of desmodontitis. A tooth pulp infection can be caused by tooth decay.
Tooth decay is a bacterial pathology. Bacteria can spread into the periodontal muscle. All these toxins can cause dental arthritis.
Inflammation of the dental ligament is caused by necrosis of the pulp tissue, and by dead microorganisms.
Recommended Reading: What Foods Cause Inflammation Arthritis
Whats The Link Between Ra And Periodontal Disease
Researchers discovered that RA might not start in your joints. Instead, data shows that the inflammatory disease might happen due to autoantibodies â antibodies that react with your own body, instead of infections â made in other parts of your body .
The microbes in your mouth create autoantibodies. This happens because a type of bacteria in your mouth, called P. gingivalis, contains peptidyl-arginine deiminase , an enzyme that changes proteins in your body. Once this change occurs, your body sees the proteins as a threat. Experts call this process âcitrullination.â It can lead to the creation of antibodies against proteins in the lining of your joints. Citrullination causes proteins to be more likely to cause an immune response that harms this joint lining.
Experts found bacteria from your mouth in the fluid between your joints in people with RA and other forms of arthritis. They believe that the bacteria moves through damaged gum tissue, enters into your bloodstream, and then escapes to other parts of your body.
P. gingivalis can lead to earlier onset, quicker progression, and more intense RA. Because of this, your bones and cartilage could become more damaged.
But itâs still not clear whether one condition directly leads to the other. Instead, experts have two major theories on how RA and periodontal disease affect each other:
Oral Health And Inflammatory Diseases
Postdoctoral research fellow Malini Moni, BDS, MS shares information and tips about common oral health problems seen in patients living with rheumatic diseases. Pain from these autoimmune diseases can make it difficult for some people to brush or floss their teeth.
A study conducted at the Johns Hopkins Arthritis Center found that gum disease and tooth loss are more prevalent in people who have rheumatoid arthritis . Another syndrome that is known to hinder oral health is Sjögrens syndrome. This syndrome can be seen in people who have rheumatic diseases.
Don’t Miss: What Not To Eat With Gouty Arthritis
Iv Treatment Of Dental Arthritis
The treatment of dental arthritis is first and foremost the treatment of the cause of arthritis. If the arthritis is related to an infectious cavity or inflammation of the teeth, then the condition must be treated first.
Antibiotics will be prescribed if an infection has caused the inflammation of the teeth.
To fight pain, anti-inflammatory drugs are usually prescribed. This is a way to act, but only on the symptoms of dental arthritis.
Apart from that, painkillers and anti-inflammatory drugs should be taken for 5 days.
What Are Symptoms Of Ra And Periodontal Disease
Studies show that symptoms and other factors of periodontal disease are more intense in people who also have RA. Similarly, there is usually more P. gingivalis in your body right before your RA symptoms begin to show.
The severity of your periodontal disease is often in line with the activity of your RA. This means that if your RA is more active, itâs likely that your periodontal disease will also worsen.
Recommended Reading: What Not To Eat When You Have Arthritis Rheumatoid
How Are Autoimmune Diseases Linked To Hearing Loss
Not all autoimmune disorders affect hearing, but many of them do. Often the hearing damage is related to harmful inflammation in the delicate ear anatomy, or disrupted blood flow to the ear. The severity of the hearing loss can vary. Depending on the underlying disease, it can affect one or both ears, may develop suddenly or slowly, and may affect different frequencies .
Given how complex both hearing and the immune systems are, its not always possible to know what role an autoimmune disorder played in hearing loss. Autoimmune disorders can flare up and then go into remission, and a person may not ever realize the link to their hearing loss.
In many cases, though the hearing loss is permanent, the cause of the damage can be transitory, so theres no way to diagnose the cause of the damage after it has happened, explained Aaron Abend, executive director of the Autoimmune Registry, Inc.
Treatment may include corticosteroids that limit blood vessel inflammation and the immune attack on the inner ear. For some autoimmune diseases, plasma transfers can clear the antibodies that attack phospholipids from the blood. Other treatments increase blood flow to the inner ear or suppress the immune system. When the hearing loss is permanent, hearing aids may be recommended.
What Is The Tmj
The TMJ is the temporomandibular jointyour jaw. This joint is responsible for opening and closing your mouth, a very important task! This everyday bodily function can be disrupted by TMJ disorder, teeth grinding, and even rheumatoid arthritis. Keeping your TMJ well-oiled is crucial to a pain-free life.
Also Check: Are Certain Foods Bad For Arthritis
Periodontal Care In Prescott Arizona
Rheumatoid arthritis is a painful and difficult diagnosis to deal with, but dedicated dental care can help prevent some of the negative side effects. Because rheumatoid arthritis affects your gums and teeth, you need a dentist that specializes in periodontal care. The experts at Prescott Dentistry can help you protect your mouth and prevent gum diseaserequest an appointment online or call us at today.
Can Rheumatoid Arthritis Lead To Dental Problemsby Bruce Wilderman On September 01 2016
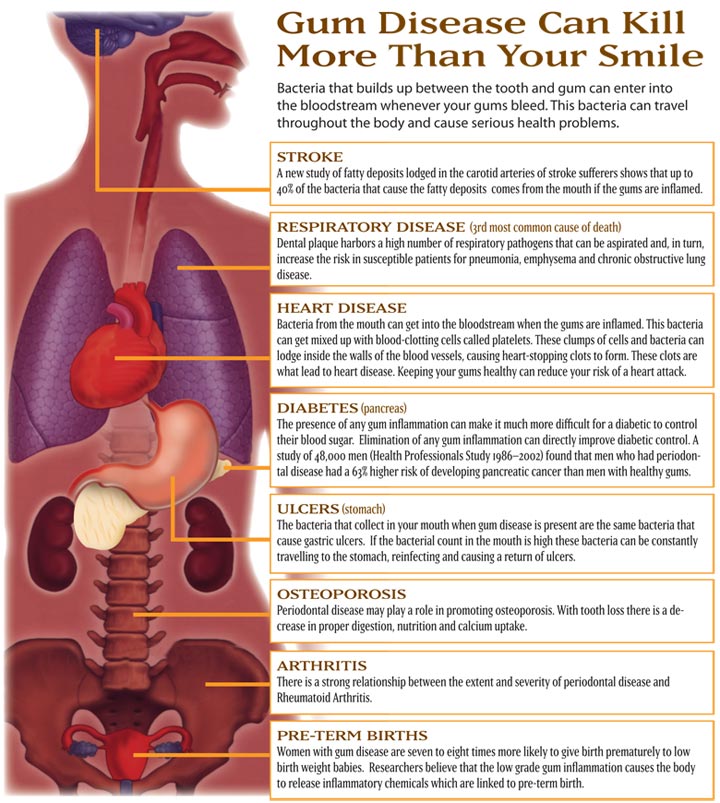
Rheumatoid arthritis is a condition that is the result of an overactive immune system. This disease causes inflammation around the joints, which can cause them to become swollen and stiff. When rheumatoid arthritis flares up, movements can be limited and painful. Unfortunately, studies show that the effects of rheumatoid arthritis can actually impact the entire body, including the mouth. Patients with rheumatoid arthritis are far more likely to suffer from gum disease, an inflammatory condition that causes swelling in the gums. Because of this link, general dentistry services to monitor and preserve oral health are vitally important to rheumatoid arthritis patients. Dr. Bruce Wilderman discusses the link between dental problems and rheumatoid arthritis with his Philadelphia, PA patients and offers some tips for minimizing the risk of oral health complications.
Also Check: What Drugs Are Used For Rheumatoid Arthritis
How To Alleviate The Symptoms
In a 2009 study, researchers found that when people with severe RA treated their gum disease, some of the side effects of RA they were experiencing greatly improved. You can stay on top of your oral health by brushing and flossing regularly and avoiding tobacco products. Be sure to see your dentist regularly and inform him or her about your RA and any new oral health issues.
Dental Care Tips For Ra Patients
One of the unfortunate effects of rheumatoid arthritis is that swollen joints can make it more difficult to perform daily tasks, including routine dental care. Swelling around the joints of the hands can compromise a patients grip and make brushing and flossing more difficult. Below are some tips that rheumatoid arthritis patients can use to make oral hygiene practices easier:
- Use an electric toothbrush, which offers maximum power with minimal effort
- If it is difficult to grip a toothbrush, consider alterations, such as a tennis ball on the base of the brush
- Use floss holders or floss picks
- Consider using a toothpaste that comes in a pump container, rather than a tube
- Use a mouthwash for extra protection against cavities
You May Like: What Causes Rheumatoid Arthritis Flare Ups
Can Rheumatoid Arthritis Affect Your Teeth
Can rheumatoid arthritis affect your teeth? What is dental arthritis ? What causes dental arthritis? The symptoms? The treatments? What is the link between dental arthritis and a devitalized tooth? What natural treatments can be used to relieve dental arthritis? And finally, how to prevent dental arthritis?
Does Sjogrens Affect Ears
3.9/5Earhearing
Likewise, can Sjogrens cause hearing loss?
Individuals with sjogrens syndrome often complain of ringing in the ears, mild hearing loss, or ear pain which is caused by inflammation of the nasal cavity blocking the Eustachian tube. *Rheumatoid arthritis is a chronic inflammatory disorder that affects mostly your joints. Some people complain of hearing loss.
Secondly, can autoimmune disease cause ear infections? Autoimmune inner ear disease , is a rare disease that happens when your bodys immune system mistakenly attacks your inner ear. It can cause dizziness, ringing in your ears, and hearing loss. Less than 1% of the 28 million Americans who have hearing loss have it because of AIED.
Besides, can rheumatoid arthritis affect your ears?
If you have rheumatoid arthritis, theres a chance youre at an increased risk for ear problems such as varying levels ofhearing loss as well as autoimmune inner ear disease. Not only that, but RA can also affect the teeny, tiny bones, joints, and even the cartilage contained within the ear.
What are the symptoms of autoimmune inner ear disease?
Signs and symptoms of AIED are:
- Progressive hearing loss in both ears. Typically will begin in one ear and gradually affect the other.
Also Check: Can Rheumatoid Arthritis Affect The Jaw
New Treatments Are On The Horizon
Ideally, once specific bacteria are identified as triggers for gum disease and rheumatoid arthritis, doctors may be able identify people at risk for RA based on their teeth and treat them before symptoms even occur. Interfering with oral health might actually improve overall health in terms of RA, Dr. Konig explains. If you were to start aggressive periodontal treatment to get rid of the bacteria, maybe you could prevent them from developing the other disease. Keeping gums healthy plus preventing the progression of joint pain: Now thats getting your moneys worth!
It’s On You To Stay On Top Of Your Heart Health
Despite the higher risk, there are no firmly established guidelines for cardiovascular screening for people with RA. An awareness of a higher risk of cardiovascular disease is important, and usual screening for CVD is advised, but there are no current recommendations that all RA patients should have specific CVD testing guided by a cardiologist, says lead study author Jon T. Giles, MD, associate professor of medicine at Columbia University in New York City.
Also Check: What Can Be Done For Arthritis In Lower Back
What Causes Autoimmune Diseases
The precise cause of autoimmune diseases is unknown. However, there are risk factors that may increase your chances of getting an autoimmune disease. Risk factors include:
- Some medications. Talk to your healthcare provider about the side effects of medications for blood pressure, statins and antibiotics.
- Having relatives with autoimmune diseases. Some diseases are genetic they run in families.
Also Check: Can You Get Rheumatoid Arthritis In Your Back
What Triggers Ra Dental Issues
I called my rheumatologist when I returned home and informed him of what had happened at the dentist. He said that it was possible that both the Humira and Plaquenil were indirect sources of my recent teeth troubles. The rationale behind this was that these medications were causing dry mouth and subsequently leading to a proliferation of bacteria, which thereby created the beginnings of those cavities.
Recommended Reading: Does Psoriatic Arthritis Show Up On Xray
Study Design Participant Recruitment And Data Collection
| As a person with arthritis . . . How do you feel about the state of your mouth health? Do you feel that the health of your mouth is good? Do you have any problems with your mouth? Do you think your arthritis affects your overall mouth health? Does your mouth health affect your arthritis? In what ways? | |
| Affect of arthritis on oral care | Does your arthritis affect your mouth care? How?Is there anything that makes it hard to care for your mouth? What helps with caring for your mouth care?Is there anything that makes it hard to seek dental care for your mouth? What helps? |
| Educational needs relating to oral health | What do you think about the aims of having information on mouth care that include recommendations for everyone but also include suggestions specific for people with arthritis?What type of information would you like to know?How do you usually get information about your arthritis, and how would you like to get information about your arthritis or mouth care?What format would be most helpful? Paper handouts, words, or pictures. From your doctors/dentists? From the internet? Do you connect with other people using Facebook or other types of social media? |
| Priority oral health concerns | Of all the things weve discussed today, what would you say are the most important issues you would like to share about arthritis and mouth concerns? |
Oral Health And Rheumatoid Arthritis: A Complex History
Doctors and researchers have long noted a link between poor oral health and rheumatoid arthritis. It was clearly noted that rheumatoid arthritis sufferers tended to have increased instances of periodontal disease. This, many assumed, was either because the crippling effects of RA made thorough oral hygiene difficult or that medications used to treat RA inhibited the body’s ability to fight oral bacteria and decay. Additionally, Sjögren’s Syndrome with RA stopped patients from being able to produce saliva a natural line of defence in the fight against gum disease.
However, Jerry A. Molitor, MD, PhD, associate professor in the rheumatic and autoimmune disease division of the department of medicine at the University of Minnesota, Minneapolis says the relationship is proving to be more complicated.
While research is yet to prove cause and effect, it’s starting to become obvious periodontal disease doesn’t always trail RA, sometimes it precedes it, says Dr. Molitor.
Dr. Molitor’s own study was presented to the 2009 scientific meeting of the American College of Rheumatology in 2009. It found people with serious gum infection who also tested positive for anti-CCP antibodies were more likely to have moderate to severe gum disease and be a smoker. Smoking is a risk factor for both periodontitis and rheumatoid arthritis. Dr. Molitor’s findings suggest RA could cause bacteria or, alternatively, that pre-existing gum disease could perhaps be triggering RA instead.
Also Check: How Many Mg In Tylenol Arthritis
Getting To The Root Of It: The Ra And Dental Health Connection
According to medical research conducted by John Hopkins and others, there is a much higher prevalence of gum disease and tooth loss among people with RA than other healthy individuals. High levels of inflammation are present in both RA and periodontal disease, and while medical experts arent sure which occurs first, one disease negatively impacts the other. And just as inflammation causes bone erosion and soft tissue damage in the rest of the body, it impacts the jaw and mouth as well.
If someone with RA also suffers from Sjogrens Syndrome as well, that complicates things further because inflammation of the salivary glands can cause dry mouth, speeding up the process that can cause gum disease and tooth loss.
Other Causes Of Tmj Pain
- Jaw Injury acute trauma to your jaw and the muscles surrounding it is one of the leading causes of TMJ pain. The injury could be due to accidents, including slips, falls, and vehicle accidents.
- Genetics if any of your parents or close relatives have TMJ pain, you are most likely to also suffer from it as you age.
- Poor Posture maintaining a poor posture can have a lot of adverse effects on your body. Having TMJ pain can be a result of it. The joints on your jaw are very finely balanced, and poor posture can cause them to misalign, lock, or cramp. This increases your risk for pain.
- Arthritis psoriatic arthritis, osteoarthritis, and rheumatoid arthritis
You May Like: How Do X Rays Show Arthritis
Recommended Reading: How Do Doctors Know If You Have Rheumatoid Arthritis